Main Body
Urinary System
Sarah Traynor, PhD
Urinary System: Posterior Abdominal Wall and Pelvis
Key Concept: The urinary system spans the posterior abdominal wall and pelvis. The kidneys and bladder contain extremely important histological structures allowing filtration of the blood and elimination of the liquid waste
- Overview of the Urinary System
- Surface Anatomy and Relationships of the Kidneys
- General Structure of the Kidney
- Nephron Structure and Histology
- The Collecting System
- Blood Supply and Drainage of the Kidney
- Blood Supply to the Urinary Bladder
- Nerves of the Posterior Abdominal Wall and Pelvis
- Innervation of the Urinary Bladder
I. Overview of the Urinary System
The urinary system is one of four organ systems that eliminate wastes. The digestive system eliminates solid waste, including indigestible food; the respiratory system eliminates carbon dioxide and water; the skin eliminates wastes in the sweat; the urinary system eliminates waste products that it filters from the blood. The urinary system is very selective in which substances it excretes so that it also controls the fluid balance in the body.
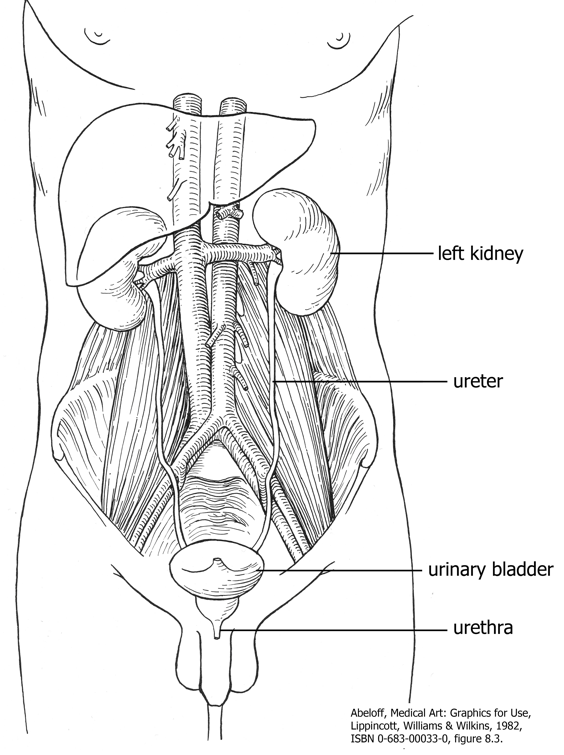
There are four organs in the urinary tract: the kidneys, ureters, urinary bladder, and the urethra. All of these organs form retroperitoneally in the embryo (posterior to the abdominal organs and the serous sac that encloses most of the abdominal organs). Although the kidneys first develop in the pelvis, they typically ascend to assume a position next to the suprarenal (adrenal) glands. In this final position, the superior poles of the kidneys are protected by the rib cage.
