Main Body
Anatomy of the Heart & Pericardium
Elise Davis PhD
Sections
- Overview of the Heart and Circulatory System
- Anatomy of the Pericardium
- Internal Anatomy of the Heart
- Overview of Histology of the Heart
- Heart In Situ
- Surface Anatomy of the Heart
- Clinical Application: Anatomical Basis for Auscultation Points (Heart Sounds)
- Clinical Application: Anatomical Basis for Auscultation Points (Heart Sounds)
- Surface Anatomy of the Heart
- Coronary Circulation
- Coronary Arteries
- Cardiac Veins
- Clinical Application: Myocardial Infarct and Treatments for Coronary Artery Blockages
Overview of the Heart and Circulatory System
From early in the development of the embryo, the heart pumps blood through the body. Each time the heart beats it sends blood through three different parts of the circulatory system simultaneously.
- The pulmonary circulation sends blood to and from the lungs to be oxygenated.
- Deoxygenated blood goes from the heart to the lungs; oxygenated blood is returned from the lungs to the heart.
- The systemic circulation sends blood to and from the body to deliver oxygenated, nutrient-rich blood to the tissues and remove waste and carbon dioxide from the tissues.
- Oxygenated blood goes from the heart to the tissues of the rest of the body; deoxygenated blood returns to the heart from the body.
- The coronary circulation is a special subset of the systemic circulation and sends blood to and from the tissue of the heart itself.
- Oxygenated blood travels to the tissues of the heart wall; deoxygenated blood returns to the heart chambers.
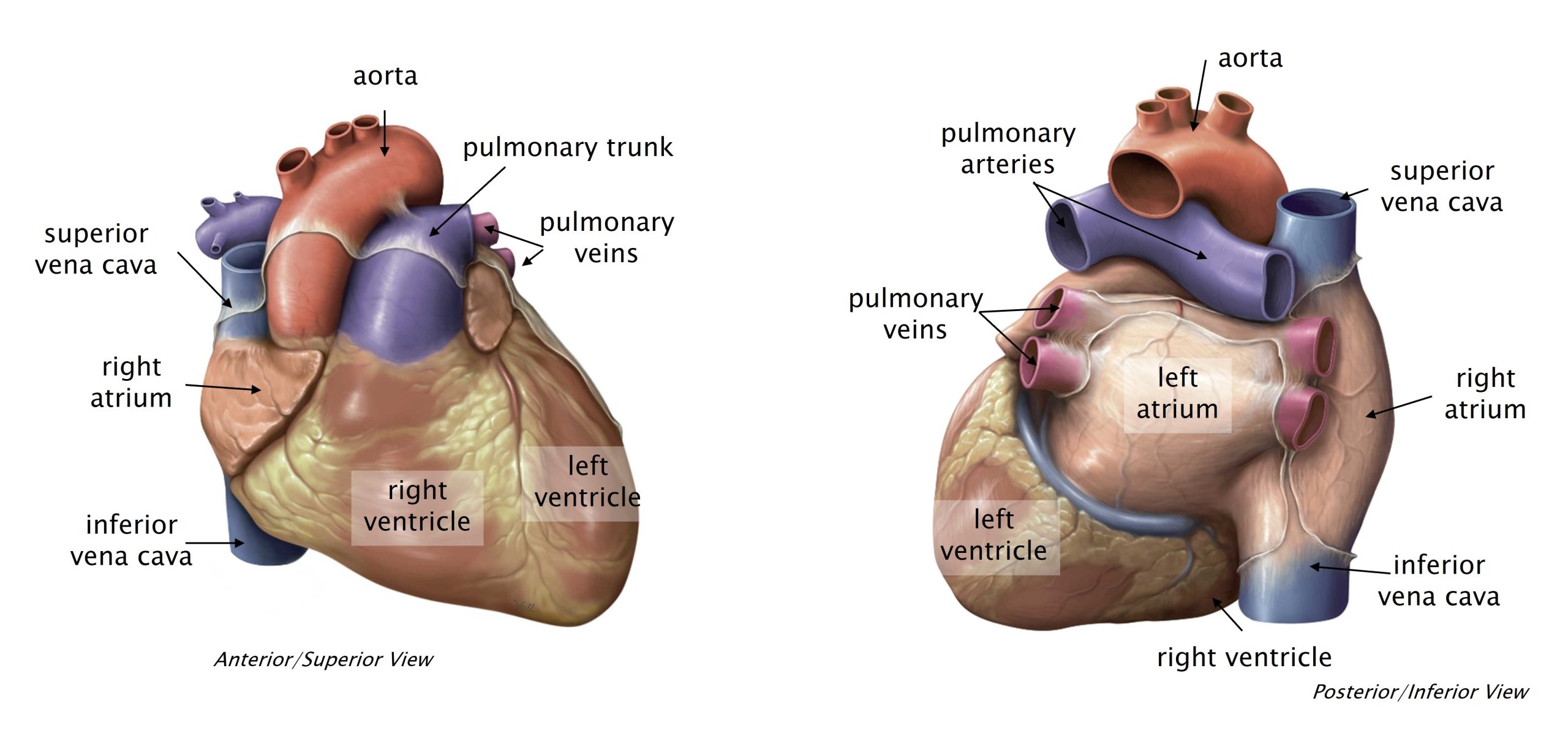
In all parts of the circulatory system, blood travels away from the heart in vessels called arteries. Blood travels to the heart through vessels called veins. The large veins and arteries that directly enter and exit the heart are called the great vessels.
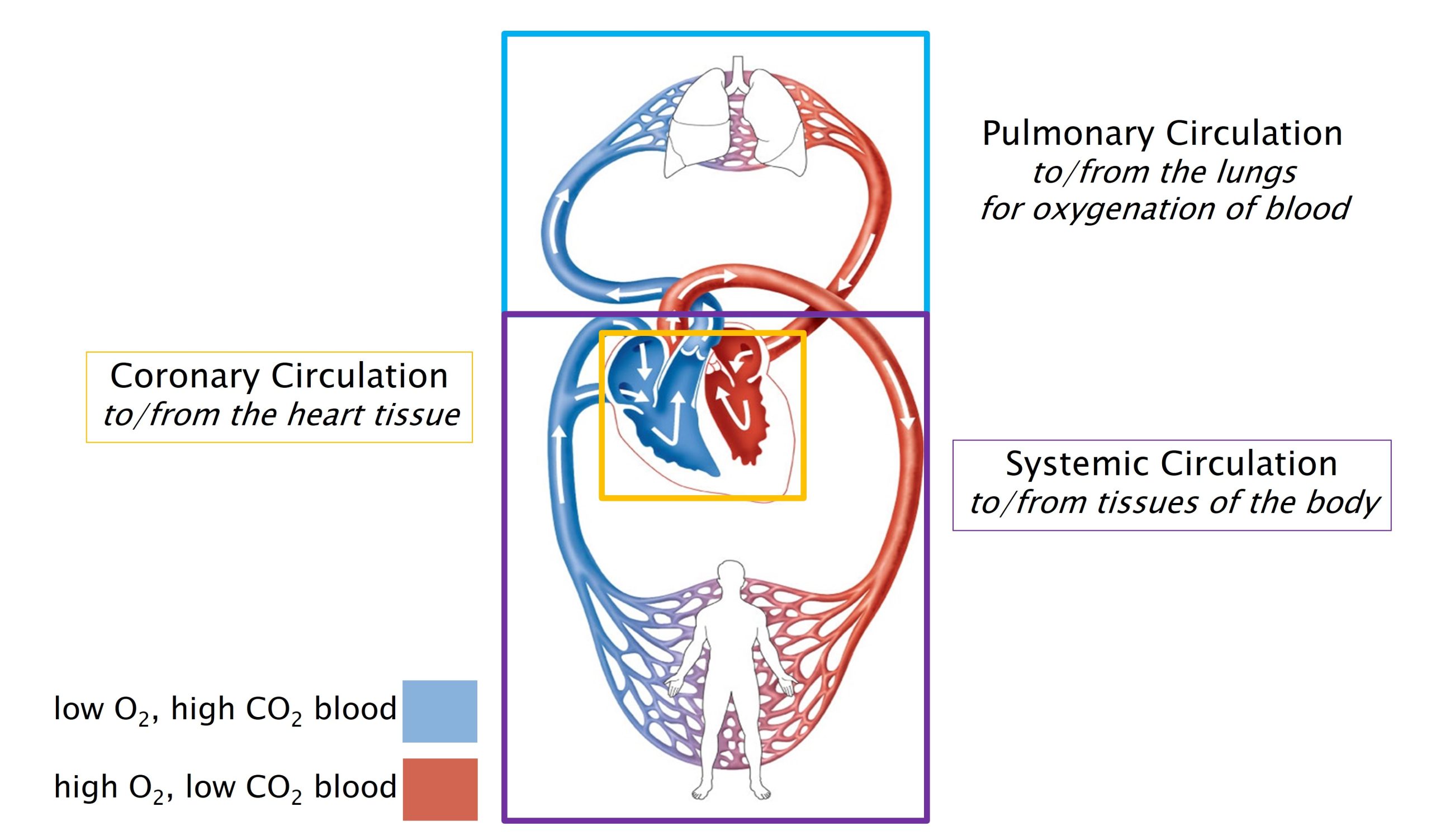
The heart is a modified tube that is continuous with the blood vessels of the body through the large veins and arteries that lead into and out of the heart. Within the heart, there are four chambers, two atria and two ventricles, through which blood travels in series. The walls of the heart are composed mostly of cardiac muscle, which contracts to pump blood through and out of the heart.
- The left atrium and the right atrium are the chambers of the heart that receive blood from the body.
- The left atrium receives oxygenated blood from the lungs.
- The right atrium receives deoxygenated blood from the rest of the body, including from the heart itself.
- Atria is the plural form of atrium: “the left and right atria”.
- The right and left ventricles are the chambers of the heart that eject blood into the pulmonary, systemic, and coronary circulations.
- The right ventricle sends deoxygenated blood to the pulmonary circulation.
- The left ventricle sends oxygenated blood to the systemic and coronary circulations.
In summary:
- The right side of the heart contains deoxygenated blood, receives blood from the tissues of the body, and sends blood to the lungs to be oxygenated.
- The left side of the heart contains oxygenated blood, receives blood from the lungs, and sends oxygenated, nutrient-rich blood to the body, including the tissues of the heart.
- Blood flows through the chambers of the heart in series:
- Blood from the body enters the heart on the right side, flows through the right atrium, then the right ventricle.
- From the right ventricle, blood goes to the lungs.
- From the lungs, blood enters the left atrium, then the left ventricle.
- From the left ventricle, blood goes to the body. Then, back to the right atrium.
Knowledge Check
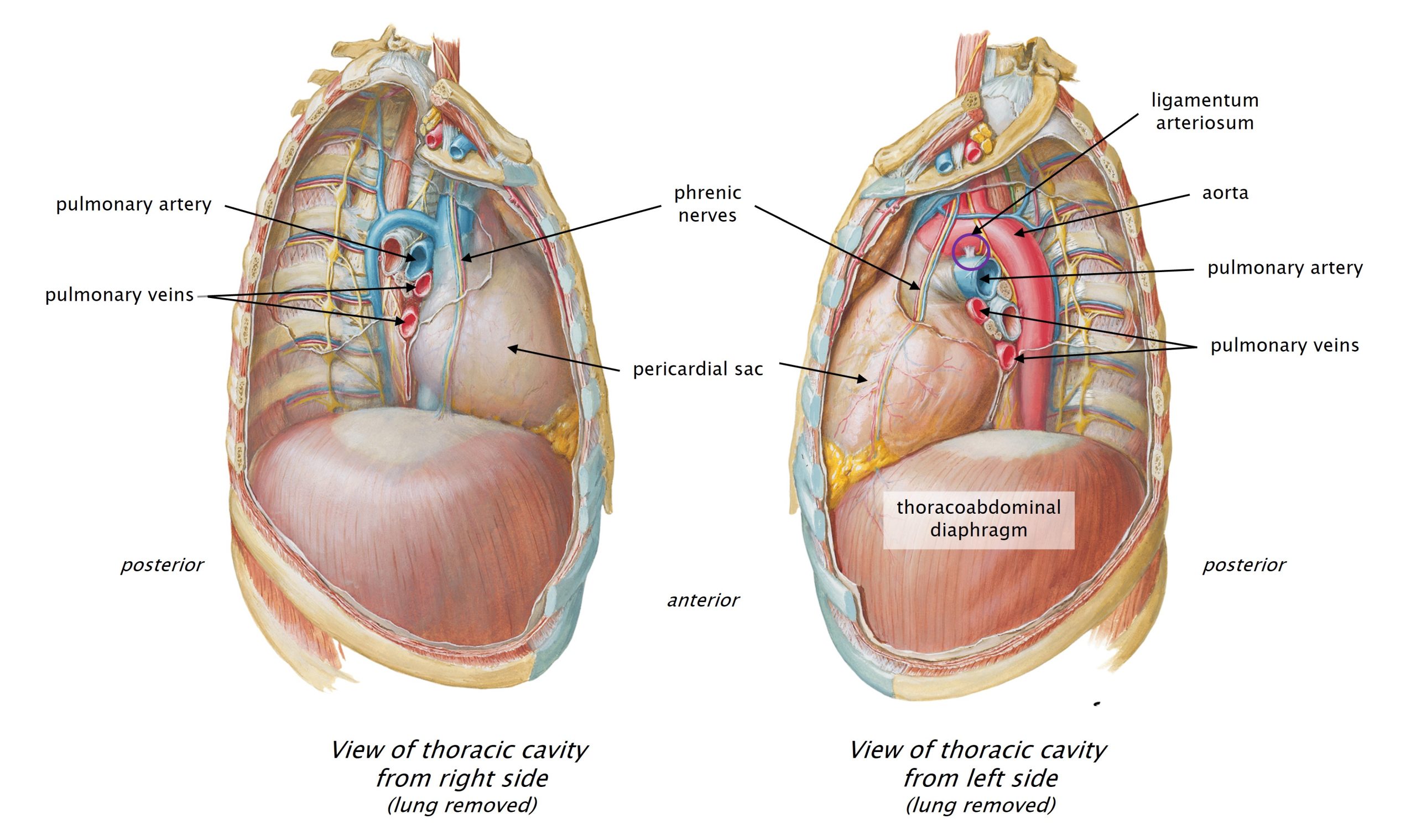
Anatomy of the Pericardium
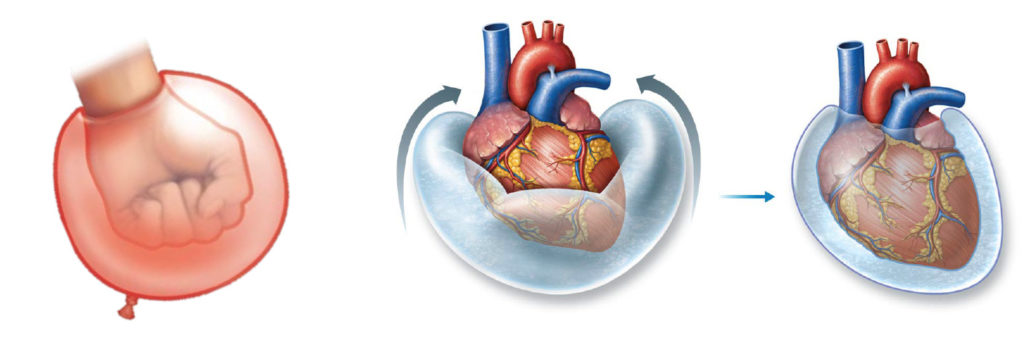
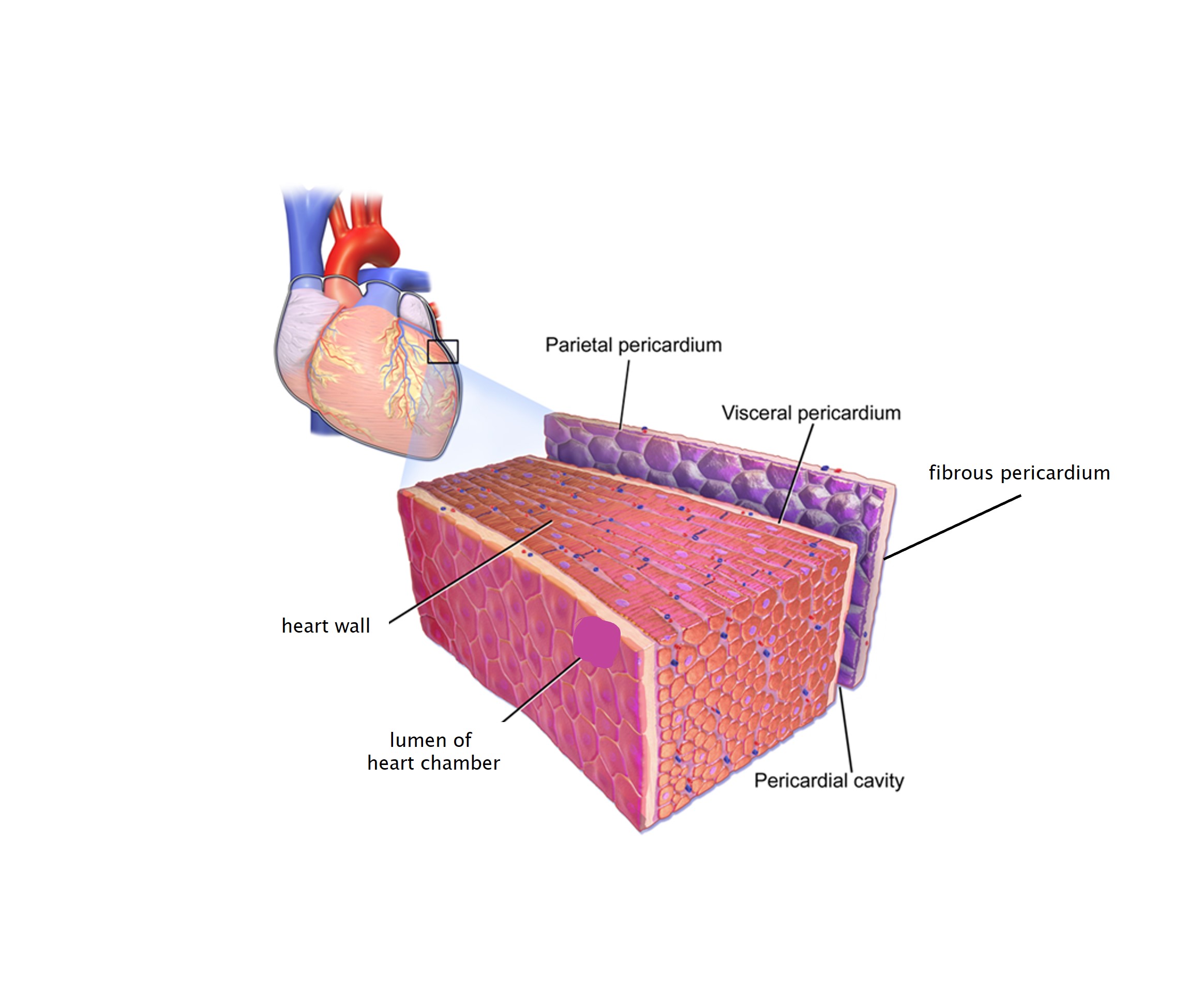
The heart is located in the thorax, the body cavity that is deep to the rib cage and superior to the thoracoabdominal diaphragm. The heart and lungs fill the thorax. The heart is surrounded by a fluid-filled sac, the pericardial sac. This sac both anchors the heart in the middle of the thorax and allows the organ to freely move as it beats within the thoracic cavity. The two parts of this sac have different features which facilitate these functions.
