Unit Three — Abdominal Organs, Pelvis & Lower Limb
Abdominal Organs
Meghan Cotter, PhD
Chapter Section
Abdominal Organs
Gastrointestinal Tract and Associated Organs
Learning Objectives
- Locate the thoracoabdominal diaphragm and identify the three major foramina within it.
- Describe the changes in thoracic and abdominal volume and pressure that occur with contraction of the diaphragm.
- Describe the relative positions and general functions of the organs within the abdomen.
Thoracoabdominal Diaphragm
- The vena caval foramen is within the central tendon of the diaphragm, at T8. The inferior vena cava passes through it, along with the right phrenic nerve. Because this foramen is within the central tendon, it will get larger when the diaphragm contracts, because the central tendon is pulled taut. This helps venous return to the heart by increasing the diameter of the inferior vena cava.
- The esophageal hiatus is within the muscular part of the diaphragm, at T10. The esophagus and vagal trunks pass through it. This hiatus gets smaller in diameter when the diaphragm contracts, which helps to prevent esophageal reflux.
- The aortic hiatus is at T12 and is actually an opening that is behind the diaphragm. The aorta runs right behind a ligamentous area at the posterior midline of the diaphragm and is just anterior to the vertebral bodies. This anatomy protects the aorta from diaphragmatic contractions. The thoracic duct travels through the diaphragm with the aorta.

This video shows an interesting clinical case of phrenic nerve injury, its consequences, and the results of a nerve repair!
KNOWLEDGE CHECK
Abdominal Organs
Gastrointestinal Tract and Associated Organs
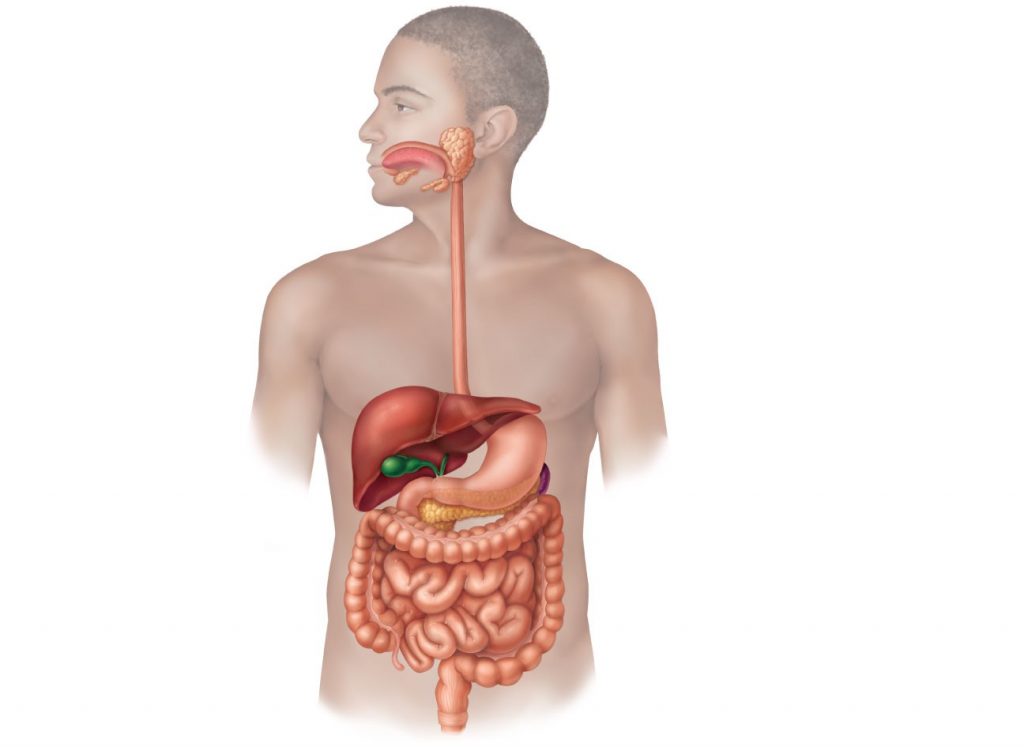
The gastrointestinal (GI) tract is a single tube, extending from the oral cavity, pharynx, and esophagus, through the stomach, small intestine, and large intestine, ending in the rectum and anus. Each segment of the GI tract is regionally specialized for particular digestive functions. In addition to the tube itself, there are three important glands that empty into the small intestine: the liver, gall bladder, and pancreas.
At every level of the GI tract, one of the major functions is propulsion: ingested food must be moved inferiorly to continue the digestive process. Certain parts of the digestive system are responsible for mechanical digestion: physically breaking up ingested food into smaller particles. Most regions of the digestive tract also have critical roles in chemical digestion: secreting enzymes and other chemicals to break chemical bonds and transform ingested food into absorbable particles.
Abdominal Quadrants
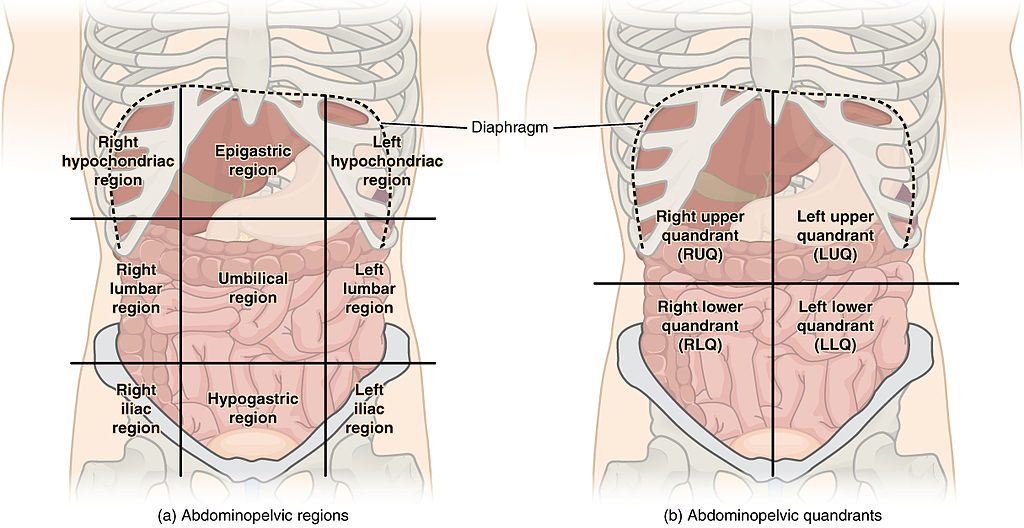
In order to make it easier to describe the anatomy and to assess patients’ conditions, the abdomen can be divided into regions, according to various systems. Two common systems are shown in the figure above. The abdomen can be divided into nine regions (at left) or into four quadrants (at right). For the purposes of this class, we will divide the abdomen into four quadrants: right upper, left upper, right lower, and left lower quadrants. You should understand the position of the organs of the abdomen in relation to these quadrants.
- The right upper quadrant contains the liver and associated structures and most of the duodenum.
- The left upper quadrant contains the spleen and much of the stomach.