II. Surface Anatomy and Relationships of the Kidneys
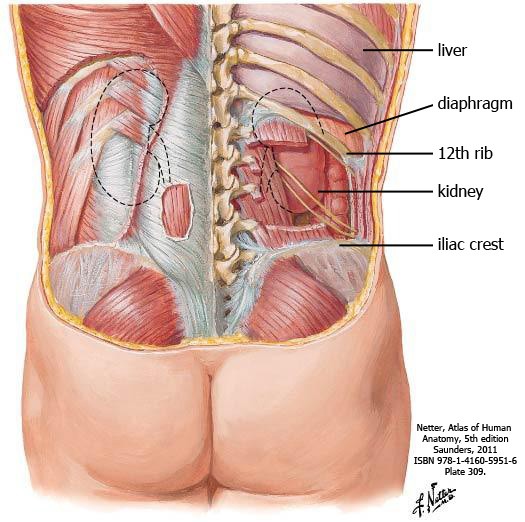
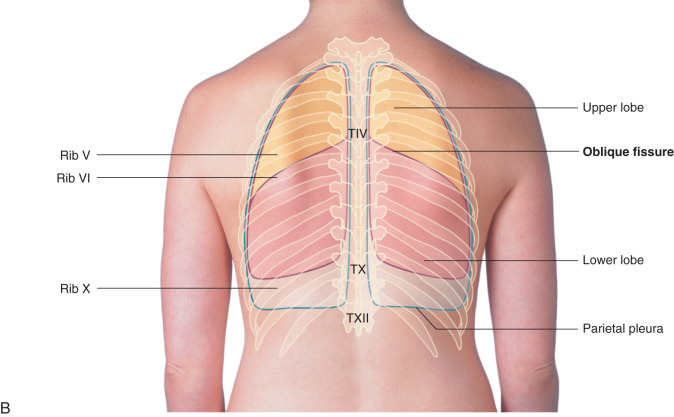
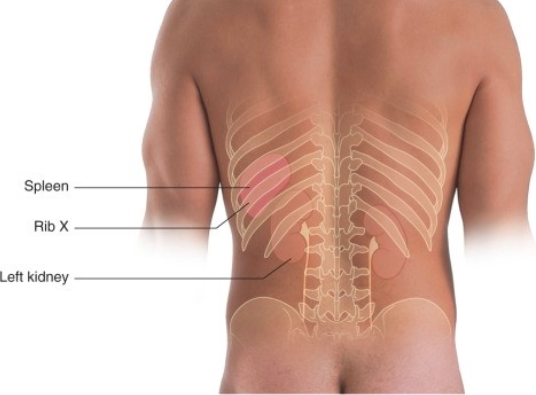
The kidneys are located approximately between vertebral body levels T12-L3. The right kidney is slightly lower than the left because of the liver. The superior pole of each kidney is protected by the thoracic cage, which also means they are overlapped posteriorly by the thoracoabdominal diaphragm and pleural cavity (remember the pleural reflection posteriorly is at the twelfth rib). To avoid entering the pleural cavity, as a rule, needle biopsies are taken from the lower ½ of the kidney.
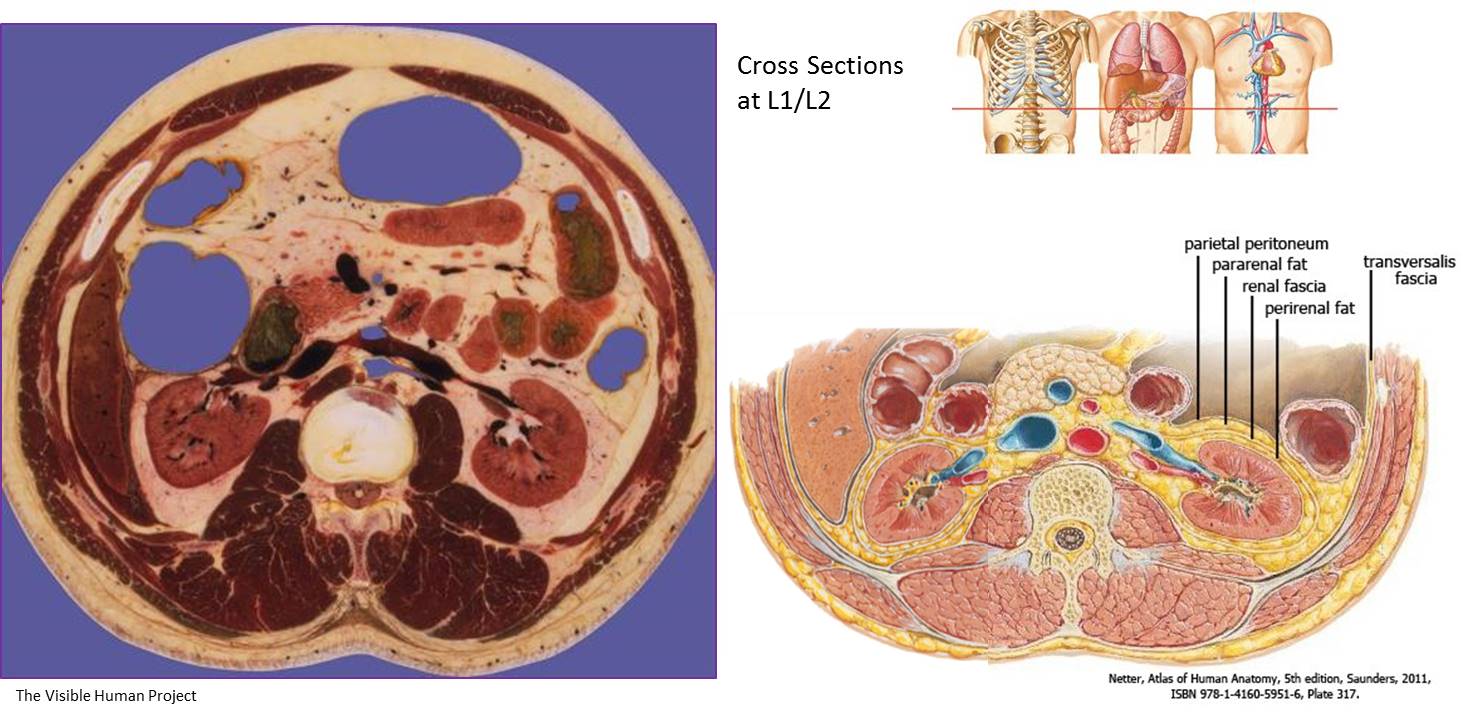
The kidneys are retroperitoneal organs—they develop and stay behind the parietal peritoneum. The parietal peritoneum is similar to the pericardial or pleural sacs of the heart and lungs, respectively, in that the GI organs are protected and supported by the visceral and parietal layers of the peritoneum. The GI organs include the stomach, spleen, liver, pancreas, small intestine and colon. These are known as peritoneal organs because they are associated with the peritoneum. We will discuss exceptions to this in Food, Fasting, and Fitness (FFF) course in the Spring semester. Retroperitoneal organs, such as the kidney, adrenal gland, and aorta, differ from peritoneal organs because they develop posterior to the GI tract and peritoneum and are not associated with the peritoneum.