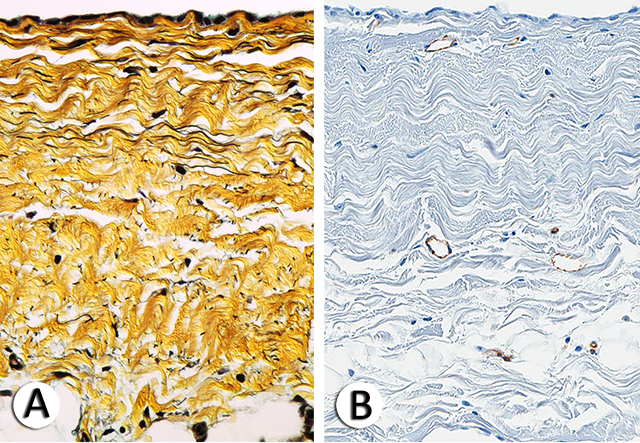
- The fibrous pericardium is the most external part of the pericardial sac. It is a thick connective tissue sac that is adhered to the thoracoabdominal diaphragm inferiorly and the great vessels superiorly. The dense tissue of the fibrous pericardium doesn’t stretch easily. This sac of connective tissue anchors the heart in place within the thoracic cavity and limits the amount that the heart can expand when filling with blood.
- The serous pericardium is deep to the fibrous pericardium. It is a continuous, closed sac (like a closed balloon) with a small amount of fluid inside. The serous sac has two layers. (Imagine a closed balloon shrink-wrapped around the organ–as if you pushed your fist into a partially-inflated balloon.) The serous pericardium is made of a layer of simple squamous epithelium (mesothelium) and a thin layer of loose connective tissue that contains elastic fibers. The mesothelium secretes a small amount of fluid, a lubricant that facilitates free movement of the heart.
- The inner layer of the balloon is called visceral pericardium and is fused to the surface of the heart.
- “visceral” means relating to organs
- The outer layer of the balloon is called parietal pericardium and is fused to the inner surface of the fibrous pericardium.
- “parietal” means wall
- The visceral and parietal pericardia are separated by a thin film of lubricating fluid that allows the two layers to move relative to each other as the heart beats.
- There are similar sacs around the lungs (pleural sacs) and abdominal viscera (peritoneal sac). We will study those later.
- The inner layer of the balloon is called visceral pericardium and is fused to the surface of the heart.
Nearby Structures
Phrenic Nerves: Just external to the fibrous pericardium, the right and left phrenic nerves travel through the thorax on their way from the neck to the diaphragm. The phrenic nerves carry motor and sensory innervation to the thoracoabdominal diaphragm. These nerves make your diaphragm contract during inspiration. Because of some fancy embryology, the phrenic nerves arise from spinal cord levels C3-C5 (even though the diaphragm is located at the border of the thorax and abdomen). Remember: C3,4,5 keep the diaphragm alive! You will find the phrenic nerves during your dissection of the heart. They are embedded in adipose tissue between the fibrous pericardium and the lungs on each side. Both phrenic nerves travel anterior to the roots of the lungs. (The root of the lung is where all the tubes go in and out of the organ.) We will discuss the phrenic nerve in a later unit. You will need to carefully dissect these nerves before you cut open the pericardial sac, so that they will be preserved for later.
Thoracoabdominal Diaphragm: The thoracoabdominal diaphragm is a sheet of skeletal (voluntary) muscle that divides the thorax from the abdomen and is the primary muscle involved in respiration. It is innervated by the right and left phrenic nerves which can be controlled voluntarily (you can decide to take a breath). Contraction of the diaphragm is also controlled unconsciously by a region in the brainstem (so you don’t have to think about breathing). We will discuss the thoracoabdominal diaphragm in more detail later in the block.
Ligamentum Arteriosum: This is a small remnant of a fetal blood vessel (originally called the ductus arteriosus) which connected the pulmonary trunk and the aorta in order to bypass the pulmonary circulation before the lungs were functioning organs. After birth, blood stops flowing through this vessel and it gradually turns into a fibrous cord of tissue. Fun fact: it is about the same diameter that it was when the person was born. It looks small now, but think about how big it was compared to the golf-ball-sized heart of a newborn. We will learn more about fetal circulation in Human Family Tree block.
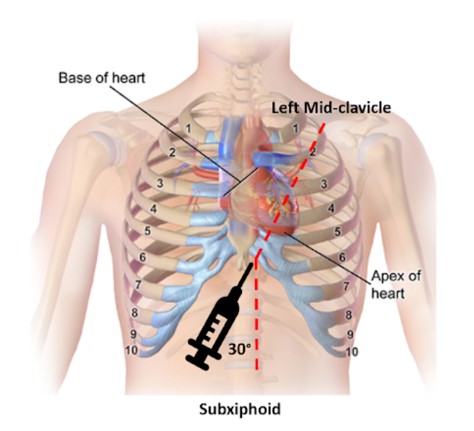
Clinical Application: Pericardial Effusion, Cardiac Tamponade, and Pericardiocentesis
An accumulation of fluid within the pericardial sac is called pericardial effusion. Fluid can accumulate in this closed space as a result of infection or inflammation of the pericardial sac (pericarditis) or due to bleeding from rupture of the heart wall or a coronary vessel (whether pathological or traumatic). Because the fibrous pericardium does not stretch much, the accumulation of fluid within it can impede the expansion of the heart chambers and prevent blood from moving through the heart and, ultimately, to the body. This condition is called cardiac tamponade and is an emergent situation.
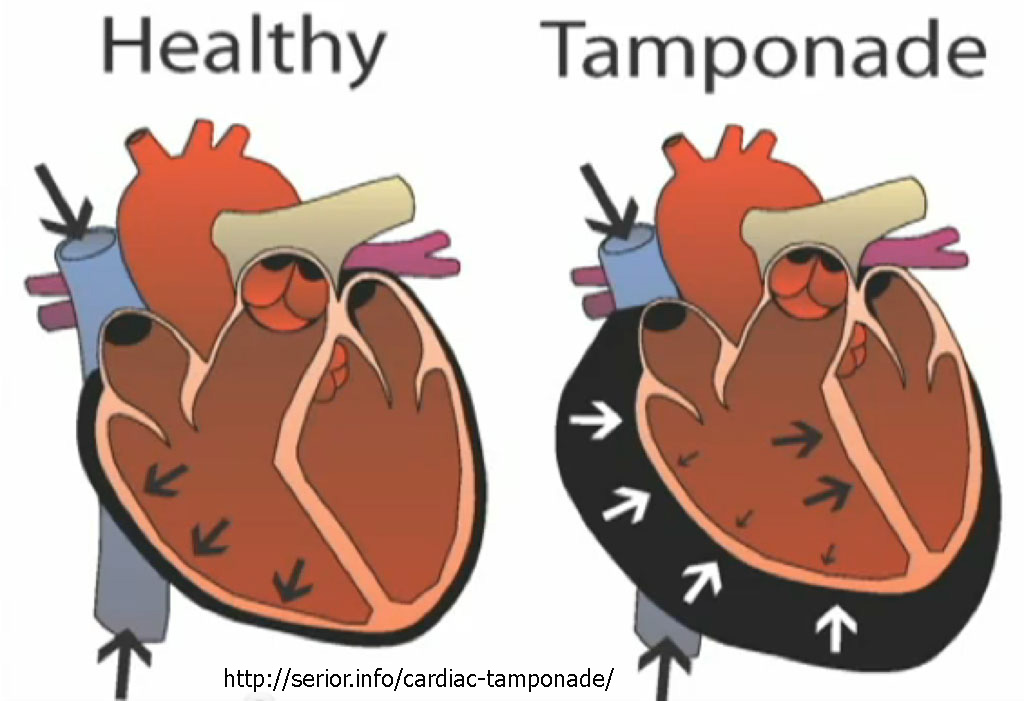
To remove fluid from the pericardial sac, a procedure called pericardiocentesis can be performed. During this procedure, a needle is angled through the thoracic wall into the distended pericardial sac and fluid is withdrawn. Anatomical landmarks are important for this procedure. The clinician palpates the xiphoid process of the sternum and the left costal margin (inferior edge of the ribs). They then insert a needle between the xiphoid process and left costal margin in a superior, posterior direction, angled slightly towards the left shoulder. Then they push the needle through the chest wall, penetrating the central tendon of the diaphragm to enter the pericardial sac from below. (The inferior surface of the pericardium is fused to the diaphragm.) Once the needle is within the pericardial sac, it is possible to remove fluid from the pericardial cavity and reduce the pressure on the heart.
Knowledge Checks
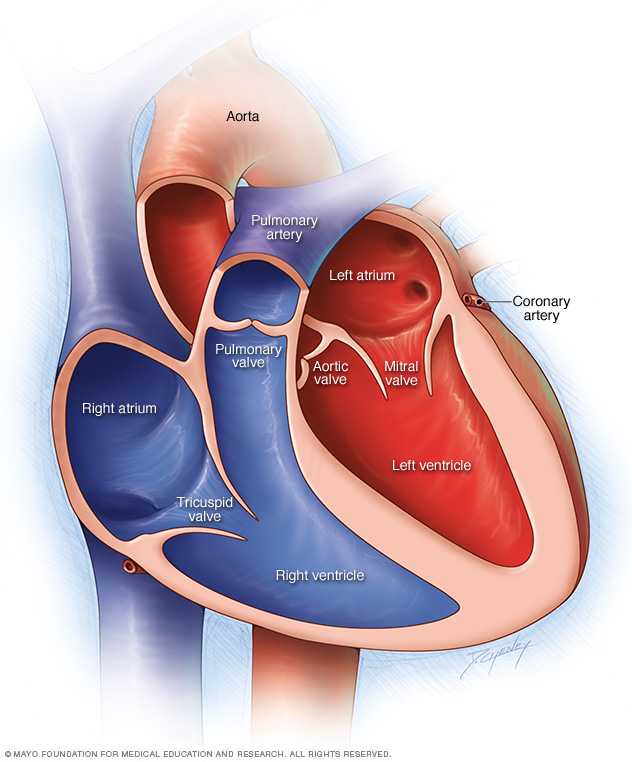
Internal Anatomy of the Heart
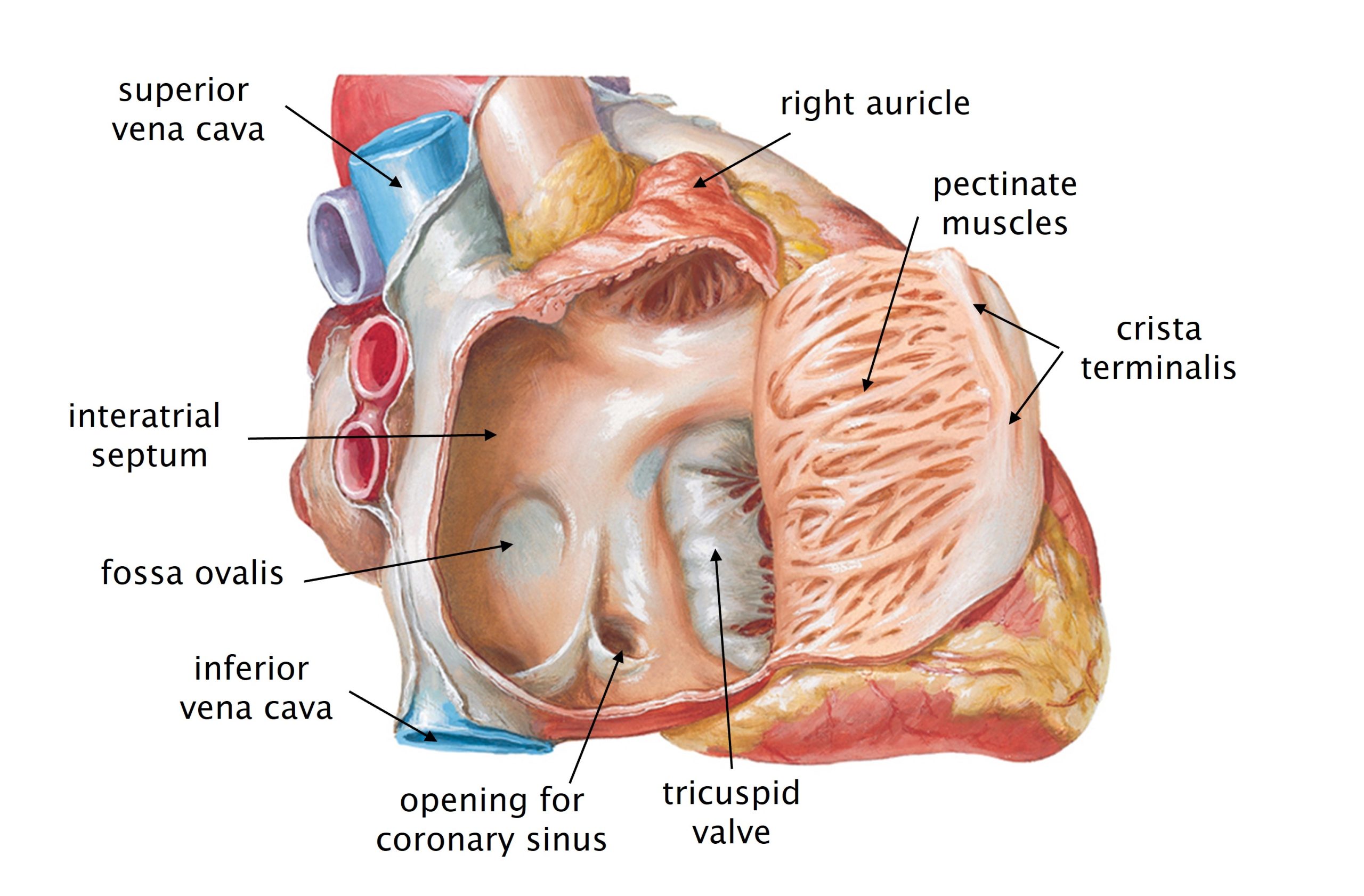
Right Atrium
The right atrium receives deoxygenated blood from the systemic and coronary circulations and sends blood to the right ventricle. The three major veins that enter the right atrium are:
- Superior vena cava is a large vein that carries deoxygenated blood from the head, upper limbs, and thorax.