- The right lower quadrant contains the appendix.
- The left lower quadrant contains the sigmoid colon.
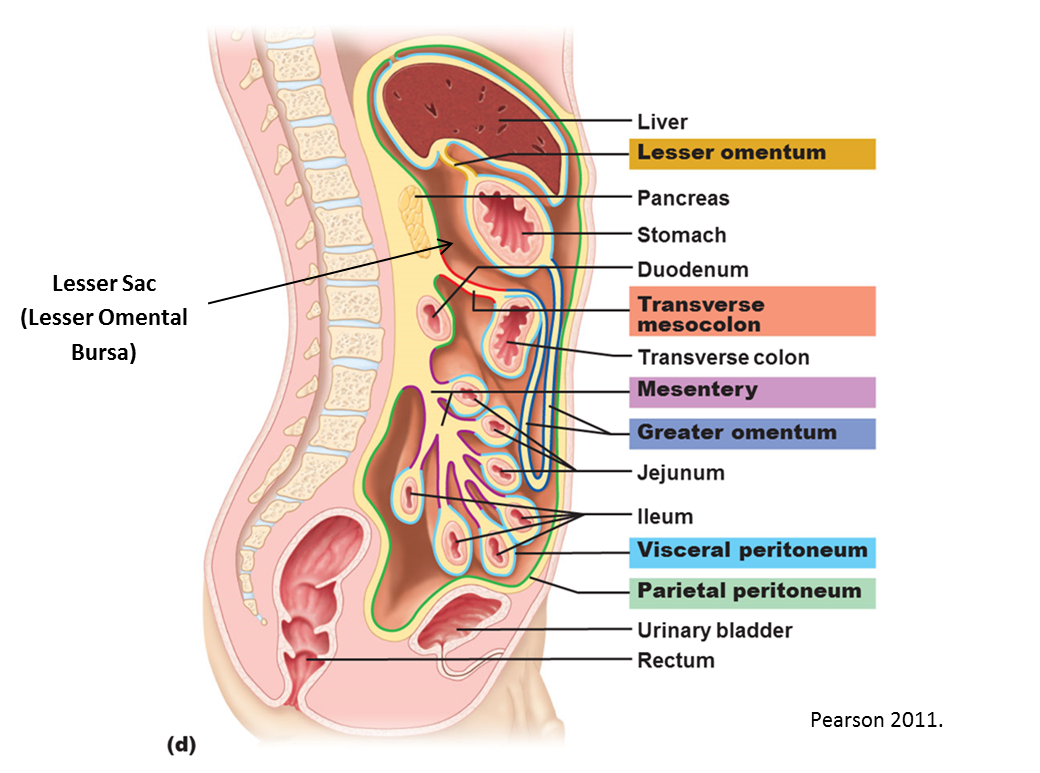
Peritoneum and Regions Within the Abdomen
Just as the thoracic organs are surrounded by sacs (the pericaridal and pleural sacs), the abdomen contains a sac called the peritoneum that surrounds many of the abdominal organs. The peritoneum has the same basic functions as the pericardial and pleural sacs: secretes a small amount of fluid into its cavity to help organs move relative to other structures, reflections act as a corridor for blood vessels to travel from the aorta to the organ. The parts of the peritoneum are also referred to in the same way as the sacs in the thorax: visceral peritoneum lines the organ itself, parietal peritoneum lines the body wall. However, the peritoneum surrounds not one organ, but many (very oddly shaped) organs, and this causes the peritoneal sac to be much more complex in shape than the pericaridal or pleural sacs.
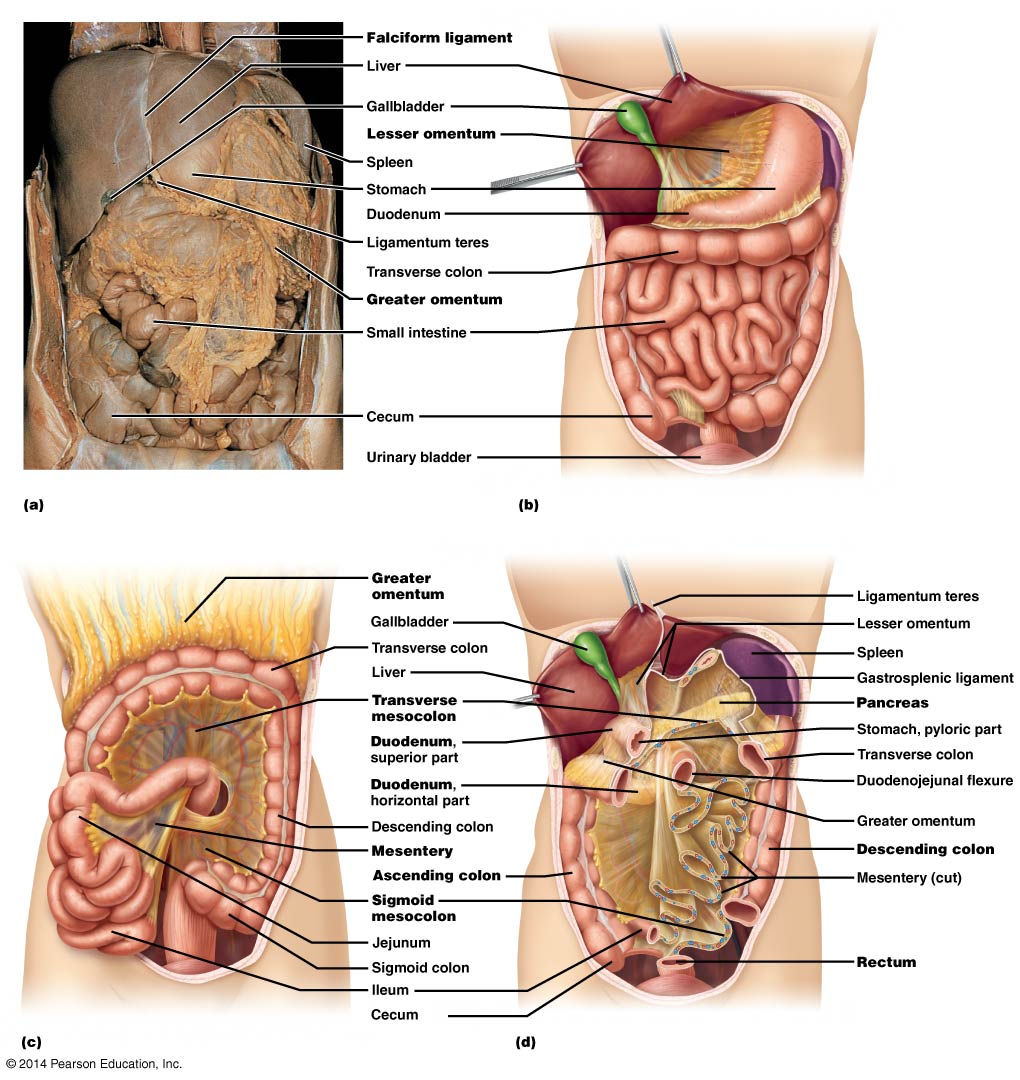
Mesenteries (reflections from parietal to visceral peritoneum) provide pathways for vessels and nerves to reach the organs. Each mesentery is named based on the organ to which it is attached. For example:
- mesointestine (aka mesentery proper): small intestine
- transverse mesocolon: transverse colon
- sigmoid mesocolon: sigmoid colon
There are regions of the mesenteries that also get named because they have a special significance:
- greater omentum: large overgrowth of the mesentery that connects the stomach and the transverse mesocolon, looks like a large apron filled with variable amounts of fat
- lesser omentum: mesentery connecting liver to stomach, encloses a small sac posterior to it known as the lesser sac
- hepatoduodenal ligament: part of the lesser omentum that transmits the proper hepatic artery, hepatic portal vein, and common bile duct (see below for more details on all of these structures)
- falciform ligament: extends between anterior body wall and liver, contained the umbilical vein during fetal life (now know as the round ligament of the liver)
Stomach
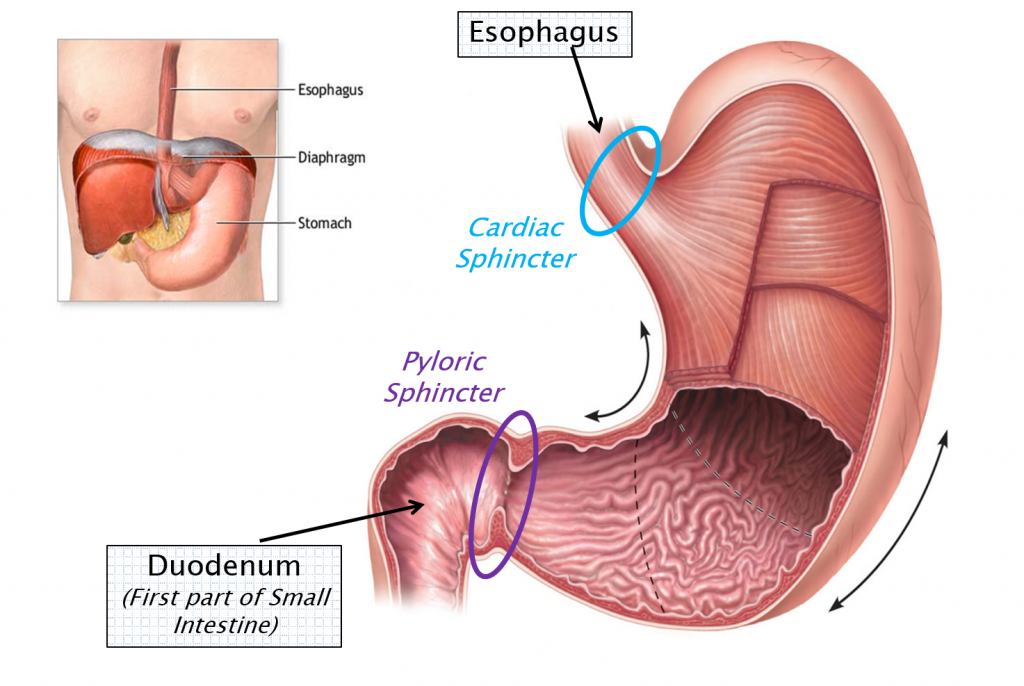