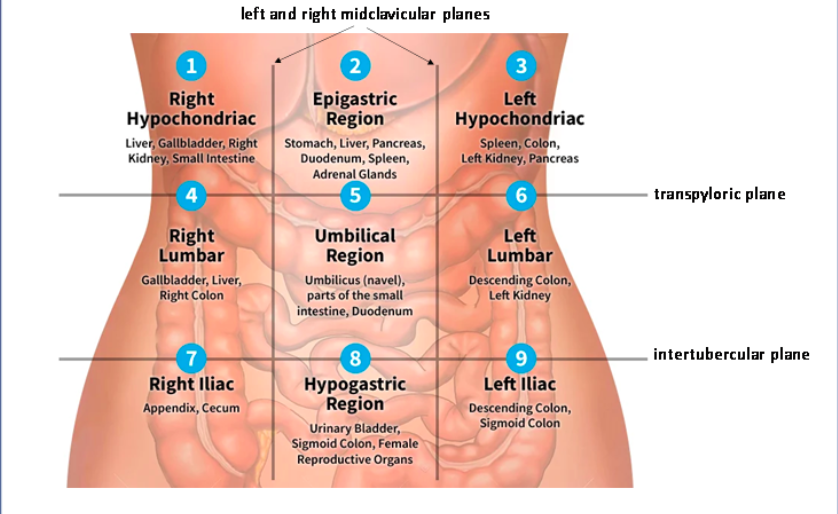
The anterior surface of the right kidney is in contact with the liver, duodenum, and right colic flexure. The anterior surface of the left kidney is in contact with the stomach, spleen, pancreas, and left colic flexure. The left and right kidneys are located within the left and right hypochondriac and lumbar regions of the abdomen, respectively.
Each kidney is located in an area known as the paravertebral gutters immediately embedded in perirenal fat. The perirenal fat and kidneys are enclosed in renal fascia, which is continuous across the midline. Renal fascia is sometimes referred to as ‘Gerota’s fascia’. External to the renal fascia is another layer of fat termed the pararenal fat. Together with the fat, the renal fascia is important in anchoring the kidneys in place.
Knowledge Check
III. General Structure of the Kidney
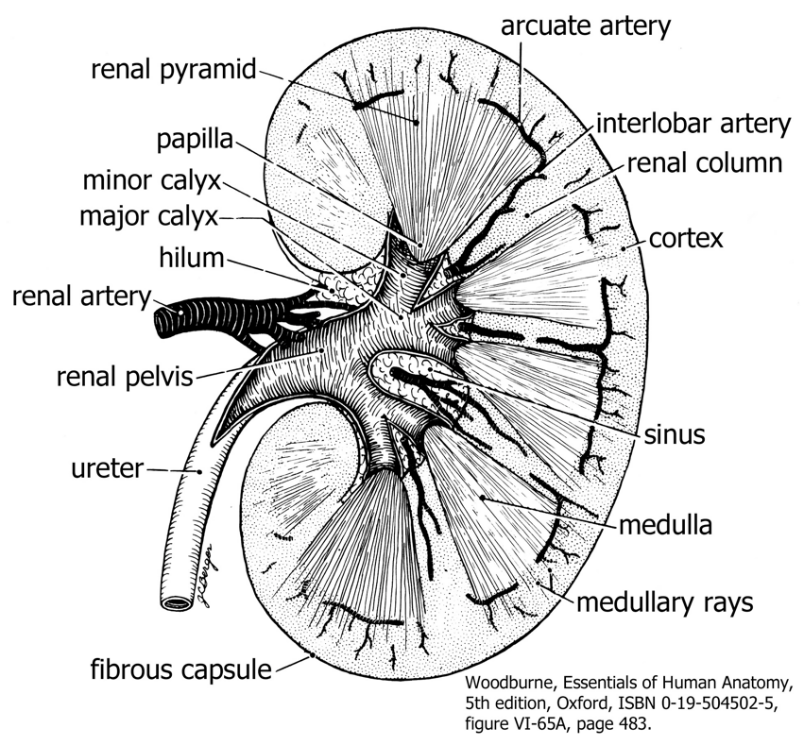
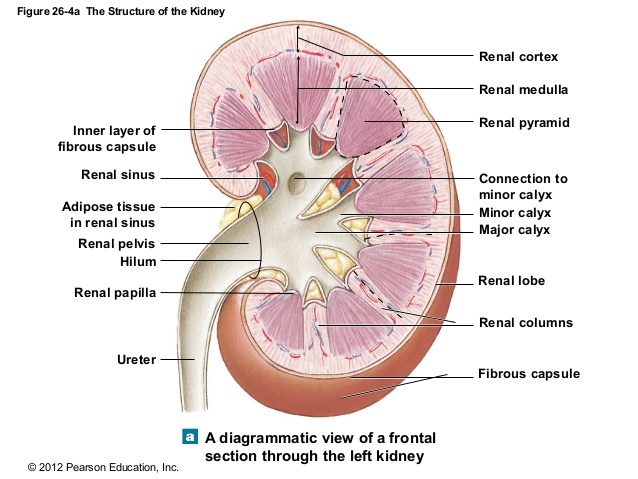
The kidney is a bean-shaped organ that is usually about the size of a bar of soap. It is convex laterally and concave medially at the hilum where the ureter and all vessels and nerves enter or leave the organ. Externally, a capsule of dense irregular connective tissue surrounds the kidney. Internally, the functional tissue of the kidney is subdivided into three major regions: the outer cortex, the middle medulla, and the inner renal sinus.
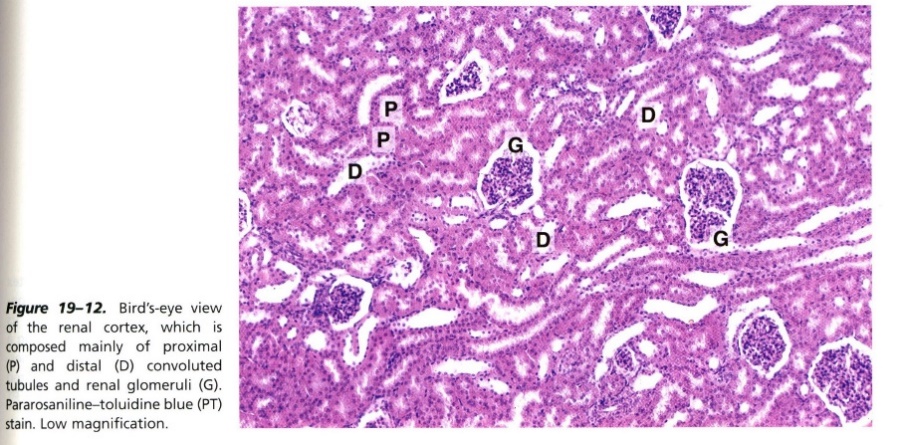
- Cortex: The cortex is the outer region of the kidney just beneath the capsule. This region appears granular because it contains all the renal corpuscles, the structures that filter the blood. Because the filtration is relatively crude, there are additional tubules in the cortex and medulla that can reabsorb substances that must be recovered from the filtrate or can secrete additional substances into the filtrate that could not pass through the urinary filter.
- Medulla: This is the deeper region of the kidney that consists of 8-18 renal pyramids. The bases of the pyramids are next to the cortex and the apices of the pyramids, called papillae, are closer to the renal sinus. The pyramids are separated from each other by the renal columns, extensions of the cortex that penetrate the medulla. Likewise, there are extensions of the medulla called medullary rays that radiate into the cortex. The renal columns and medullary rays form interdigitations between the cortex and medulla. The renal pyramids appear striated because they contain a series of tubules that are all aligned with each other. These tubules continue to modify the filtrate by resorbing substances from it and they help to concentrate the filtrate, so we do not lose too much body fluid.
- Renal Sinus: The renal sinus is an inner cavity within the kidney that is occupied by the collecting system of the kidney, blood vessels, nerves and fat. There are 8-18 initial branches of the collecting system called minor calyces, one for each renal pyramid. When the urine is delivered to the minor calyx from the collecting ducts at the renal papilla, it is in its final form and will not be modified further in any way. The minor calyces drain into the major calyces, which empty into the renal pelvis. The renal pelvis is the upper dilated end of the ureter found at the hilum of the kidney. The urine continues immediately through the ureter to the urinary bladder where it is stored.