- Inferior vena cava is a large vein that carries deoxygenated blood from the regions of body inferior to the thoracoabdominal diaphragm (abdomen, pelvis, perineum, and lower limbs).
- The coronary sinus is a smaller vein that carries deoxygenated blood from the walls of the heart itself.
- Some small cardiac veins empty directly into the right atrium, via microscopic openings in the chamber wall: the anterior cardiac veins and smallest cardiac veins. (We will not see these tiny vessels.)
The interior surface of the walls of the right atrium has some distinctive features.
- The right atrium is separated from the left atrium by the interatrial septum.
- Typically, blood does not flow directly between the right and left atria. (In some heart malformations, it does. More about that in Human Family Tree block.)
- In the right atrium, the interatrial septum is smooth and contains a depression called the fossa ovalis (“oval depression” in Latin).
- The fossa ovalis is the remnant of a structure in the developing fetus which shunted blood from the right to the left atrium in order to bypass the pulmonary circulation. This shunt typically closes at birth, but may remain patent in some individuals. We will study more about fetal circulation in the Human Family Tree block.
- Much of the rest of the internal surface of the right atrium is covered with parallel ridges called pectinate muscles.
- There is a prominent ridge in the right atrial wall at the junction between the smooth part of the wall and the pectinate muscles. This ridge is called the crista terminalis (“terminal crest”).
- This ridge marks the junction of two different tissues which form the right atrium in embryonic development.
- There is a prominent ridge in the right atrial wall at the junction between the smooth part of the wall and the pectinate muscles. This ridge is called the crista terminalis (“terminal crest”).
- Anteriorly, there is an outpouching of the right atrium which is called the right auricle or right atrial appendage. The interior walls of the auricle are rough with pectinate muscles.
- Blood leaves the right atrium through the right atrioventricular valve (tricuspid valve) to reach the right ventricle.
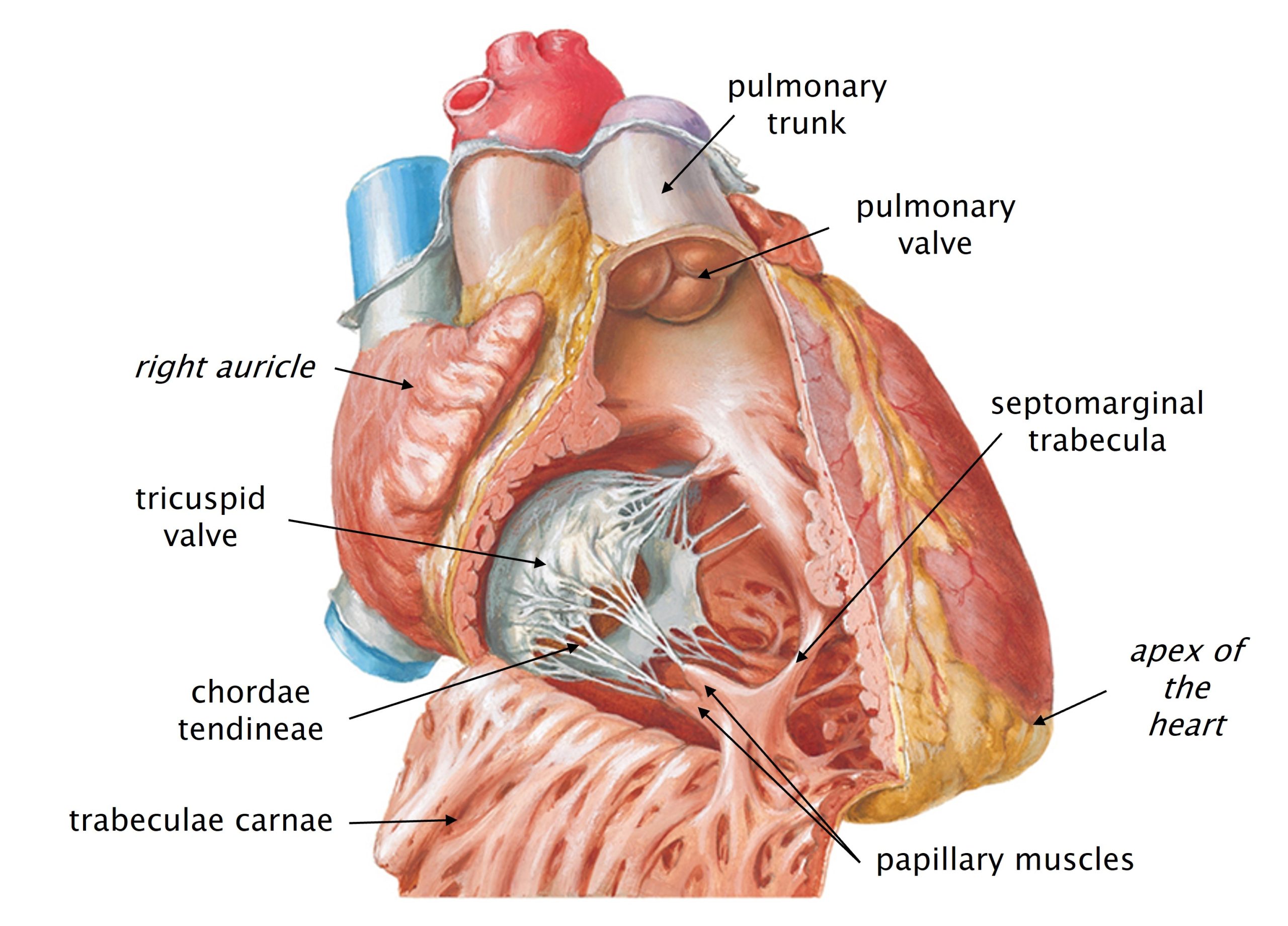
Right Ventricle
The right ventricle receives deoxygenated blood from the right atrium and sends blood out the pulmonary (pulmonic) trunk.
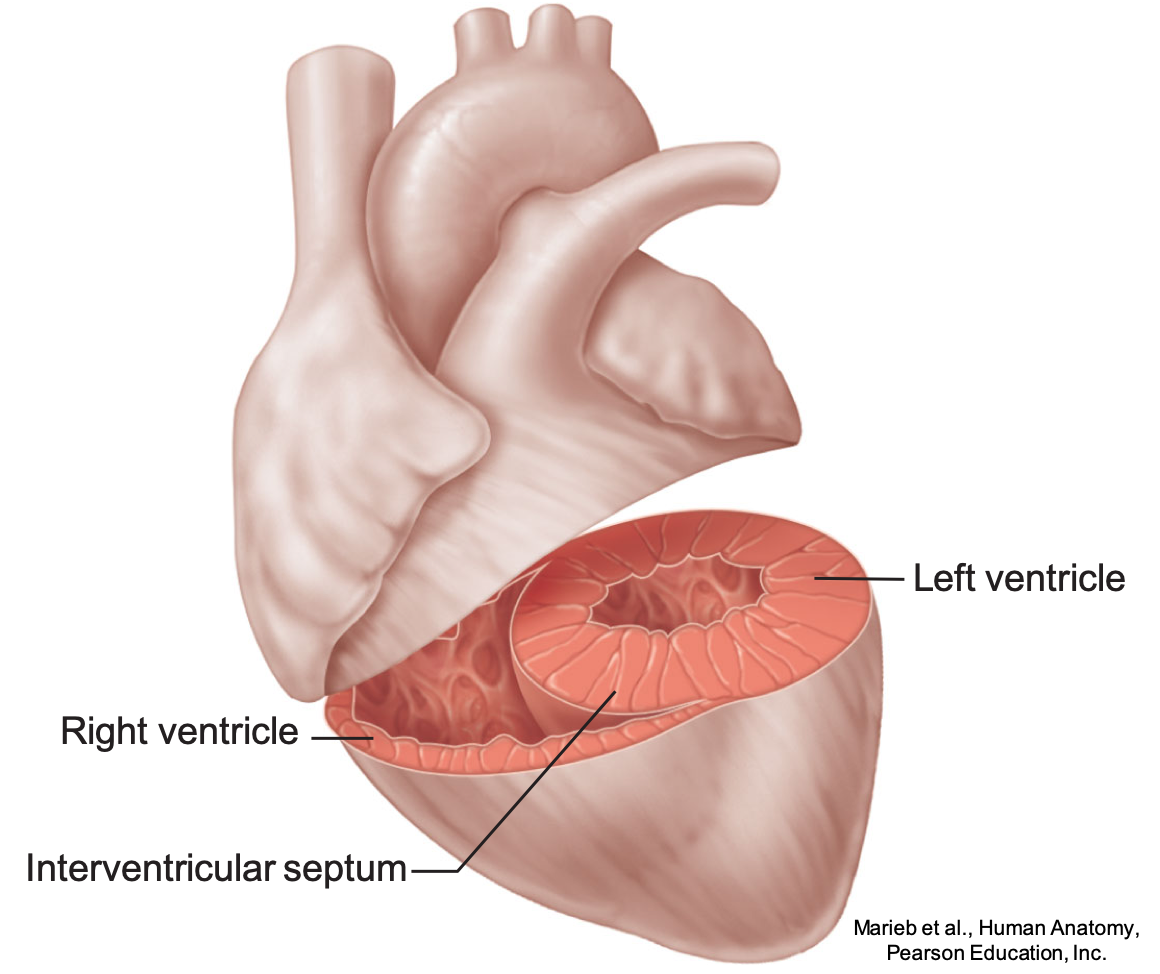
The right and left ventricles are separated by a thick interventricular septum. Most of the septum and the walls of the ventricles are made of cardiac muscle.
- Blood does not travel directly between the right and left ventricles. (In some heart malformations, it does. More about that in Human Family Tree block.)
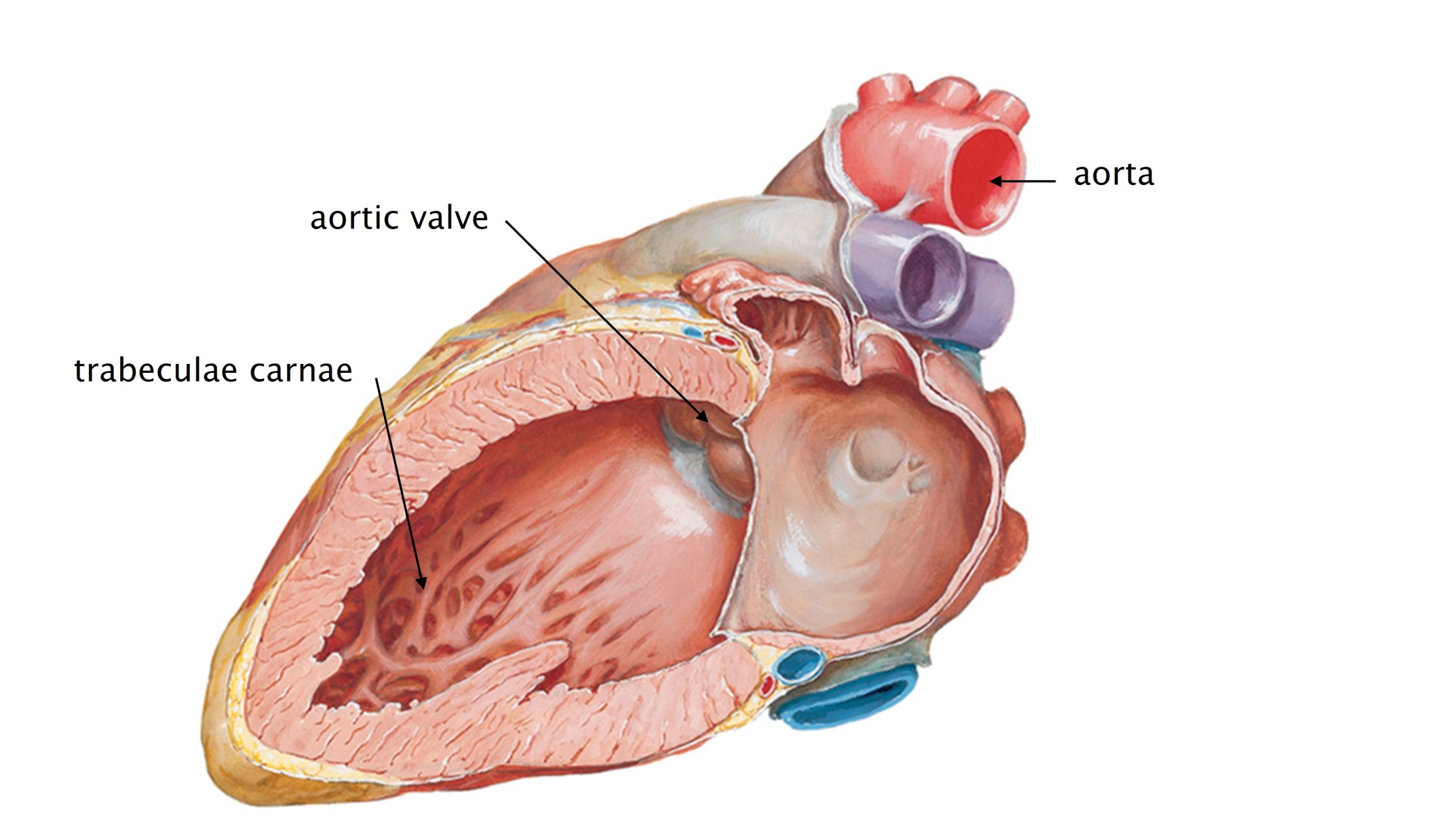
- The walls of the right ventricle are rough internally with ridges of cardiac muscle called trabeculae carnae (“small beams of meat” in Latin; if that helps…)
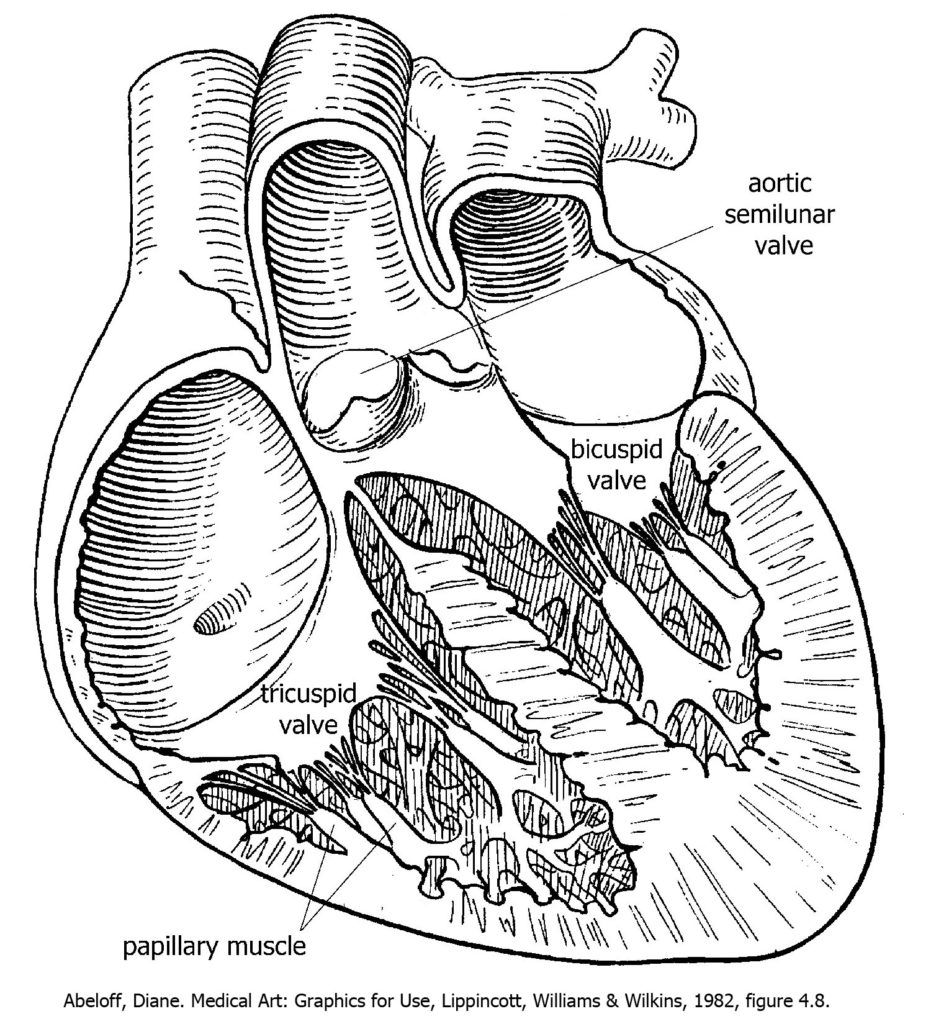
Blood enters the right ventricle through the right atrioventricular valve (tricuspid valve).