The stomach is the widest part of the GI tract. Food from the esophagus enters the stomach through the cardiac sphincter which is just inferior to the diaphragm. The large volume and expandability of the stomach allows it to store food after eating and slowly release it to the small intestine. Normal capacity of the stomach is about one liter, though it can purportedly be stretched to a whopping four liters of capacity!
The pyloric sphincter regulates the movement of food from the stomach to the proximal part of the small intestine (the duodenum). Unlike the cardiac sphincter, the pyloric sphincter is highly functional and regulates the movement of food past the stomach.
The stomach has several functions:
- Storage of food: The large capacity of the stomach allows us to eat larger amounts at one time. The stomach releases ingested food slowly to the small intestine, which allows for more complete digestion and absorption of nutrients.
- Mechanical digestion: Contraction of three layers of smooth muscle in the wall of the stomach grinds ingested food into smaller particles and mixes it with stomach secretions.
- Chemical digestion: Cells in the epithelial lining of the stomach secrete hydrochloric acid, which helps break food into smaller pieces, and pepsin, an enzyme which digests proteins.
The slurry of digested food and gastric juices that leaves the stomach is called chyme.
Small Intestine
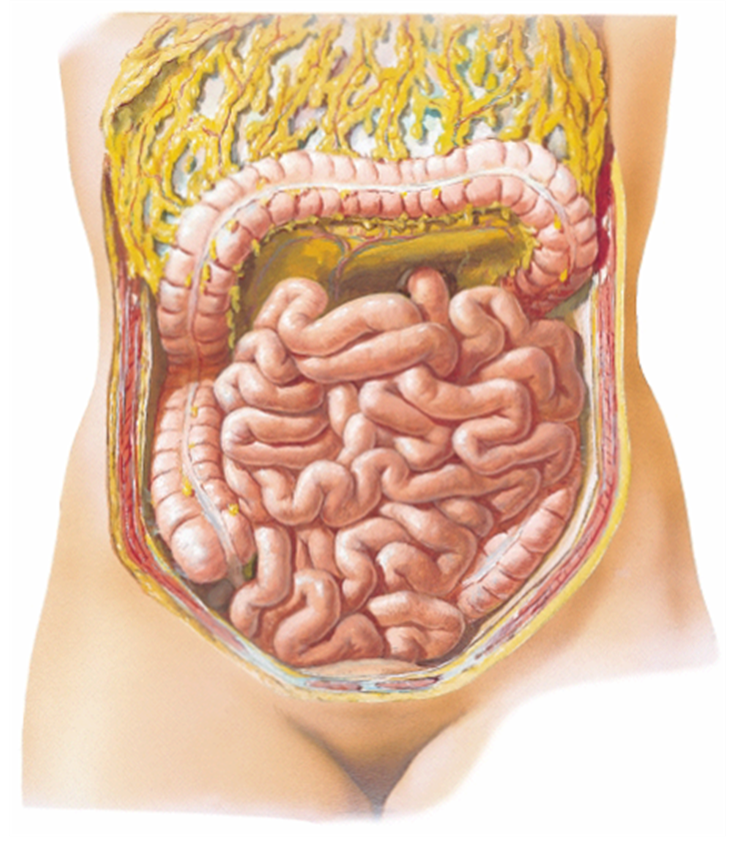
There are three regions of the small intestine: the duodenum, jejunum, and ileum. Though they are distinct histologically, the three segments of the small intestine are not distinguishable grossly. You should know them by location.
- The duodenum is the C-shaped segment continuous with the stomach; it is wrapped around the head of the pancreas in the posterior abdomen. It is consists of the first twelve inches (or so) of the small intestine and receives all of the secretions from the liver, gall bladder, and pancreas. Its lining contains bicarbonate-secreting glands (Brunner’s glands) to neutralize the acidic chyme from the stomach.
- The jejunum is located mostly in the upper left quadrant of the abdomen. This middle section of the small intestine has extensive folds to facilitate both secretion of digestive enzymes and absorption of nutrients by the cells lining its walls.