Knowledge Check
IV. Nephron Structure and Histology
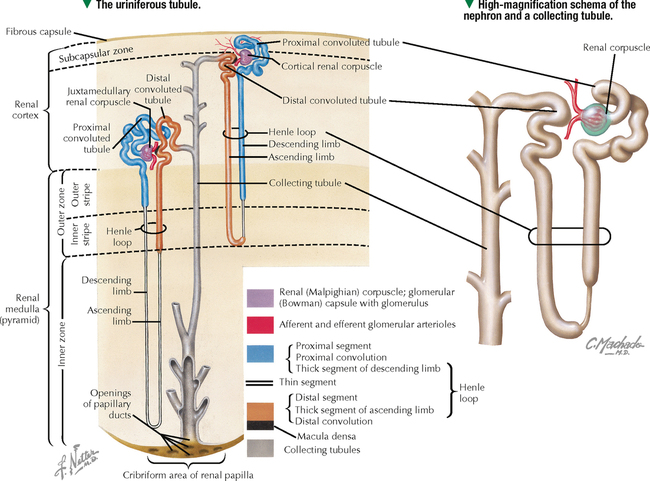
The functional organization within the kidney can be described in multiples levels of scale. On the largest scale, each renal pyramid and its associated cortical tissue form a lobe; on an intermediate scale, each medullary ray and its associated cortical tissue form a lobule; on the smallest scale the kidney contains 1-2 million nephrons that can each produce urine.
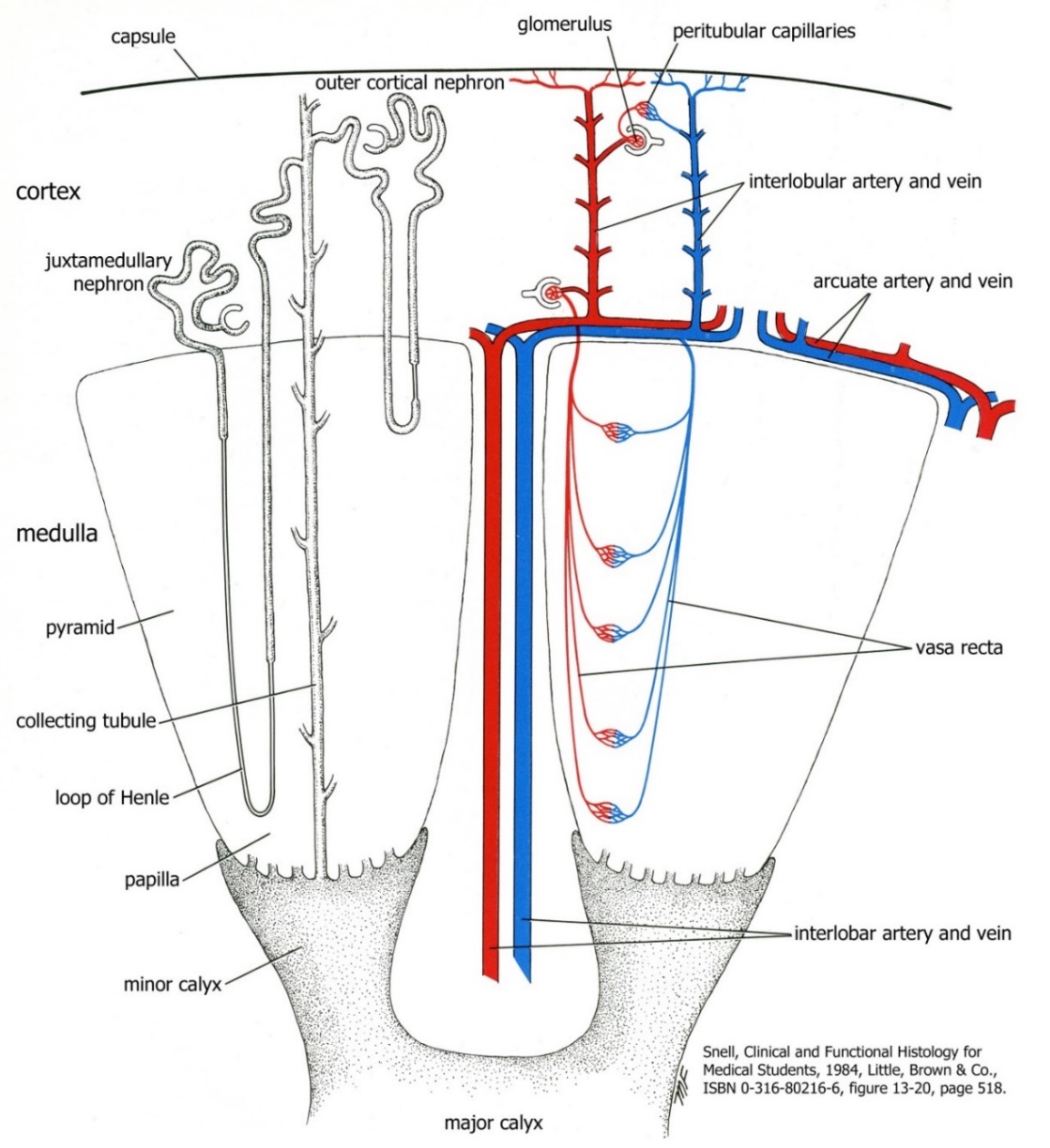
The nephron is the functional unit of the kidney where filtration of metabolic waste occurs. The nephron spans the cortex and the medulla and consists of a 1) renal corpuscle 2) proximal convoluted tubule 3) loop of Henle 4) distal convoluted tubule and 5) collecting tubule.