- The three leaflets of the tricuspid valve are attached to papillary muscles with tiny tendons called chordae tendineae. Papillary muscles protrude from the ventricular wall and are made of cardiac muscle.
- Chordae tendineae are the cutest tendons in the body!
- The anterior-most papillary muscle is connected to the interventricular septum by a distinctive band of cardiac muscle called the septomarginal trabecula (or moderator band). This structure is the only part of the electrical conduction system of the heart that is grossly visible.
Contraction of the right ventricle pushes blood through the pulmonary semilunar valve (also called the pulmonic valve) into the pulmonary trunk, a large artery which splits into the right and left pulmonary arteries that enter each lung. (The arteries of the pulmonary circulation are the only arteries in the body that carry deoxygenated blood.)
- The muscle layer in the wall of the right ventricle is thinner than that of the left ventricle because the pulmonary circulation is relatively small and low pressure. The right ventricle does not have to generate as much force as the left ventricle does, so the muscular wall is thinner. In cases of pulmonary hypertension, when the pressure in the lungs is higher than normal, the wall of the right ventricle can become quite a bit thicker.
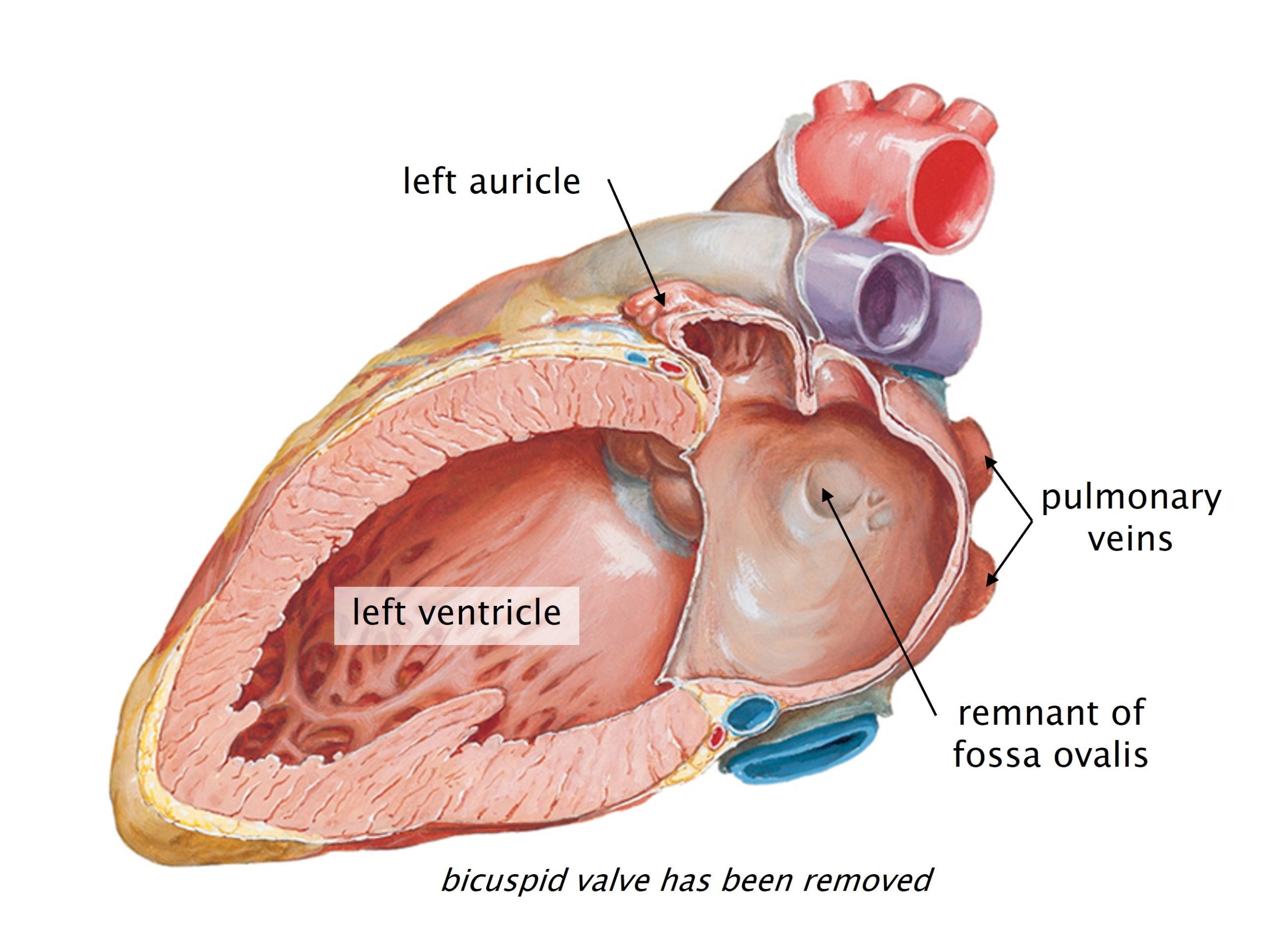
Left Atrium
The left atrium receives oxygenated blood from the pulmonary circulation through four pulmonary veins (two from each lung) and sends blood to the left ventricle.
Most of the interior wall of the left atrium has smooth walls, but the walls of the anteriorly-projecting left auricle (left atrial appendage) are rough with pectinate muscles.
- On the interatrial septum on the left side, you may see a remnant of the fetal shunt that made the fossa ovalis in the right atrium.
Blood leaves the left atrium through the left atrioventricular valve (bicuspid, or mitral, valve) to enter the left ventricle.
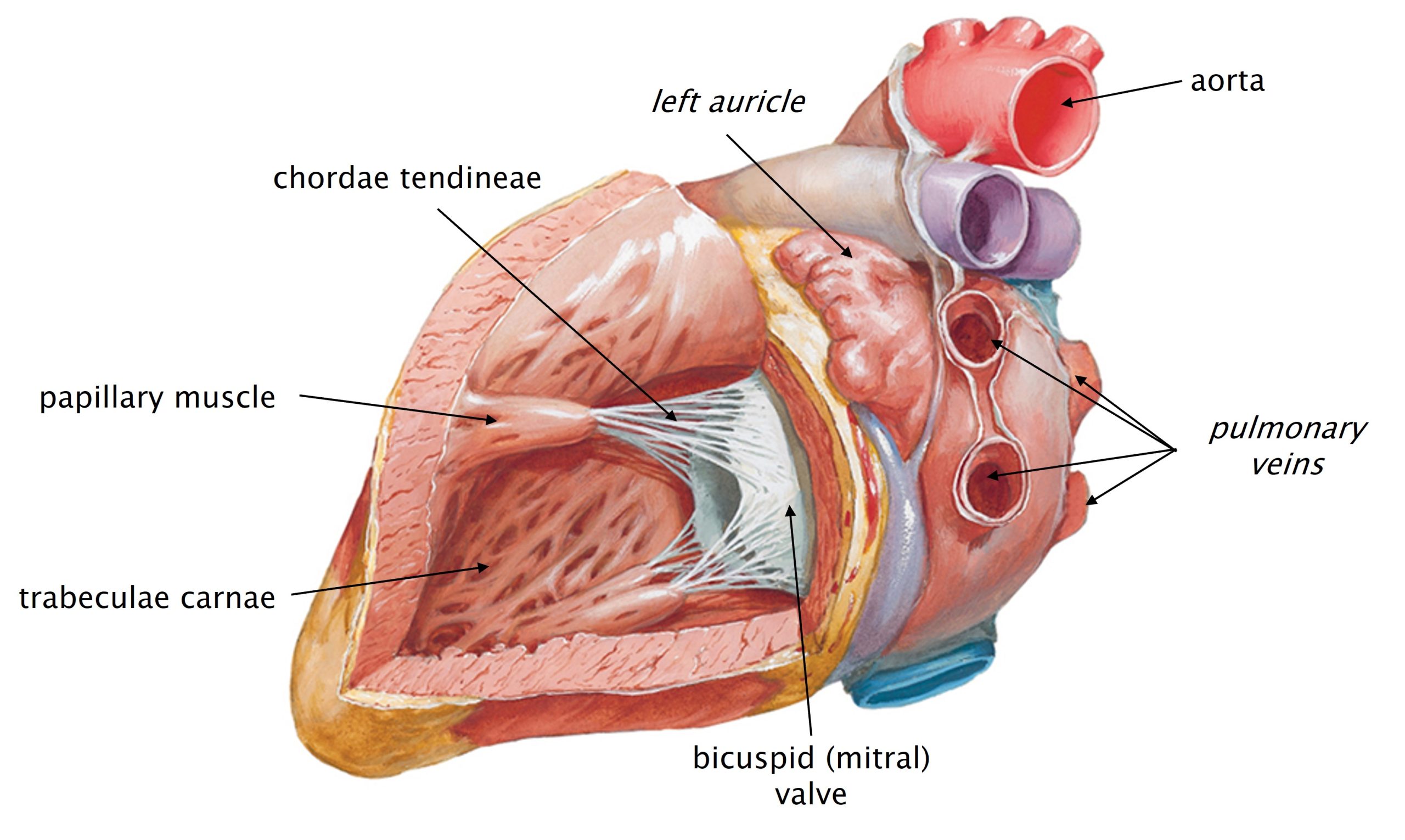
Left Ventricle
The left ventricle receives oxygenated blood from the left atrium and sends it out the aorta, a very large artery that supplies oxygenated blood to the entire systemic and coronary circulations.
Blood enters the left ventricle through the left atrioventricular valve (bicuspid valve or mitral valve).
- As in the right ventricle, the two leaflets of the bicuspid valve are attached to papillary muscles in the ventricular wall by tiny tendons (chordae tendineae).
Like the right ventricle, the internal walls of the left ventricle contain trabeculae carnae. In the left ventricle, the muscular wall is substantially thicker (~2.5 times) than that of the right ventricle. The left ventricle generates greater force when it contracts in order to push blood against the resistance in the aorta and systemic circulation. This difference in wall thickness typically makes it easy to differentiate between the two ventricles.
Contraction of the left ventricle pushes blood through the aortic semilunar valve and into the proximal aorta. From the proximal aorta, blood can enter either the coronary circulation or the systemic circulation. To reach the coronary circulation, blood enters the right or left coronary artery. These arteries are the first branches off of the aorta. (The heart feeds itself first!) Most of the blood that leaves the left ventricle continues through the aorta to reach the rest of the body.
Review of Circulation of Blood through the Heart
To review, deoxygenated blood flows from the systemic and coronary circulations into the heart through the superior vena cava, inferior vena cava, and coronary sinus to enter the right atrium. From the right atrium, blood flows through the tricuspid valve into the right ventricle. From the right ventricle, blood flows through the pulmonary semilunar valve into the pulmonary trunk which goes to the lungs.
Blood is oxygenated in the lungs.
Oxygenated blood flows from the lungs through the four pulmonary veins into the left atrium. From the left atrium, blood flows through the bicuspid (mitral) valve into the left ventricle. From the left ventricle, blood flows through the aortic semilunar valve into the proximal aorta. From the proximal aorta, blood can enter the coronary circulation, through the right and left coronary arteries, or can enter the systemic circulation by continuing through the aorta to the rest of the body.
Knowledge Check
Valves of the Heart
The efficient, one way flow of blood through the chambers of the heart depends on the presence of the four valves of the heart. All four of the valves attach to the cardiac skeleton, a dense connective tissue framework that surrounds the valves.
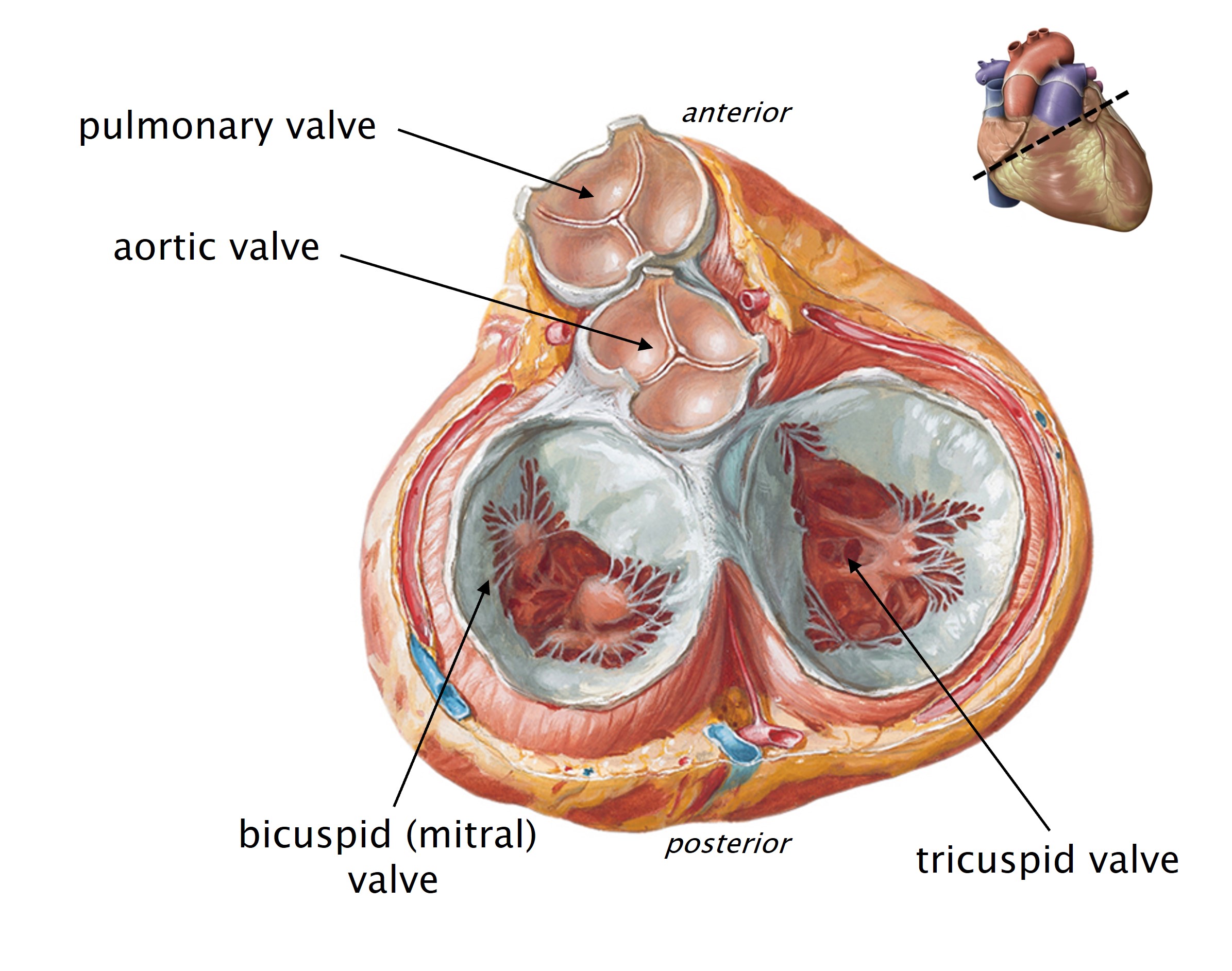
- Between the atria and ventricles are the right and left atrioventricular valves.