- The ileum empties into the cecum of the large intestine and is located mostly in the lower right quadrant. It has abundant immune cells in its walls (Peyer’s patches). The ileum ends at the junction with the large intestine (the ileocecal junction).
All three segments of the small intestine are important for both chemical digestion and absorption of nutrients. Cells lining the small intestine secrete digestive enzymes (which break down fats, proteins, and carbohydrates) as well as absorb nutrients from the lumen of the gut. Deep to the epithelial lining of the small intestine are dense networks of blood and lymphatic capillaries. Fats are absorbed into the lymphatic capillaries and then travel through the lymphatic system to the thoracic duct, which returns them to the venous circulation of the body. Proteins and carbohydrates are absorbed into the blood capillaries. Blood from these capillary beds travels to the liver, via the hepatic portal circulation (below). The liver will process proteins and carbohydrates for use by the cells of the body.
Liver, Gall Bladder, and Pancreas
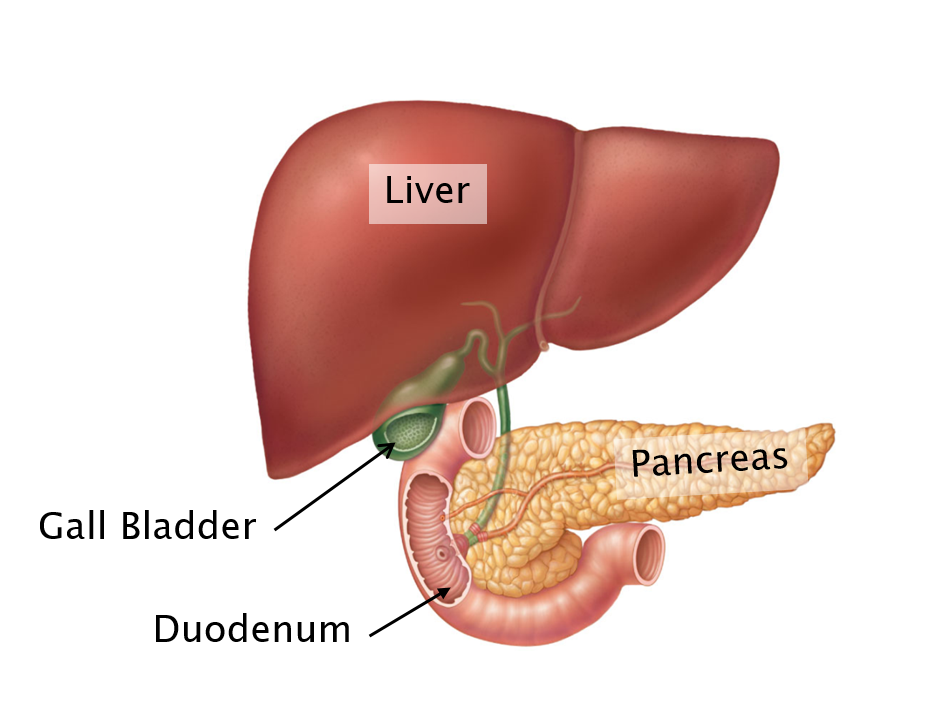
The liver is the largest gland in the body and it has many functions (most of which are beyond the scope of this class). Cells of the liver (hepatocytes) process the nutrients (proteins and carbohydrates) and toxins absorbed by the digestive tract, metabolize waste products from red blood cell destruction in the spleen, and produce bile.
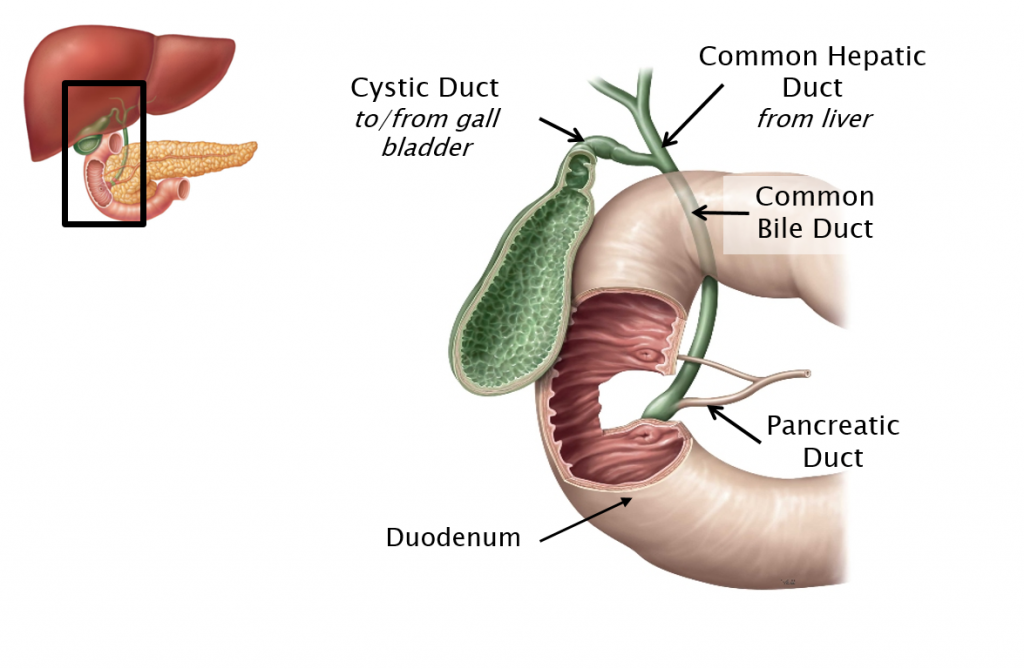
Bile is a substance which emulsifies fats, breaking them into smaller pieces in order to make them more susceptible to enzymatic digestion. Hepatocytes produce bile constantly. Bile leaves the liver through the common hepatic duct. If bile is not needed in the duodenum to digest fats immediately, it will travel into the gall bladder through the cystic duct where it will be stored until needed. When fat reaches the small intestine, the gall bladder is stimulated to release bile. Bile travels through the common bile duct to the duodenum. (The common bile duct carries bile from both the liver and the gallbladder. See figure below.)
To reach the duodenum, the common bile duct passes through the head of the pancreas. The pancreas is a long gland located posterior to the stomach. The head of the pancreas is surrounded by the duodenum. The pancreas is both an exocrine and endocrine organ. Its endocrine function is to secrete insulin and glucagon into the bloodstream. These hormones regulate blood glucose levels by affecting the release and storage of glucose from cells of the liver. Its exocrine function is to secrete digestive enzymes, through the pancreatic duct, into the duodenum. These pancreatic enzymes are critical to chemical digestion in the small intestine, breaking down fats, proteins, and carbohydrates into components that can be absorbed by the epithelium that lines the small intestine.
The pancreatic duct is a tube that runs through the length of the pancreas. Within the head of the pancreas, the common bile duct and the pancreatic duct join together briefly and empty into the duodenum through a common opening. Because the two duct systems share a common opening to the duodenum, gallstones (which form in the gall bladder) can potentially block both the secretion of bile and the secretion of pancreatic enzymes into the duodenum, depending on where the gallstones lodge.