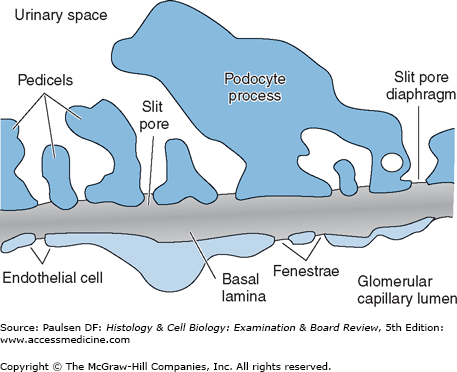
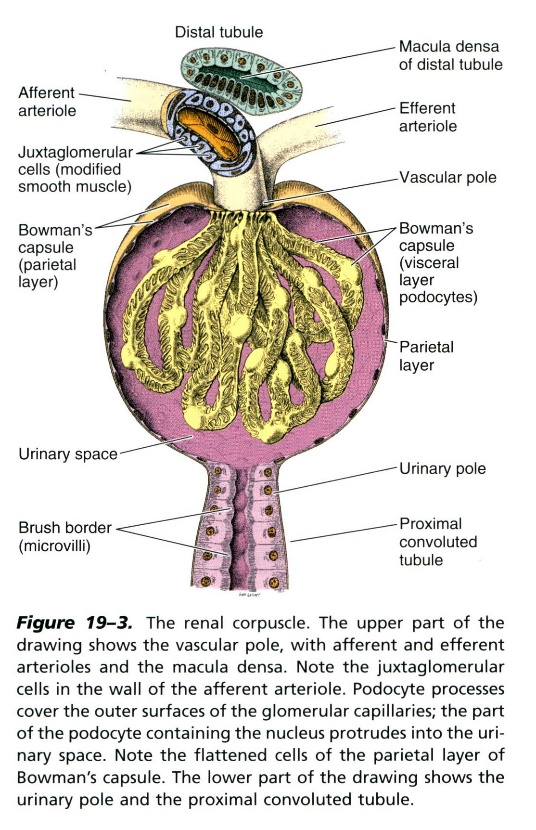
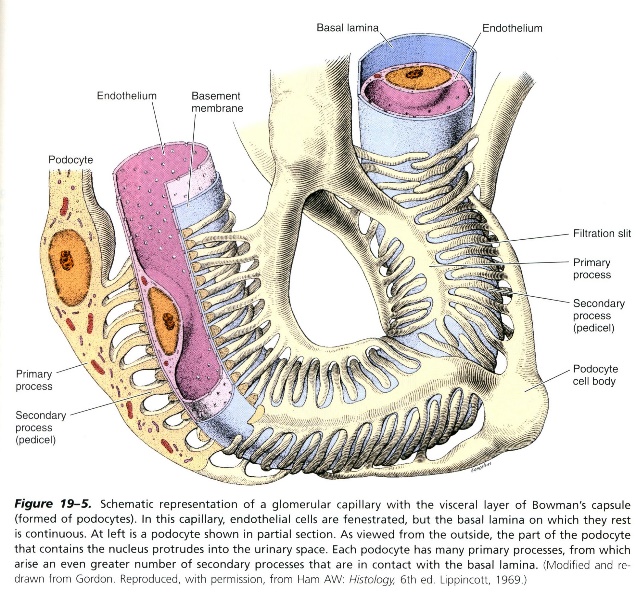
Beginning in the cortex, the renal corpuscle consists of the glomerulus and the glomerular capsule (Bowman’s capsule). The renal corpuscle has a vascular pole and a urinary pole. The vascular pole contains the afferent and efferent arterioles entering and exiting the glomerulus, respectively. The glomerulus is a capillary bed of fenestrated endothelium, where metabolic waste is crudely filtered out of the blood. The glomerular capsule surrounding the glomerulus consists of two layers, a visceral layer and a parietal layer. The visceral layer is composed of specialized epithelial cells called podocytes. Podocytes have processes called pedicels that envelop the capillaries. Because both the endothelium and the podocytes have basal lamina, it is the combination of both basal laminae that create the basement membrane that lies between the endothelium and pedicels. The endothelium, basement membrane, and filtration slits between pedicels (visceral layer of glomerular capsule) are the three layers that comprise the urinary filter.