- Tricuspid valve between the right atrium and ventricle.
- Bicuspid (mitral) valve between the left atrium and ventricle.
- At the bases of the pulmonary trunk and aorta are two semilunar valves.
- Pulmonary valve between the right ventricle and pulmonary trunk.
- Aortic valve between the left ventricle and aorta.
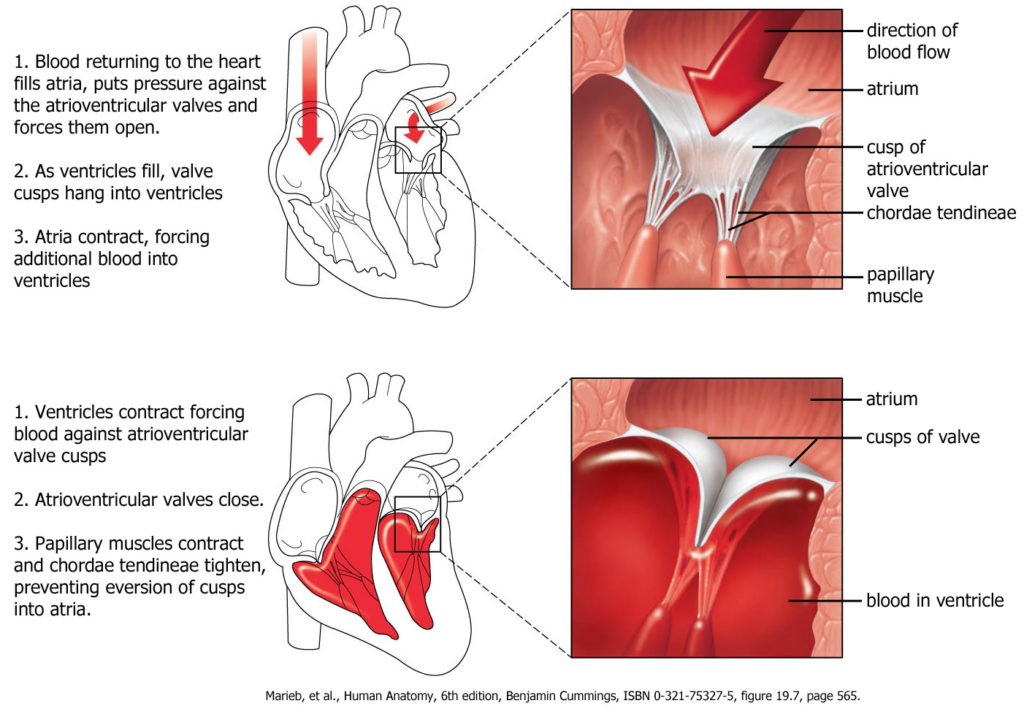
Atrioventricular Valves (Bicuspid and Tricuspid Valves)
The atrioventricular valves (bicuspid and tricuspid) have two or three leaflets (“cusps”) which are flaps of connective tissue that project into the ventricles. When the ventricles contract, the force of the blood flow pushes the cusps up toward the atrium, closing off the path between the atrium and ventricle and preventing blood from flowing “backwards.” Instead, blood flows from the ventricles into the pulmonary trunk or aorta.
Each of the cusps of the tricuspid and bicuspid valves are attached to papillary muscles in the ventricle by chordae tendineae. When the ventricles contract, the papillary muscles also contract, putting tension on the chordae tendineae and preventing the valve cusps from everting into the atria.
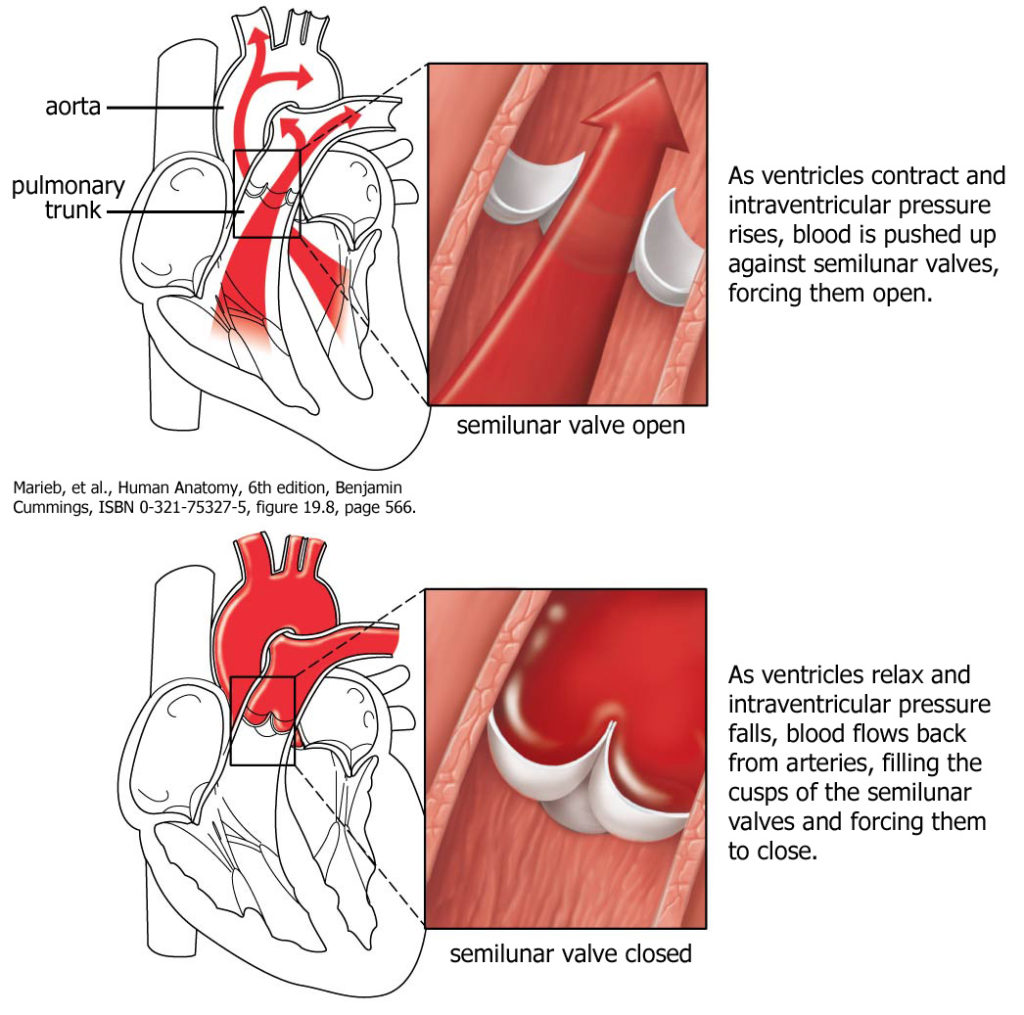
Aortic and Pulmonary Valves (Semilunar Valves)
The semilunar valves between the ventricles and the aorta and pulmonary trunk have a different structure than the atrioventricular valves. The aortic and pulmonary valves are each formed by three semilunar, cup-shaped flaps of tissue that protrude into the lumen of the aorta and pulmonary trunk. As illustrated below, when the ventricles relax, blood flows backward a little bit from the aorta and pulmonary trunk, filling these tiny cups with blood. As the cups fill, they protrude into the lumen of the vessel, closing it off and preventing backflow into the ventricles. (There are tiny nodules at the edges of the cups which meet when the valves close and make a semi-rigid structure. Look for them in your heart dissection.)
Clinical Application: Mitral Stenosis
Mitral stenosis is a narrowing of the opening of the mitral (bicuspid) valve. The most common cause of mitral stenosis is rheumatic fever though the stenosis happens gradually and usually does not become clinically significant for several decades. The leaflets of the bicuspid valve undergo an initial phase of inflammation, which is followed by a more protracted phase of scarring (fibrosis). Extensive fibrosis thickens and distorts the valve leaflets. These fibrotic changes reduce the pliability of the leaflets, causing an narrow, crescent-shaped opening to persist in the closed valve. This is called mitral insufficiency.
The aortic and tricuspid valves may be similarly involved in patients with rheumatic heart disease. The pulmonary valve is the least likely to be damaged.
Knowledge Check
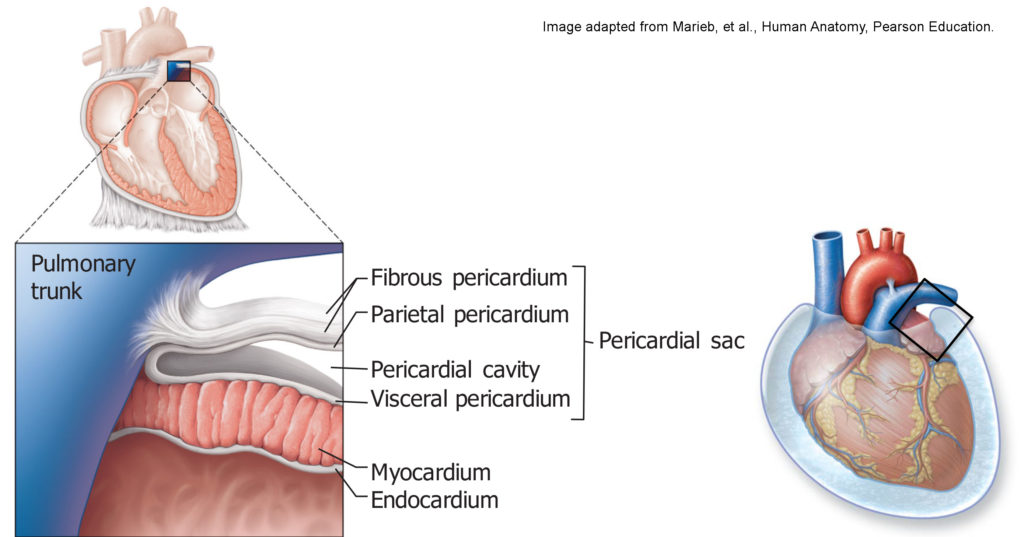
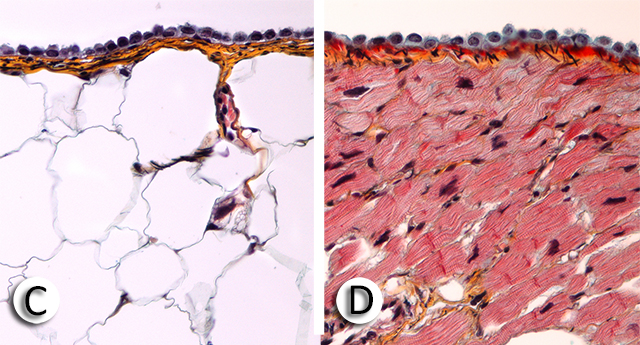
Overview of Histology of the Heart: Three Layers
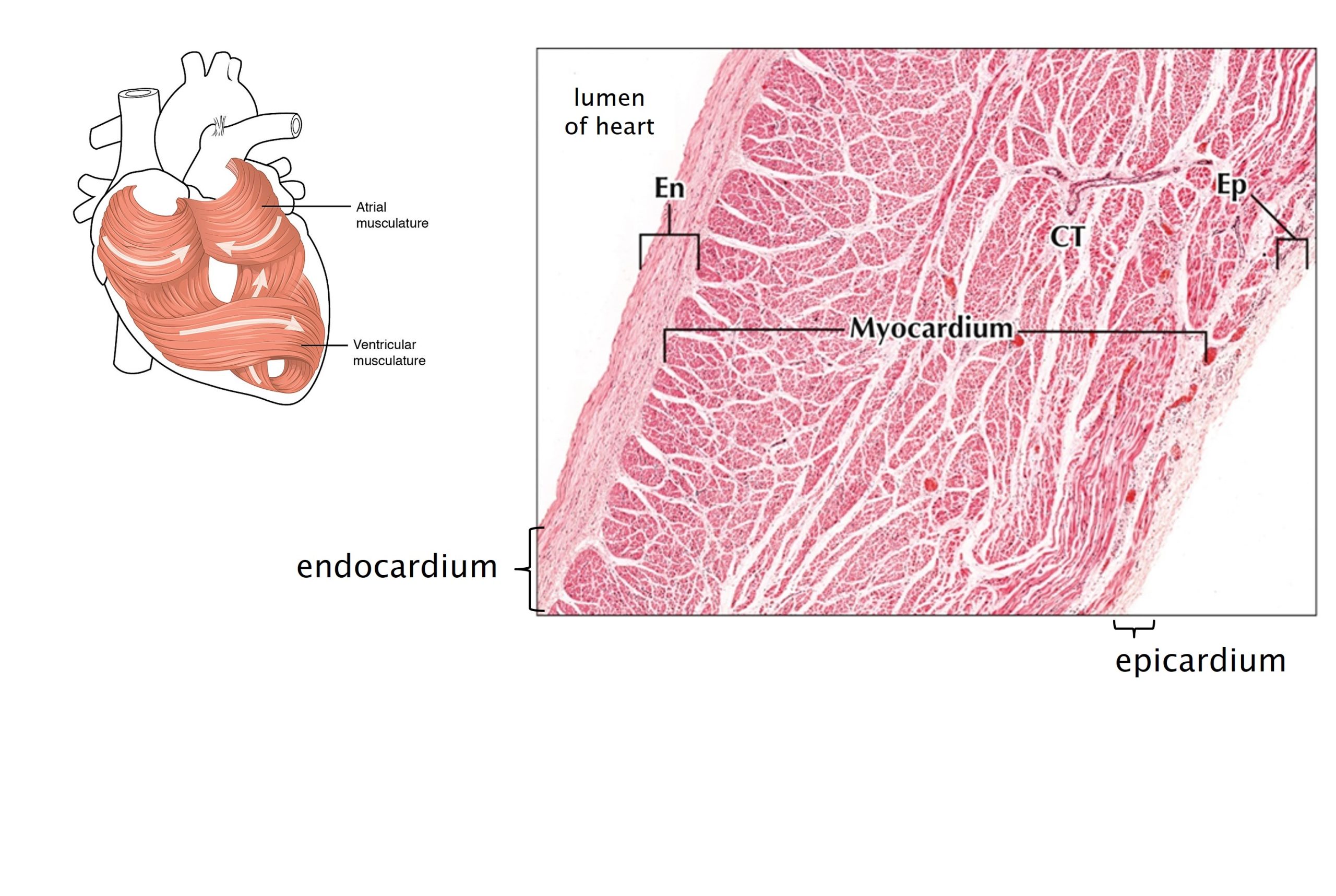
There are three layers in the wall of the heart from superficial to deep, the epicardium, myocardium and endocardium.
Epicardium
Epicardium is the outermost layer of the heart wall. Epicardium is the visceral pericardium. It is comprised of a mesothelium and an underlying layer of loose connective tissue with varying amounts of adipose tissue. You can use the terms epicardium and visceral pericardium interchangeably.
Branches of the coronary arteries and cardiac veins travel through the connective tissue of the epicardium.
Myocardium
Myocardium is the middle layer of the heart wall. It is the thickest of the three layers and consists of bundles of cardiac muscle cells (myocytes). These muscle cells are attached to a cardiac “skeleton,” a fibrous framework that encircles the valves and gives the heart its form. Muscle cells in the myocardium are roughly organized into a spiral around the chambers. When they contract, this arrangement of muscle fibers effectively squeezes blood out of the chambers. Because of this orientation, histological sections through the myocardium show many different orientations of cardiac muscle cells.
In the atria, the myocardium is thinner than in the ventricles. The atria require less muscular walls because, in moving blood to the ventricles, they do not work against peripheral resistance and need to generate less force.
Specialized cardiac muscle cells make up the conducting system of the heart. These cells conduct electrical impulses, rather than contract. These specialized cells make up the sinoatrial (SA) node, atrioventricular (AV) node, and the atrioventricular (AV) bundle (also known as the bundle of His). Other fibers of the conducting system run just deep to the endocardium. These are called Purkinje fibers.