Large Intestine (Colon) & Rectum
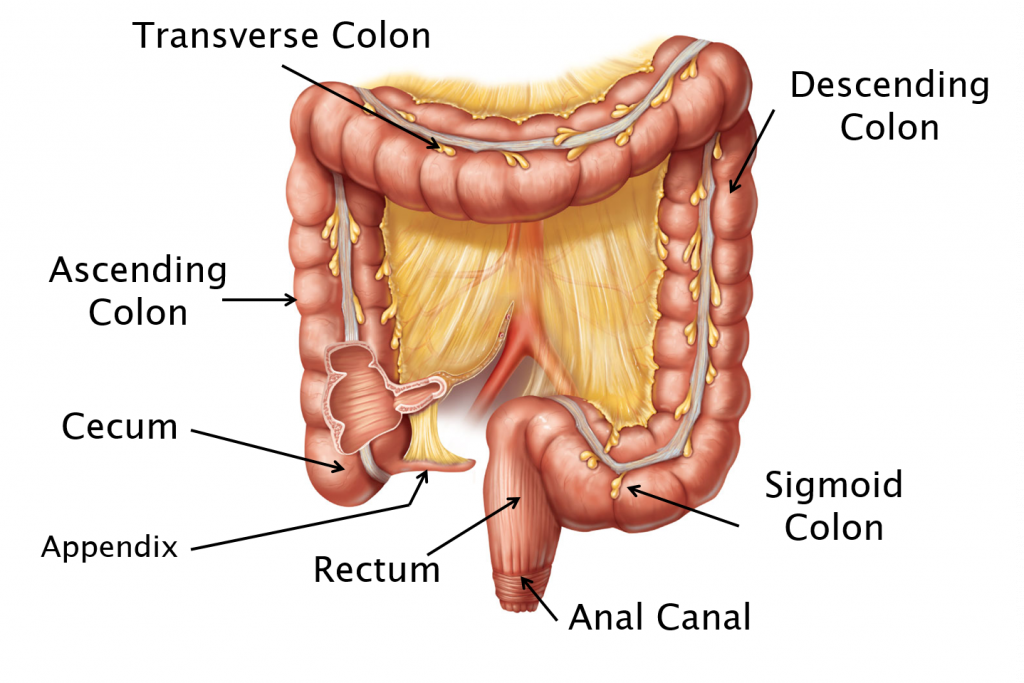
The ileum of the small intestine empties into the large intestine (colon) at the cecum (through the ileocecal junction, in the lower right quadrant of the abdomen). Hanging off of the inferior part of the cecum is the appendix, a small appendage which is filled with lymphatic tissue (lymphocytes, macrophages, and supporting tissues). Food passes from the cecum through the ascending, transverse, descending, and sigmoid colons. The junction between the ascending and transverse colons is called the hepatic flexure; the junction between the transverse colon and the descending colon is called the splenic flexure. The sigmoid colon passes into the pelvis where it becomes the rectum. Fecal waste leaves the body through the anal canal and the anus.
The primary function of the large intestine is the absorption of water and vitamins.
The passage of fecal waste out of the body is regulated by two sets of sphincter muscles in the anal canal. The internal anal sphincter is made of smooth muscle and is under involuntary control. Generally, sympathetic innervation keeps this sphincter closed and parasympathetic stimulation relaxes it. The external anal sphincter is made of skeletal muscle and is under voluntary control. This skeletal muscle sphincter is innervated by the pudendal nerve, which is comprised of ventral rami from S2, S3, and S4 spinal levels.
Spleen
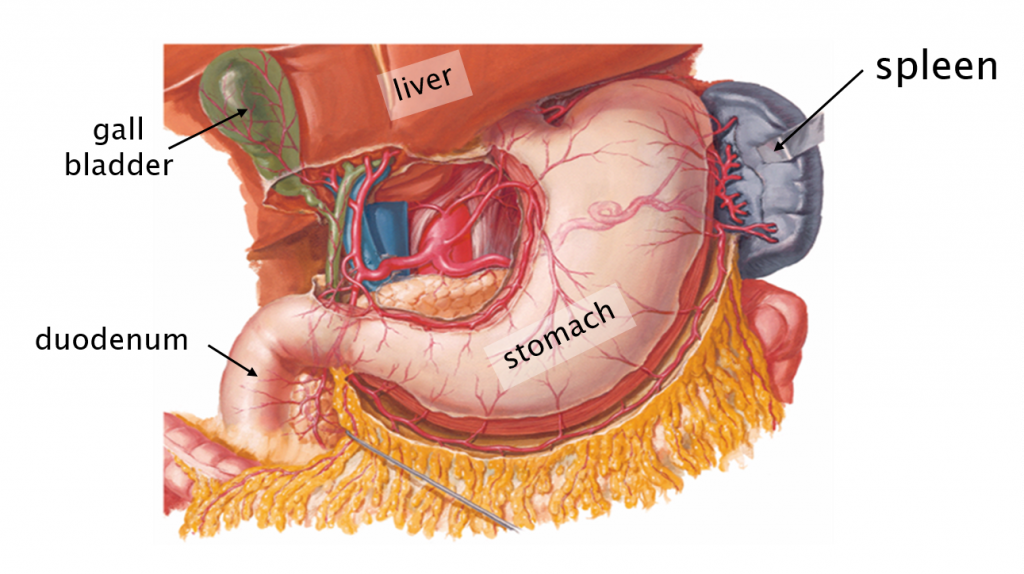
The spleen is an organ of both the immune and circulatory systems located in the posterior recess of the superior left abdomen, near the tail of the pancreas. Although it is not a digestive organ, the spleen is supplied by the arteries which also supply the organs of the digestive system. Importantly, the spleen’s venous drainage passes through the hepatic portal system (below).
One of the important functions of the spleen is to destroy old red blood cells. This process produces bilirubin, a waste product. Bilirubin travels to the liver via the hepatic portal vein and is recycled by hepatocytes as a component of bile. As described above, bile is released to the small intestine where it emulsifies fats.
The spleen is also a reservoir for blood. The blood supply to the spleen is huge and damage to the spleen can cause major blood loss. Since the organ is difficult to repair, it is often removed if it is damaged.