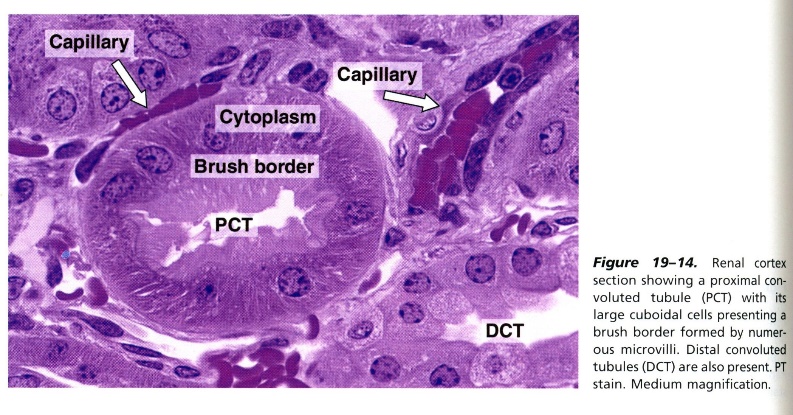
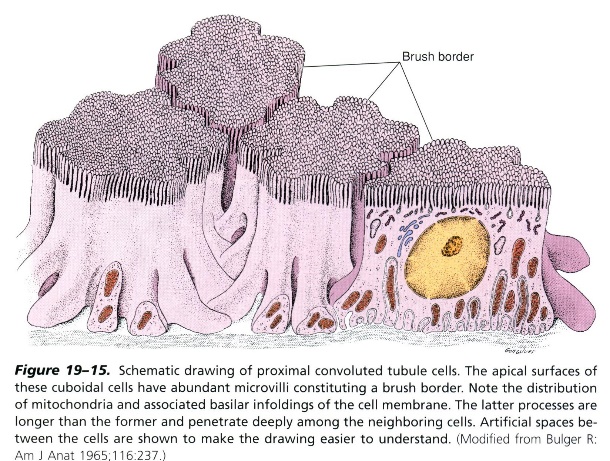
After the PCT, the filtrate passes through the descending and ascending thick and thin limbs of the loop of Henle. Henle’s loop extends into the medulla and is primarily for water retention. The descending thick limb consists of simple cuboidal cells with brush border (like the PCT, except in the medulla rather than the cortex). The thin limb consists of simple squamous cells. The ascending thick limb consists of simple cuboidal cells without a brush border. The lumen is more apparent in the ascending thick limb compared to the descending thick limb due to the lack of a brush border.

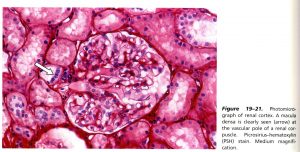
At the transition from the ascending thick limb to the distal convoluted tubule, we find the macula densa. The macula densa is very apparent histologically because the cell nuclei are densely concentrated and adjacent to the afferent arteriole at the vascular pole of the renal corpuscle within the cortex. The macula densa cells are particularly sensitive to filtrate flow rates and ion content and part of a functional region known as the juxtaglomerular apparatus, which will aid in the regulation of blood pressure. After passing the specialized cells of the macula densa, the filtrate is now in the distal convoluted tubule (DCT). The DCT is composed of simple cuboidal cells, but unlike the PCT, these cells do not contain the brush border.