Endocardium
Endocardium is the innermost layer of the heart wall. It is comprised of a layer of specialized simple squamous epithelium, endothelium, and a layer of loose connective tissue.
- Endothelium is a specialized simple squamous epithelium that lines all of the spaces in the body that contact blood. This includes all of the heart chambers and valves; the linings of all arteries, veins, and capillaries; and the erectile tissues of the body. The endocardium of the heart is continuous with the endothelium that lines the blood vessels that enter and leave the heart.
- Some fibers of the conducting system (Purkinje fibers) pass through the thin layer of connective tissue between the endocardium and myocardium in the walls of the ventricle.
Knowledge Checks
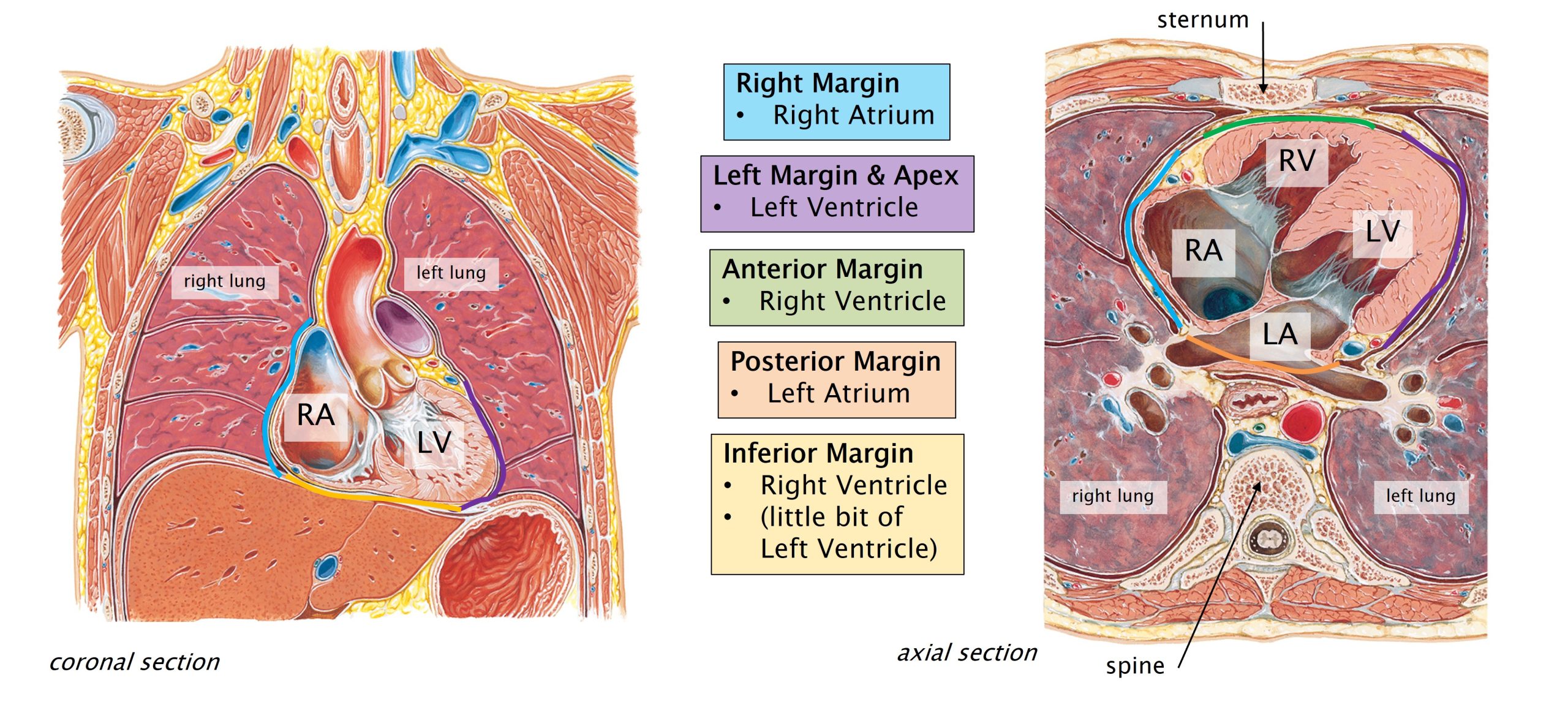
Heart In Situ
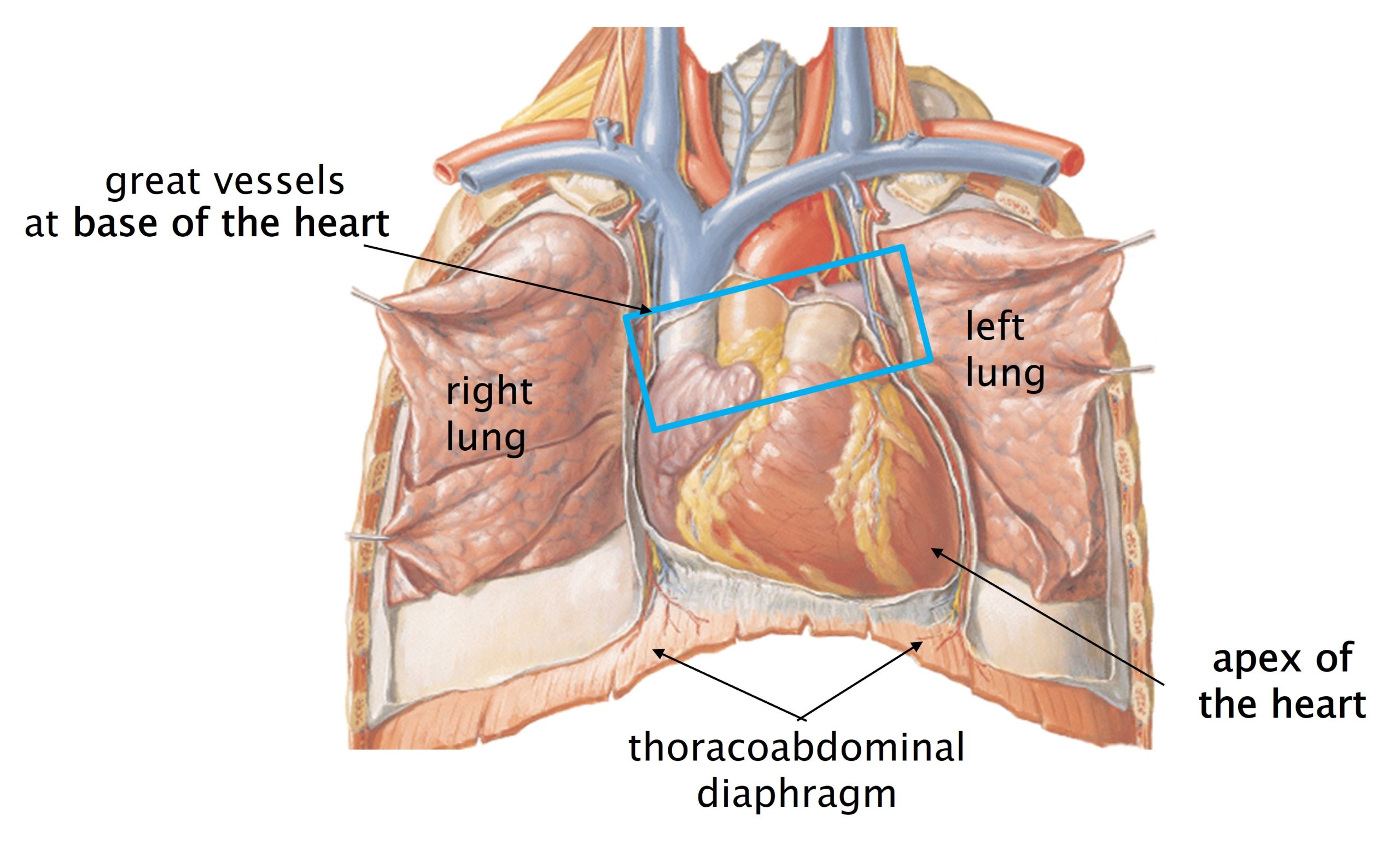
Once you understand the internal anatomy of the heart and circulation of blood, it’s important to understand how the heart sits inside the thorax and how it relates to other structures there. The heart sits somewhat on its side within the thorax. The wide part of the heart, where the aorta and pulmonary trunk emerge from the ventricles, is defined as the base of the heart. The part of the heart that points inferiorly and to the left is the apex of the heart. (So, somewhat confusingly, the apex of the heart points down(ish) and the base of the heart is superior to the apex.)
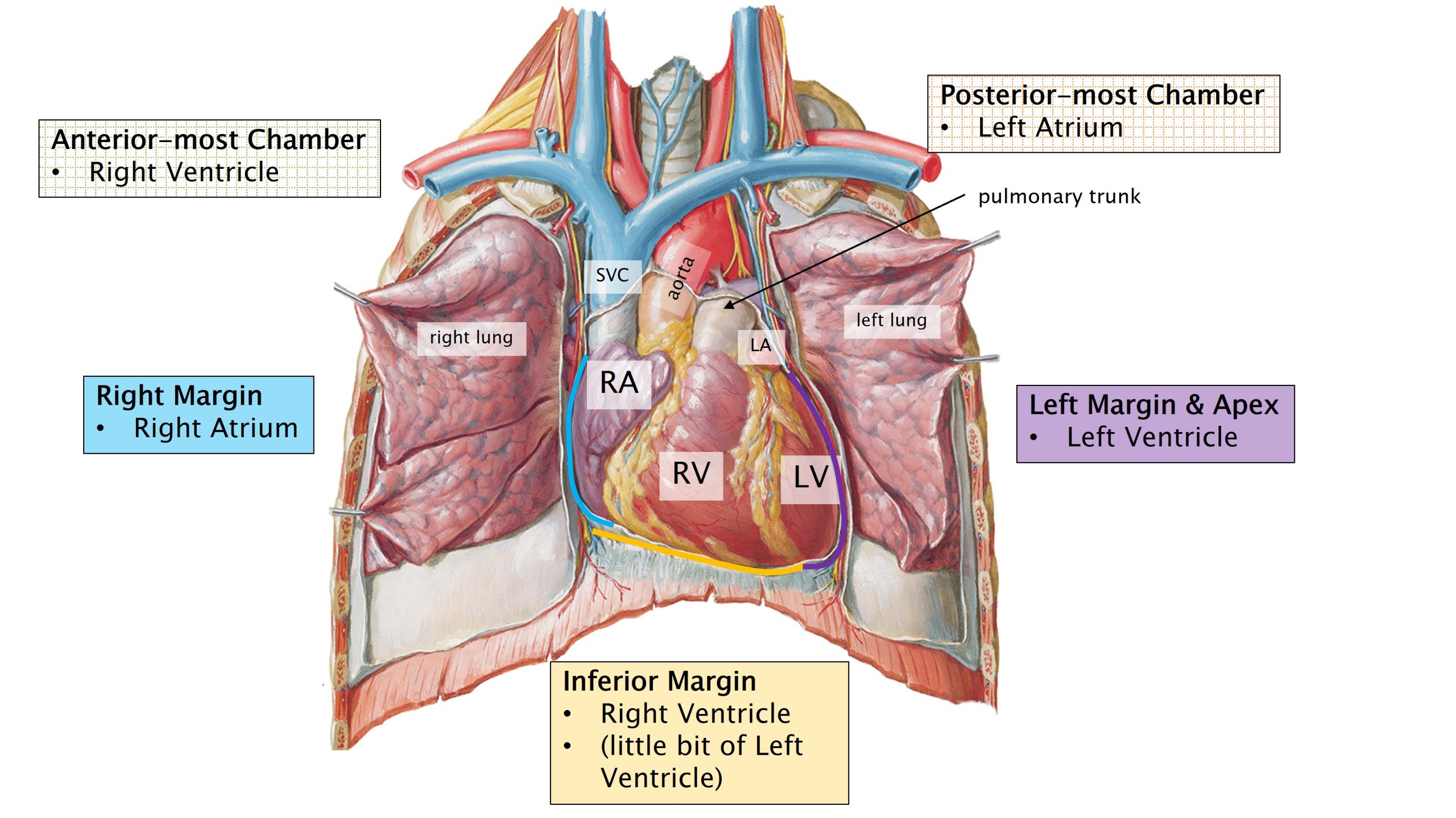
- As you can see in the figures above, the right ventricle of the heart makes up most of its anterior surface.
- In your dissection, when you remove the anterior thoracic wall, the right ventricle is the chamber that sits just deep to the sternum.
- Chest compressions use this anatomical relationship to transfer force from the bony sternum to the underlying right ventricle and pump blood through the heart manually.
- In your dissection, when you remove the anterior thoracic wall, the right ventricle is the chamber that sits just deep to the sternum.
- The left ventricle makes the left margin and the apex of the heart.
- The right atrium makes the right margin of the heart.
- From an anterior view, the left atrium is not visible. It is the most posterior of the four chambers.
- Of the great vessels, the aorta, pulmonary trunk, and superior vena cava enter/exit the heart from its superior side, at the base of the heart.
These relationships are important in orienting yourself on your dissections and on the hearts that you will remove. These relationships are also crucial in orienting yourself in radiologic images of the heart. In the images above, the thorax has been cut in coronal and axial (horizontal) sections. For all imaging, remember that the image is oriented as if you are looking at a patient. In a axial section, orient yourself as if you are looking up from below (from the patient’s feet toward the head; the patient is assumed to be supine).
- Image left is patient right. Image right is patient left.
- In an axial section, the superior part of the image is the anterior body; inferior on the image is posterior.
Margins of the heart:
- The right margin of the heart is formed by the right atrium.
- The left margin of the heart is formed by the left ventricle.
- The anterior margin (just deep to the sternum) is formed by the right ventricle.
- The posterior border is formed by the left atrium.
- The inferior surface of the heart (which sits on the thoracoabdominal diaphragm) is formed by the left and right ventricles.
Knowledge Check
Surface Anatomy of the Heart
To understand the position of the heart within the thorax, you need to know some key bony landmarks of the thorax.
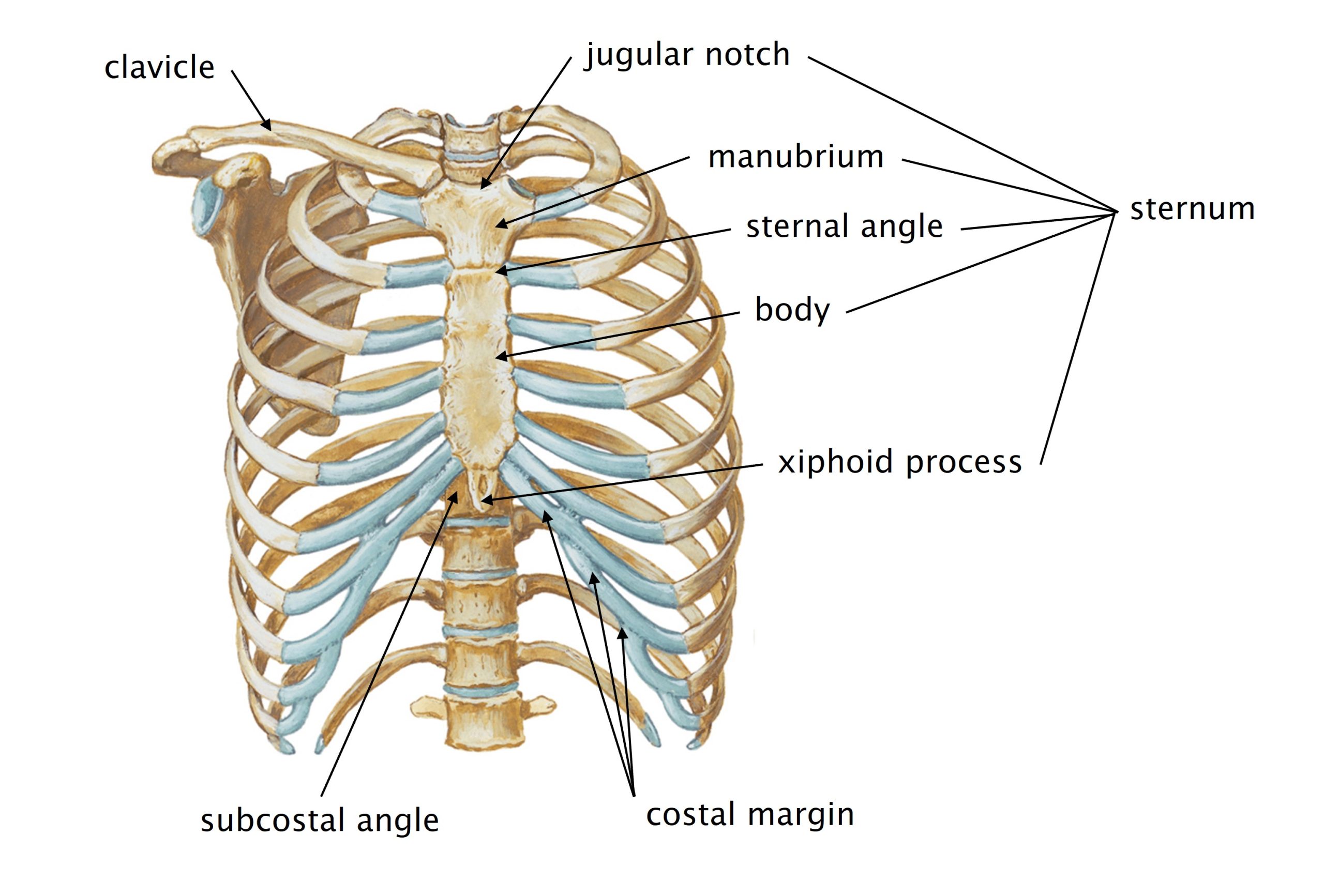
- Sternum: This mid-line bone is palpable for its entire length.