KNOWLEDGE CHECKS
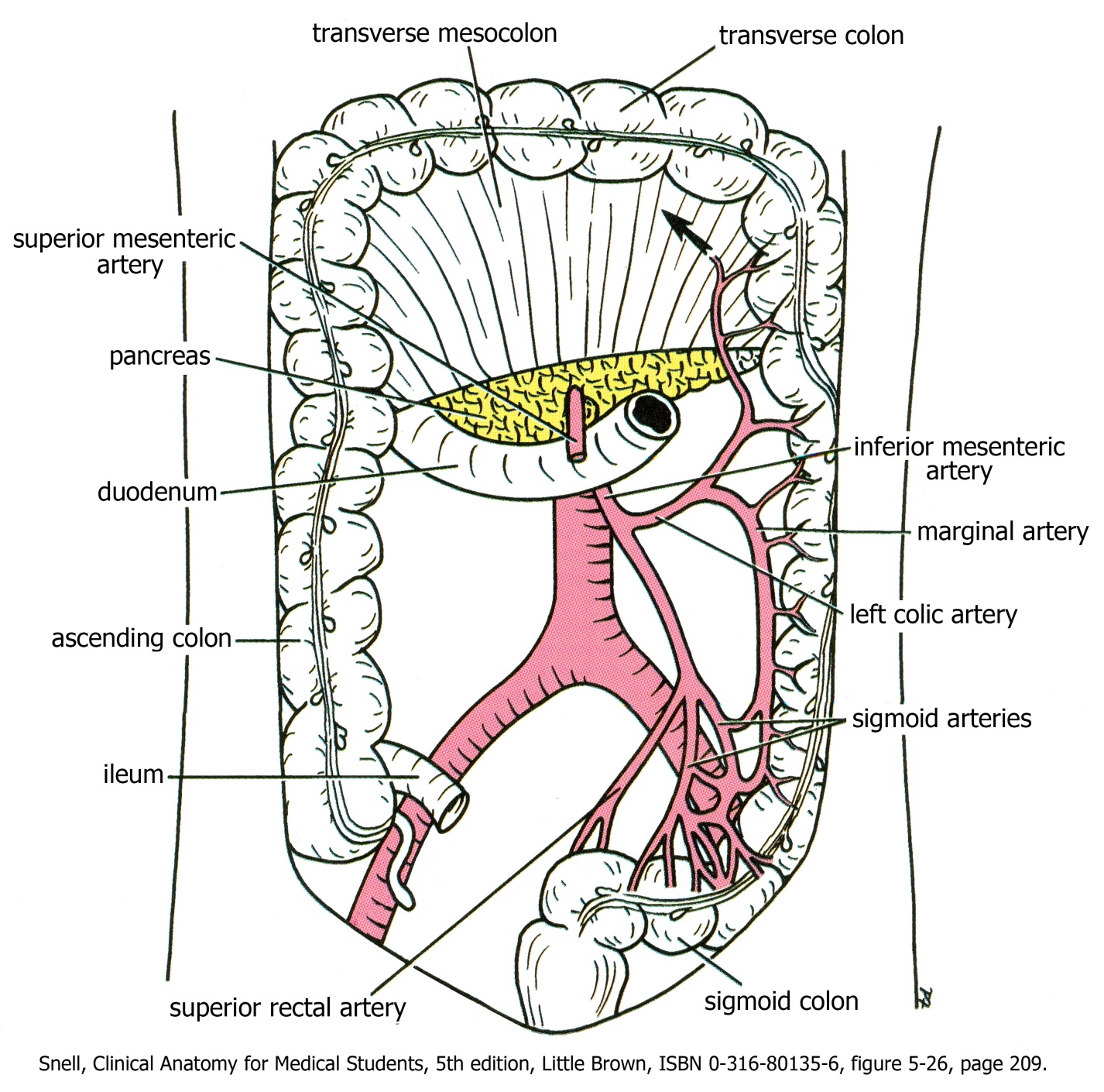
Arteries of the Digestive System
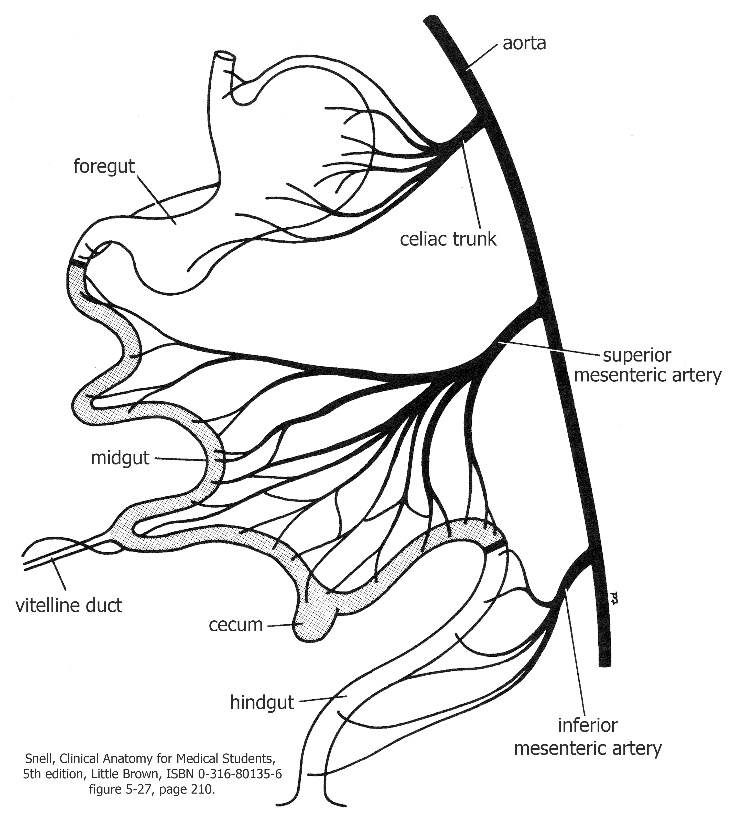
The blood supply to the gut tube is related to its development. Early in the embryo, the developing gut tube is supplied with blood by three unpaired branches of the abdominal aorta. The celiac trunk supplies the foregut (stomach to duodenum); the superior mesenteric artery supplies the midgut (duodenum to transverse colon); and the inferior mesenteric artery supplies the hindgut (descending colon to anus). There are anastomoses between these three arteries in areas that join foregut to midgut and midgut to hindgut. These patterns of circulation, established very early in development, persist throughout the formation of the convoluted gut tube and into the adult.
The main arteries to the digestive system have extensive branching. The names of all of the many (many!) branches is beyond the scope of this course, but we will dissect some of them to get a sense of the vast branching patterns. Branches that you definitely need to know are in bold (and are included in the lab as well).
Celiac Trunk
The celiac trunk supplies the stomach, spleen, liver, and parts of the duodenum. The liver receives arterial blood from a branch of the celiac trunk called the proper hepatic artery (see Venous Drainage of the Gut and Spleen below for the other part of the liver’s blood supply). The spleen receives blood from a very distinctively curly artery (like a pig tail!) called the splenic artery. The stomach receives blood from multiple branches of the celiac trunk. If you see “gastro” in the name of an artery, it goes to the stomach.