- Jugular (suprasternal or sternal) notch: the superior edge of the sternum.
- Manubrium: the superior 1/3 of the bone; ends at the second rib.
- Body of the sternum: the inferior 2/3 of the bone; ends at the xiphoid process.
- Sternal angle (of Louis): the junction between the manubrium and body of the sternum.
- You can feel a slight bulge in the bone at the sternal angle.
- This is a good landmark for the level of the second rib.
- Xiphoid process: cartilaginous section of the sternum
- Often ossifies (turns to bone) with age.
- Subcostal angle: angle between the xiphoid process and the costal margin (inferior edge of the rib cage).
- Clavicle: This bone is palpable for its entire length from the sternum to the point of the shoulder.
- The mid-clavicular line is a good landmark. It is the point that would bisect the clavicle.
- The nipple is approximately at the mid-clavicular line.
- The mid-clavicular line is a good landmark. It is the point that would bisect the clavicle.
- Ribs:
- The ribs are numbered from 1-12 beginning superiorly.
- Intercostal spaces are the spaces between the ribs. They are numbered according to the rib that is superior to the space.
- So, the second intercostal space is just inferior to the second rib.
- Costal cartilages are hyaline cartilage that connect the ends of the bony ribs to the sternum.
- The inferior-most costal cartilages (just lateral to the xiphoid process) are from the seventh ribs.
- The costal cartilages of ribs 8-12 do not reach the sternum. These are called ‘false ribs.’
- Ribs 11-12 generally have no costal cartilages and end in soft tissue. These are called ‘floating ribs.’
- The left and right costal margins are the inferior edges of the rib cage.
Surface Projections of the Heart
Surface projections of the heart are important in clinical practice. It is important to understand what surface landmarks to use to approximate the position of the heart within the thorax. As you will see in your dissections, hearts vary in size (and shape) by individual, but these guidelines are helpful in approximating the position of the heart by using surface landmarks.
Use the figure below, and the descriptions provided, to understand where the heart sits based on surface landmarks.
Notes on terminology:
- Remember that the right side of the image is the patient’s left side, and vice versa. When we talk about anatomy, we’re always talking about the patient’s right or left.
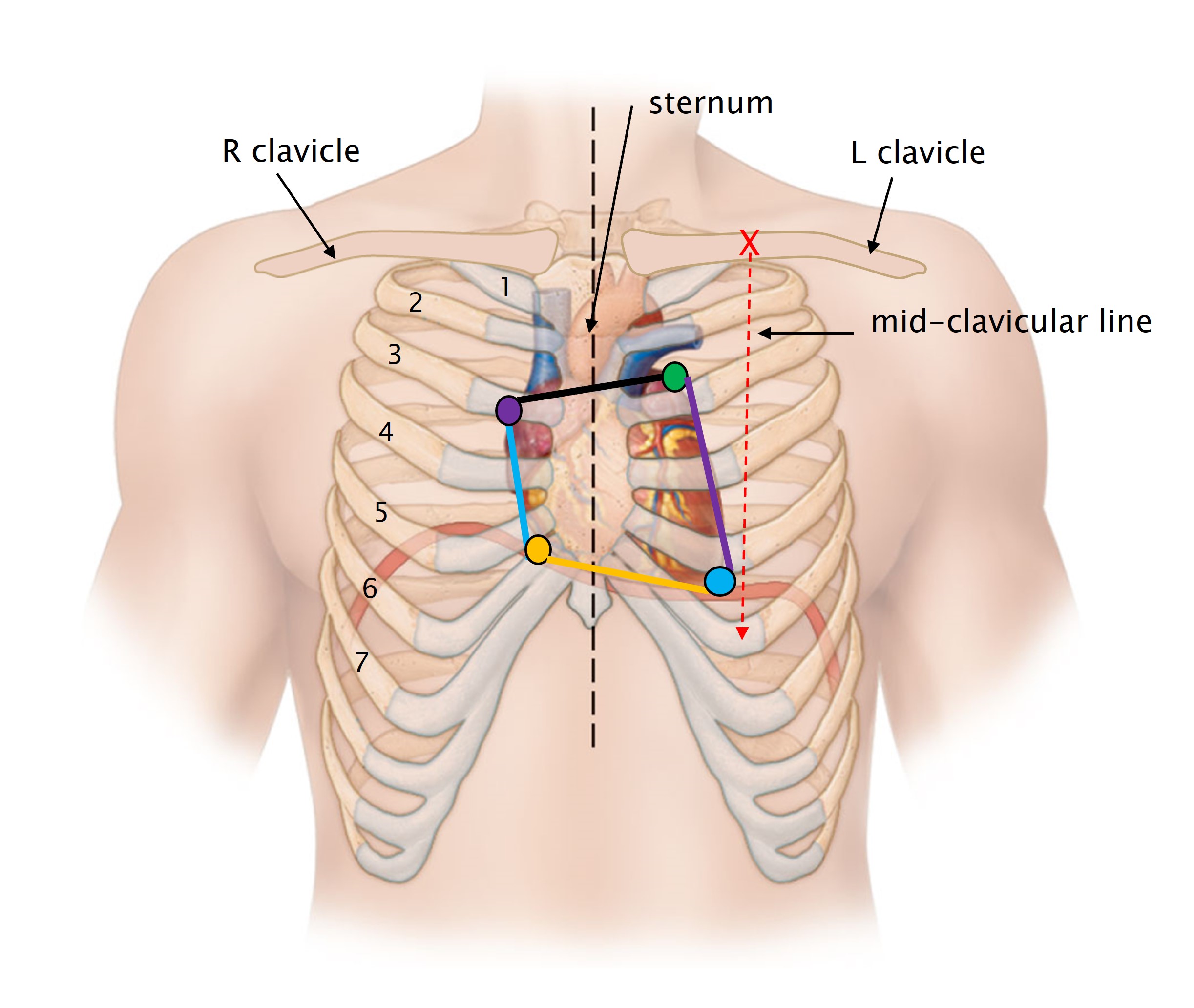
You can draw the approximate outline of the heart on the surface of the thorax with lines connecting four points:
- Second left intercostal space, just lateral to the sternum (green)
- Third right costal cartilage, just lateral to the sternum (purple)
- Sixth right costal cartilage, just lateral to the sternum (yellow)
- Fifth left intercostal space, at the mid-clavicular line (blue)
Connect these points to form an outline of the heart and define the margins of the organ from the surface:
- Superior border of the heart: point 1 to point 2
- Line that extends slightly obliquely from the second left intercostal space to the third right costal cartilage.
- Right border of the heart: point 2 to point 3
- Line that extends approximately straight down from the third right costal cartilage to the sixth right costal cartilage.
- This line is located about 1/2 inch to the right of the sternum.
- Inferior border of the heart: point 3 to point 4
- Line that extends from the sixth right costal cartilage to the fifth left intercostal space at about the mid-clavicular line.
- The fifth left intercostal space at the mid-clavicular line is approximately the location of the apex of the heart.
- Left border of the heart: point 4 to point 1
- Line that extends obliquely from the fifth left intercostal space at the mid-clavicular line to the second left intercostal space.
Understanding the surface projection of the heart can be important in cases of a penetrating wound to the thorax. For example, a penetrating wound to the fifth intercostal space two inches lateral to the left border of the sternum could involve the heart. A similar wound to the fifth intercostal space on the right side of the sternum would be less likely to involve the heart.
Knowledge Checks
Clinical Application: Anatomical Basis for Auscultation Points (Heart sounds)
Normal contraction of the heart produces two sounds, lub (S1) and dup (S2). These sounds are produced by the closure of the heart valves.
- The first sound (lub) is produced by the closure of the atrioventricular valves at the start of systole.
- The second sound (dup) is produced by the closure of the aortic and pulmonic valves at the end of systole.
Each valve sound is heard best at a particular location on the chest wall. The auscultation points do not correspond exactly to the locations (surface projections) of the valves. (The valves are mostly located retrosternally, making it difficult to hear them through the bone.) Each auscultation point corresponds to the region where the blood is going after it passes through a valve, as shown in the figure below. Remember there are individual variations in heart size and position, but this is a good general starting point.
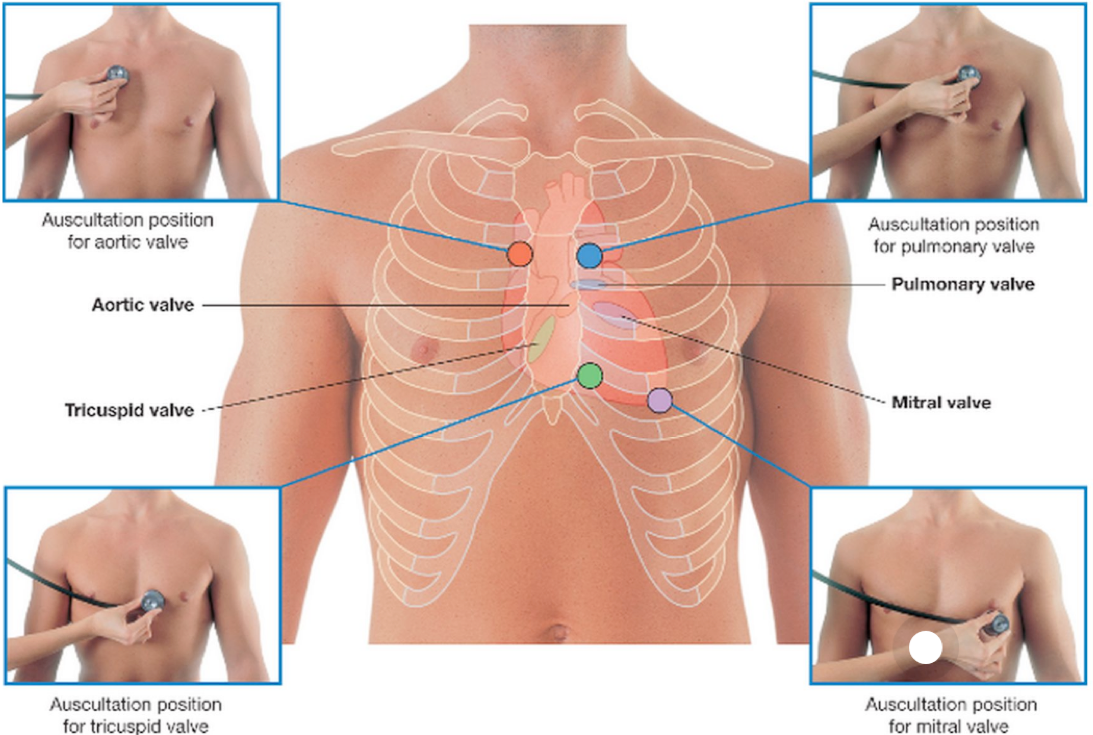
- The aortic valve (orange in the figure) is heard best over the second right intercostal space just lateral to the sternum. Deep to this location is the aorta: the destination of the blood going through the aortic valve.
- The pulmonary valve (blue) is best heard over the second left intercostal space, a location just superficial to the pulmonary trunk.
- The tricuspid valve (green) is best heard over the fifth left intercostal space, just to the left of the xiphoid process (over the right ventricle).
- The mitral valve (purple) is heard best at the fifth left intercostal space, over the apex of the heart (left ventricle), .
Coronary Circulation
The coronary circulation delivers nutrient- and oxygen-rich blood to the tissue of the heart walls via coronary arteries and returns deoxygenated blood to the right atrium via cardiac veins.
Coronary Arteries
The right and left coronary arteries are the first branches off of the aorta, originating just distal to the aortic semilunar valve. The two coronary arteries give rise to all of the arteries that run through the epicardium on the external surface of the heart. The coronary arteries and their branches supply whatever region of the heart that they overlie, i.e. if the artery or branch sits over the right ventricle, it is supplying the right ventricle.
Below is a description and image of a “typical” branching pattern of the coronary arteries. Keep in mind that there are many individual variations in these patterns. Ultimately, as long as blood gets to the tissues of the heart, it does not matter what pathway blood takes. You will see many variations in the lab.
- The left coronary artery arises from the left side of the aorta. It is typically very short and branches into two large arteries after passing between the pulmonary trunk and the left auricle. The two main branches of the left coronary artery are:
- The anterior interventricular artery (also called the left anterior descending artery (LAD)) travels down the anterior surface of the heart over the interventricular septum.
- It supplies the right and left ventricles and the muscular interventricular septum on the anterior side.
- The circumflex artery travels to the posterior side of the heart within the coronary sulcus (the groove on the external surface of the heart which separates the atria from the ventricles).
- It supplies the left atrium and left ventricle.
- The anterior interventricular artery (also called the left anterior descending artery (LAD)) travels down the anterior surface of the heart over the interventricular septum.
- The right coronary artery arises from the right side of the aorta. It has a longer course than the left coronary artery does. It travels in the coronary sulcus toward the right margin of the heart. It has two main branches.
- At the right margin of the heart, the right (acute) marginal artery branches off and runs on the right border of the heart.
- It supplies the right ventricle.
- The right coronary artery continues to the posterior side of the heart in the coronary sulcus. It ends as the posterior interventricular artery which travels over the interventricular septum on the posterior heart.
- It supplies the right and left ventricles and the posterior portion of the muscular interventricular septum.
- Additional small branches of the right coronary artery supply the right atrium as well as the SA node (via the sinoatrial nodal artery). We will not see these smaller branches in the lab, but you should understand that they exist.
- At the right margin of the heart, the right (acute) marginal artery branches off and runs on the right border of the heart.
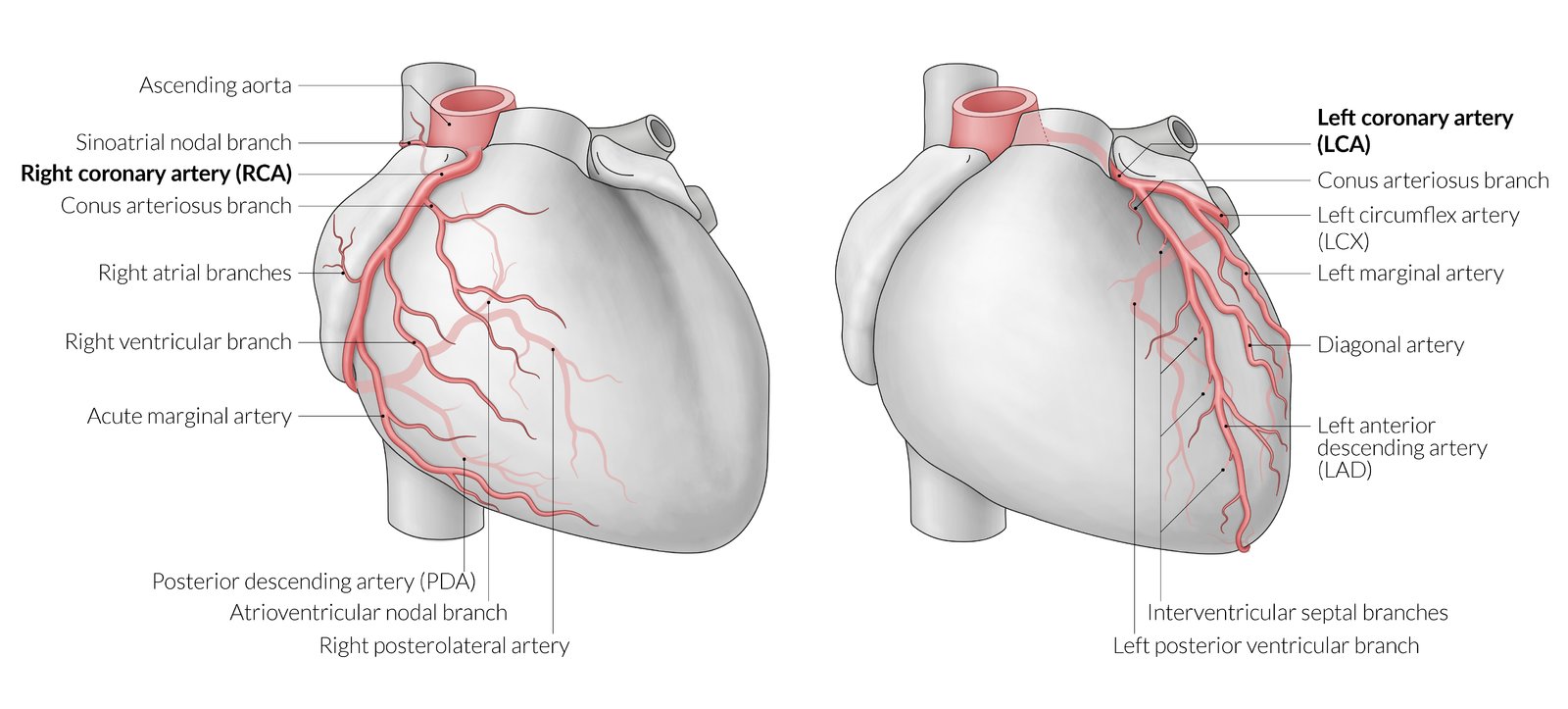
Right and left coronary arteries and branches. From https://www.amboss.com/us/knowledge/Heart/
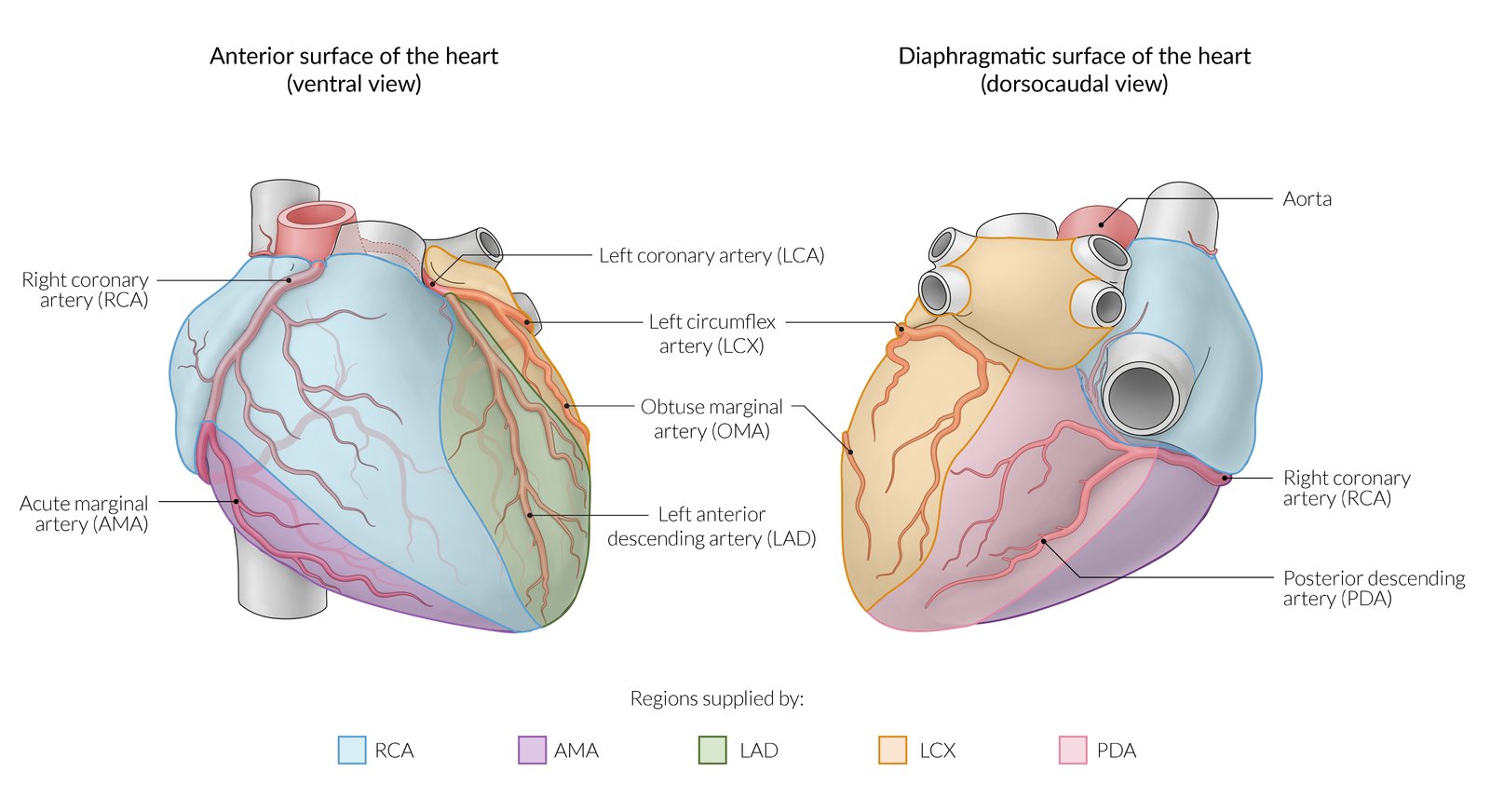
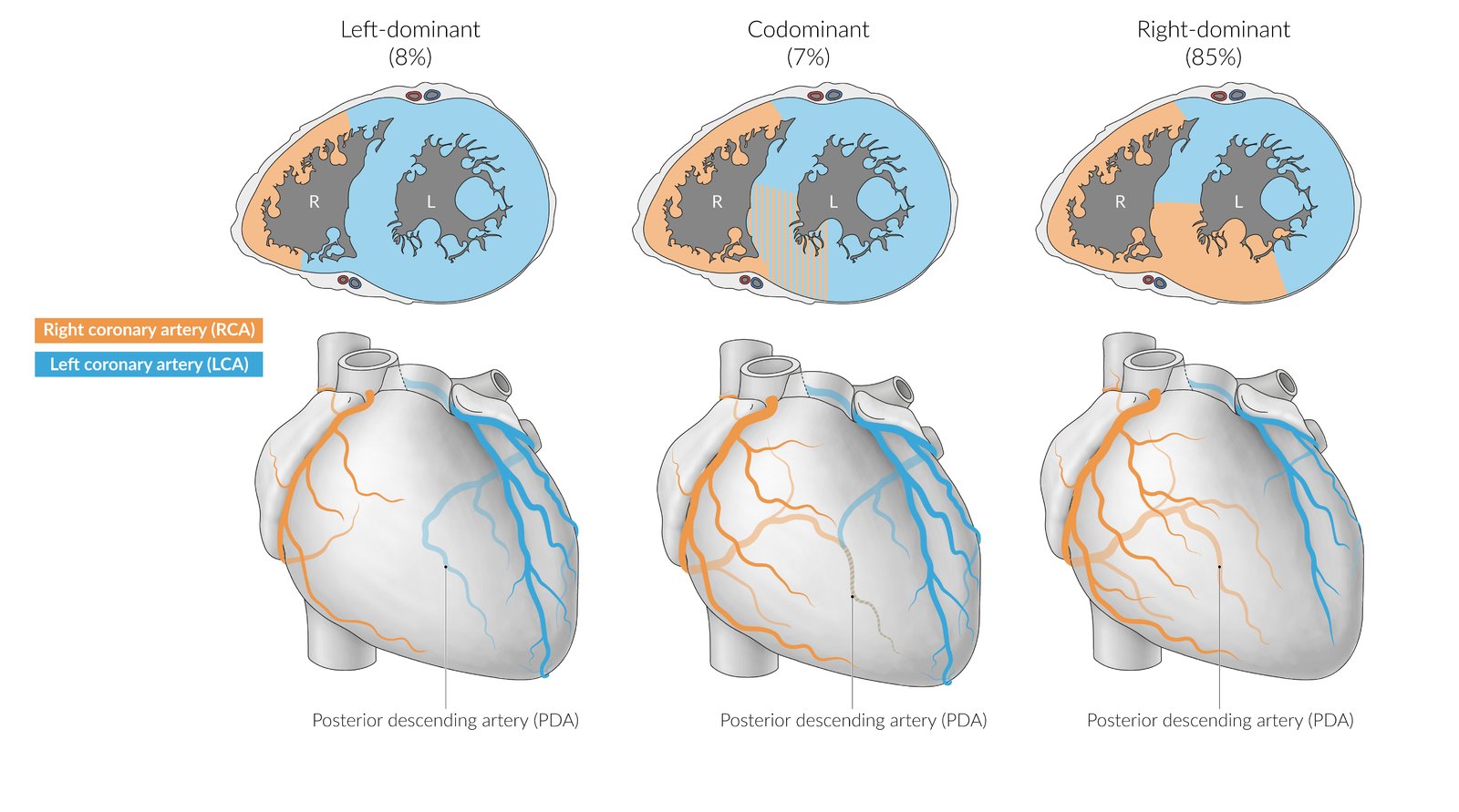
Variations in Coronary Arteries
Generally (in 85% of people), the right coronary artery supplies the right and posterior sides of the heart and the left coronary artery supplies the left and anterior sides of the heart. This is termed right-dominance. In some individuals (8%), the posterior interventricular artery branches from the circumflex artery, instead of from the right coronary artery. This is termed left dominance (because the left coronary artery gives rise to both the anterior and posterior interventricular arteries). In third subset of people (7%), the posterior interventricular artery arises from both the right coronary artery and the circumflex artery. This is termed co-dominance.
Cardiac Veins
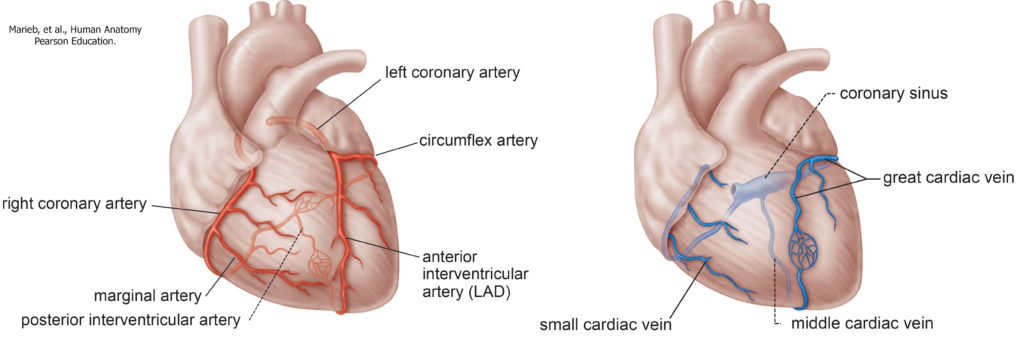
While coronary arteries deliver blood to nourish the heart, deoxygenated blood returns from the heart tissue to the right atrium through a series of cardiac veins. Each coronary artery is accompanied by a specific cardiac vein.
- The great cardiac vein is the largest vein. It accompanies both branches of the left coronary artery, the anterior interventricular artery and the circumflex artery.
- The middle cardiac vein travels with the posterior interventricular artery.
- The small cardiac vein travels with the right marginal artery.
All of these major cardiac veins drain into the coronary sinus, which delivers the deoxygenated blood to the right atrium.
- A small amount of the venous blood from the coronary circulation empties directly into the right atrium, via microscopic openings in the chamber wall. We will not see these in the lab.
- These vessels are the anterior cardiac veins and smallest cardiac veins.
Knowledge Checks
Clinical Applications: Myocardial Infarction, Treatments for Coronary Artery Obstruction
Myocardial Infarction
If a coronary artery is obstructed (via atherosclerosis or a clot) and collateral circulation is inadequate, a heart attack or myocardial infarct can occur. With the loss of blood supply, the muscle cells of the heart wall can die from the lack of oxygen (ischemia), impairing the function of the affected section of the heart wall.
If damage is in the left ventricle, damage to the wall can lead to incomplete emptying of the ventricle and dilation of the ventricular lumen. The surviving part of the wall may show signs of compensatory hypertrophy. Incomplete emptying of the left ventricle can raise the left ventricular diastolic pressure, which would elevate the left atrial and pulmonary venous pressures and result in pulmonary congestion, as blood essentially “backs up” in the left side of the heart.
If damage is in the right ventricle, similar changes can happen there: incomplete emptying and dilation of the chamber. The increased right ventricular diastolic pressure can lead to systemic congestion and increased venous pressure. This can result in edema in the extremities.
Treatments for Coronary Artery Obstruction
Treatments for coronary artery disease depend on the degree of obstruction and health of the patient. Options include treatment with medications, minimally invasive angioplasty, and highly invasive coronary artery bypass surgery (CABG).
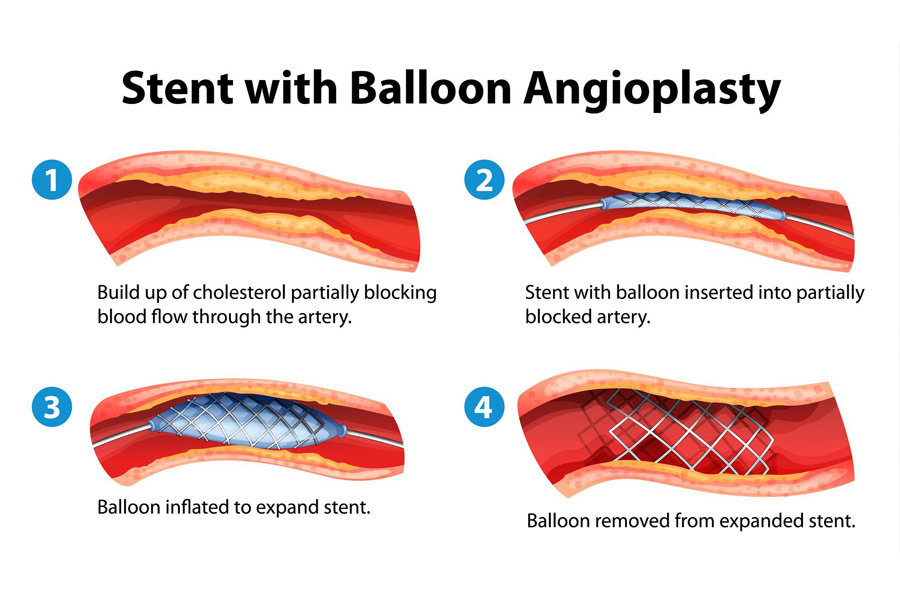
Angioplasty
This procedure involves threading a catheter into the peripheral vasculature (often in the groin or forearm) to reach the site of obstruction in the coronary circulation. Once the blockage is reached, a balloon is inflated to compress the plaque and to increase blood flow. A stent may be inserted in order to help hold the vessel open.
Coronary Artery Bypass Grafting (CABG)
Coronary artery bypass grafting is a surgical procedure in which replacement vessels are attached to the aorta proximally and to a location distal to the blockage, effectively creating a detour or bypass around the site of obstruction. The replacement (donor) vessels are taken from the patient, often from the thorax, forearm, or thigh. This procedure involves open surgery to gain access to the heart. You may see evidence of this type of surgery in the donors in the lab. If multiple grafts are placed, the procedure is called a double, triple, quadruple bypass, etc. Replacement vessels are sutured to the aorta and distal to the site of obstruction to restore sufficient blood flow.
Knowledge Checks