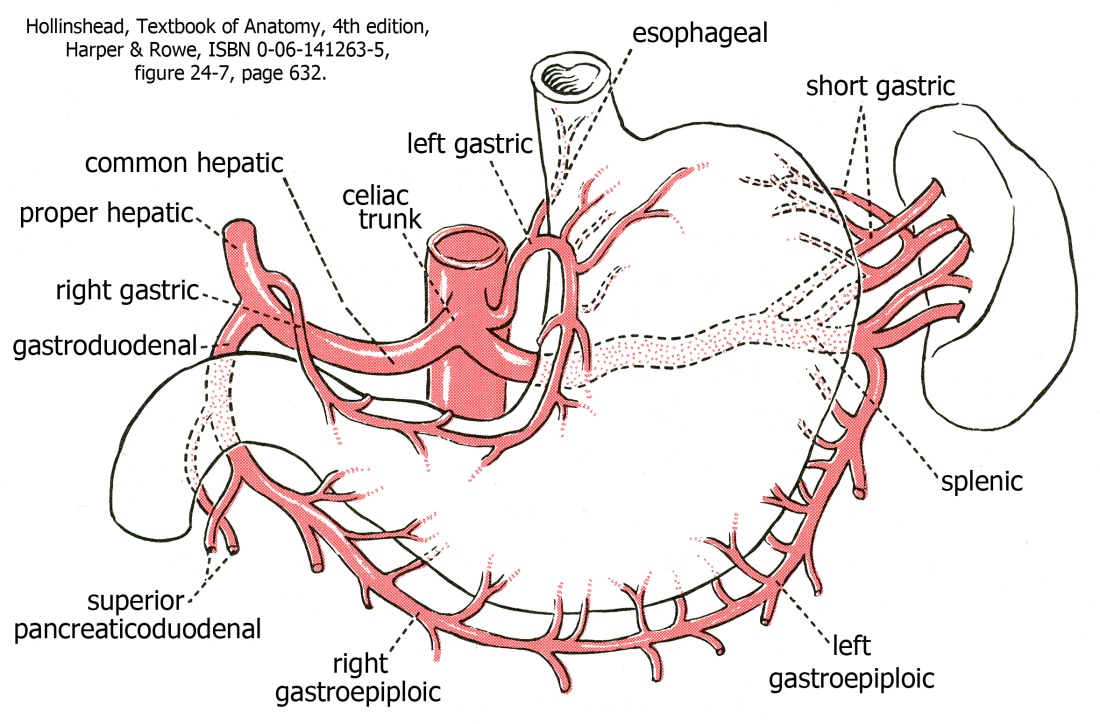
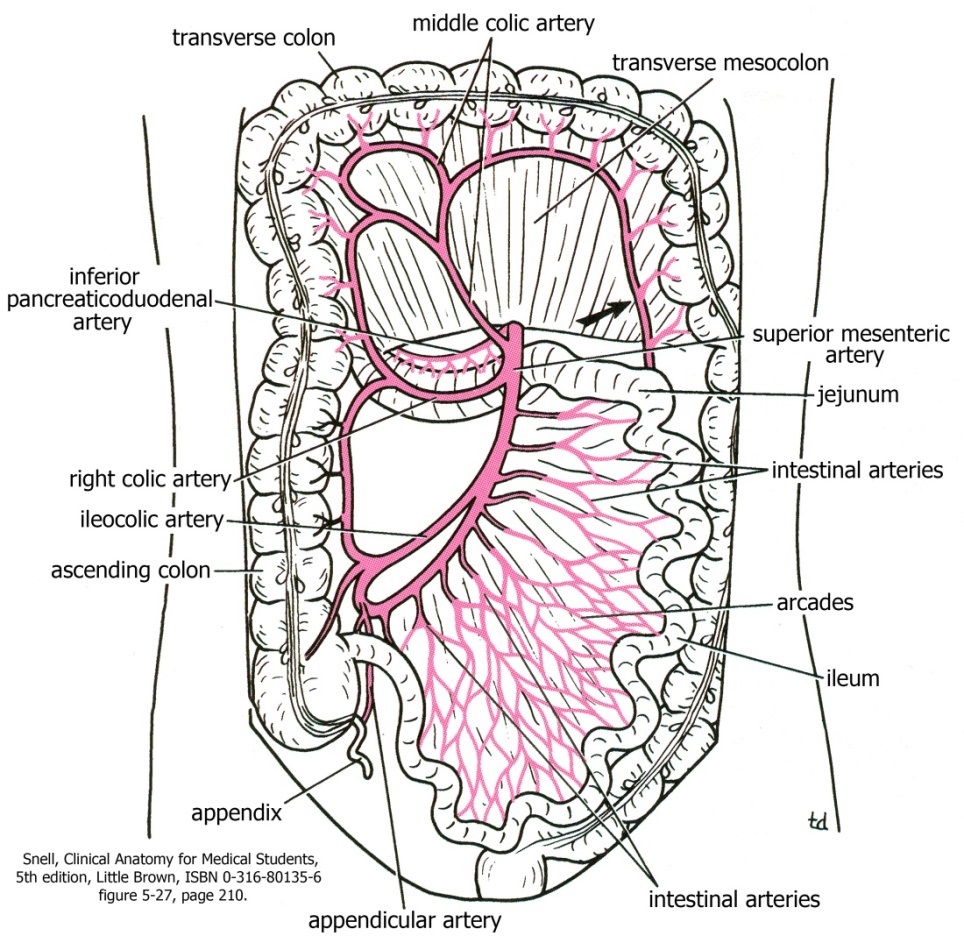
Inferior Mesenteric Artery
The inferior mesenteric artery branches from the aorta just superior to the aortic bifurcation (near L3-L4 vertebral bodies). The inferior mesenteric artery supplies the descending colon, sigmoid colon, and rectum. Branches from the inferior mesenteric artery are named after the location on the colon they supply. For example, branches to the sigmoid colon are called sigmoid arteries.
Venous Drainage of the Gut Tract and Spleen
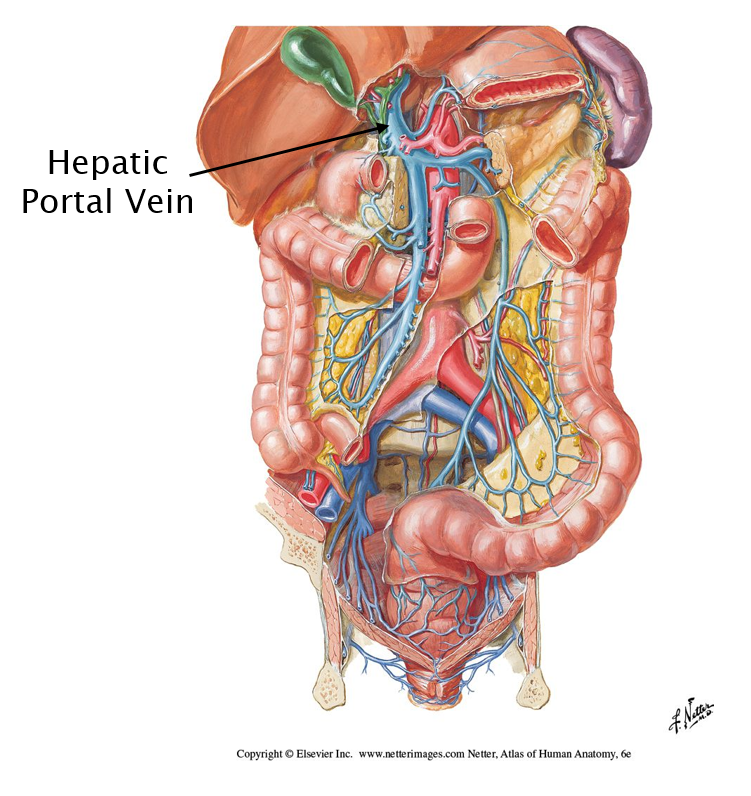
The return of venous blood from the GI tract involves a portal system: a system of veins that connects two capillary beds. In this case, the first set of capillary beds are within the walls of the gut tube (where nutrients are absorbed) and in the spleen (which destroys red blood cells); the second set of capillary beds is within the liver (where the absorbed nutrients, as well as bilirubin from the spleen, are processed).
All of the venous drainage from the capillary beds of the GI tract and spleen ends up in the hepatic portal vein, a huge vein leading into the liver. After being processed in the capillaries of the liver, blood leaves the liver through the hepatic veins and enters the inferior vena cava (and the systemic circulation).
Urinary Tract
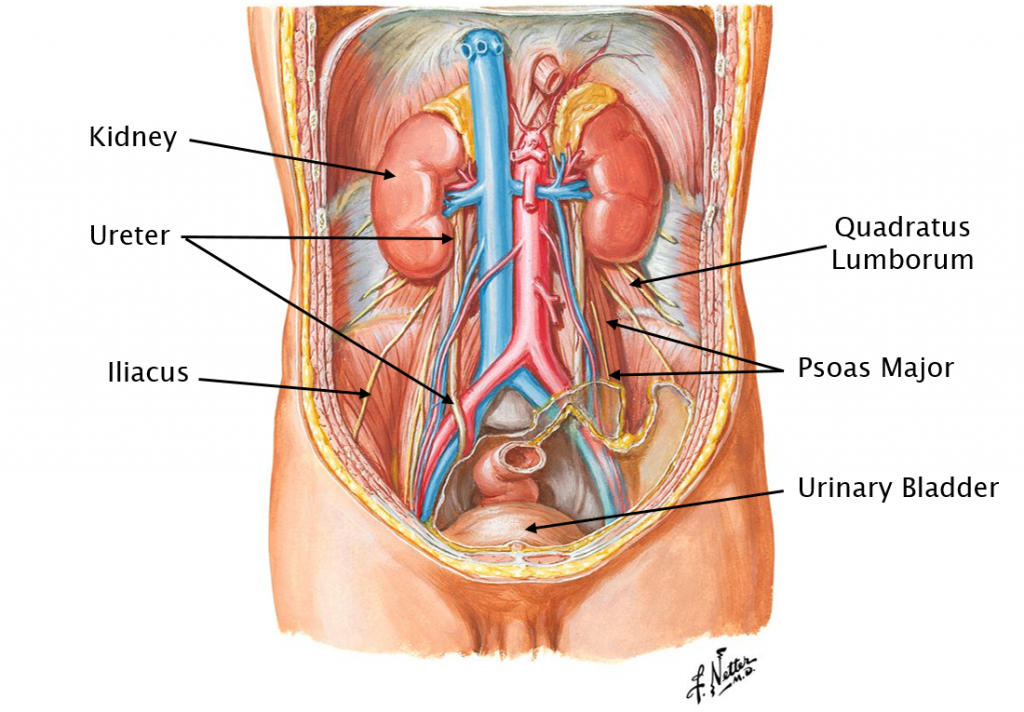
The kidneys are located in the superior abdomen, posterior to all of the organs of the digestive system. Although they are not large organs, the kidneys receive 25% of the cardiac output of blood, a testament to their critical function in maintaining appropriate blood volume, pressure, and concentration. All of the kidney’s vasculature as well as the ureter enter or exit the organ from the medial side (at the hilus of the kidney). Usually there is a single renal artery and vein, as well as a single ureter. The large renal arteries branch directly off the aorta; the renal veins empty into the inferior vena cava.
The adrenal (suprarenal) glands sit on top of the kidneys, but are not functionally associated with them. These endocrine glands secrete epinephrine and norepinephrine into the blood stream to elicit a systemic sympathetic response. They also secrete corticosteroids and androgens, among other hormones.
The ureters are extremely muscular tubes (smooth muscle). Peristaltic contractions of the walls of the ureters move urine from the kidneys to the urinary bladder. Urine is not altered as it travels down the ureter. The ureters pierce the posterior wall of the urinary bladder. Their oblique course through the muscular wall of the bladder acts as a valve, closing off the ureteric opening when the bladder is full. This prevents urine from backing up from the urinary bladder to the kidneys.
The urinary bladder is located in the pelvis, but can extend into the lower abdomen when it is distended. Since it stores urine until it is possible (or necessary) to eliminate it, the urinary bladder can stretch to many times its resting size. The epithelium lining the urinary bladder is able to stretch as the organ distends. The organ has extremely thick muscular walls (smooth muscle), which contract to eliminate urine.
At the base of the bladder, at the junction with the urethra, is an involuntary internal urethral sphincter (made of smooth muscle) which prevents the bladder from emptying; it contracts involuntarily (so we don’t have to think about it). Sympathetics generally keep the sphincter closed; parasympathetic stimulation relaxes the sphincter.
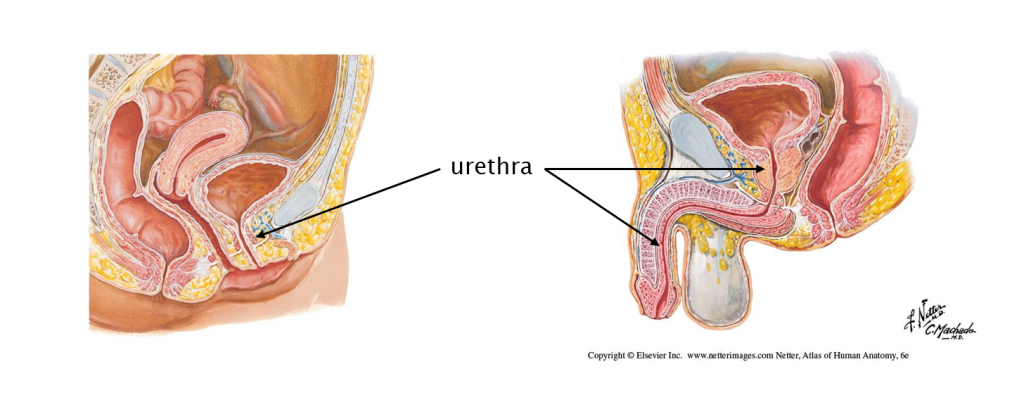
Urine leaves the bladder through the urethra. In females, the urethra is fairly short. It passes through a sheet of skeletal muscle (the urogenital diaphragm) which contains the external urethral sphincter (skeletal muscle; a voluntary sphincter). In males, the urethra is much longer and consists of 3 distinct segments:
- the prostatic urethra (which passes through the prostate gland)
- the membranous urethra (which passes through the urogenital diaphragm & is the site of the external urethral sphincter)
- the penile urethra (which passes through the erectile tissue of the penis).
More about this when we talk about the pelvis!!
There are two important muscles in the posterior abdomen which are involved in moving the lower limb: psoas major and quadratus lumborum. We will discuss them with the lower limb.