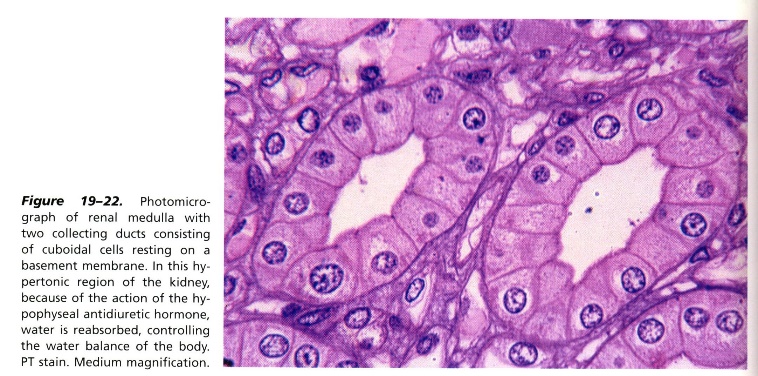
Once the filtrate has passed through the DCT, it will drain into the collecting ducts, which will span the length of the renal pyramid (medulla) down to the renal papilla. The collecting ducts are also composed of simple cuboidal cells and aid in water retention. Once the filtrate is at the apex of the renal pyramid (renal papilla) in the collecting duct, it is in its final form as concentrated urine and will drain into the minor calyx, which is the beginning of the collecting system of the kidney.
Knowledge Check
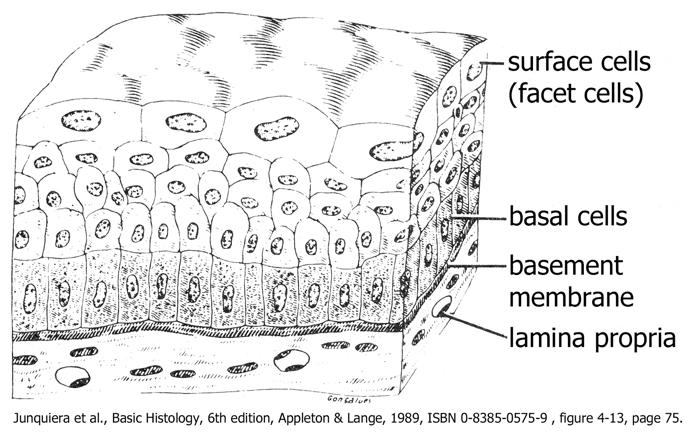
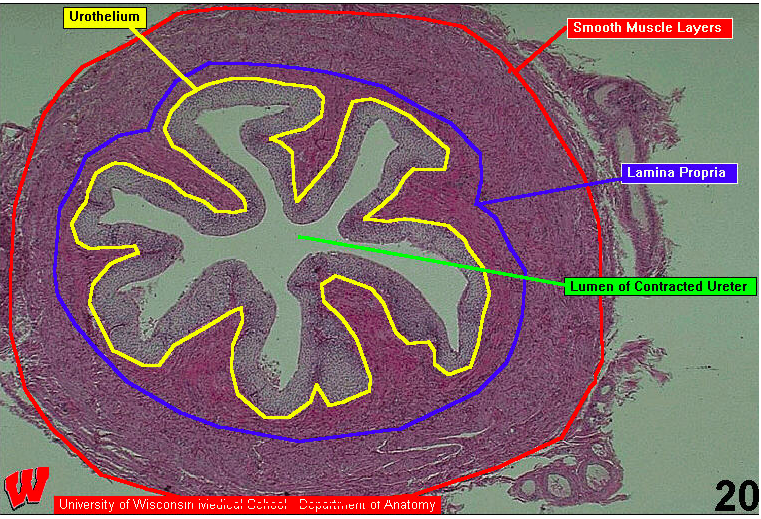
After the urine enters the minor calyx, it continues immediately to the major calyx, renal pelvis, and then to the ureter. As it continues through the urinary system, the urine will not be modified in any way. Because the amount of urine being excreted at any time may vary widely depending on fluid intake and hormonal effects, all organs downstream of the kidney must be able to adapt to the possibility of holding a variable amount of fluid.
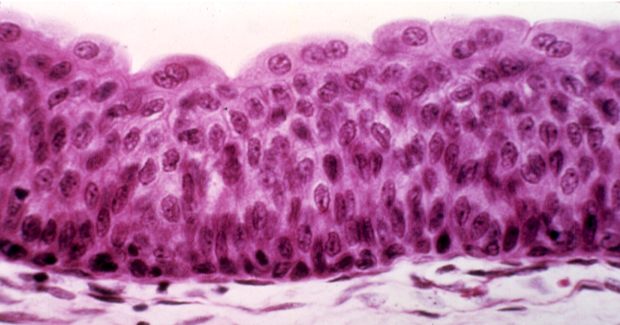
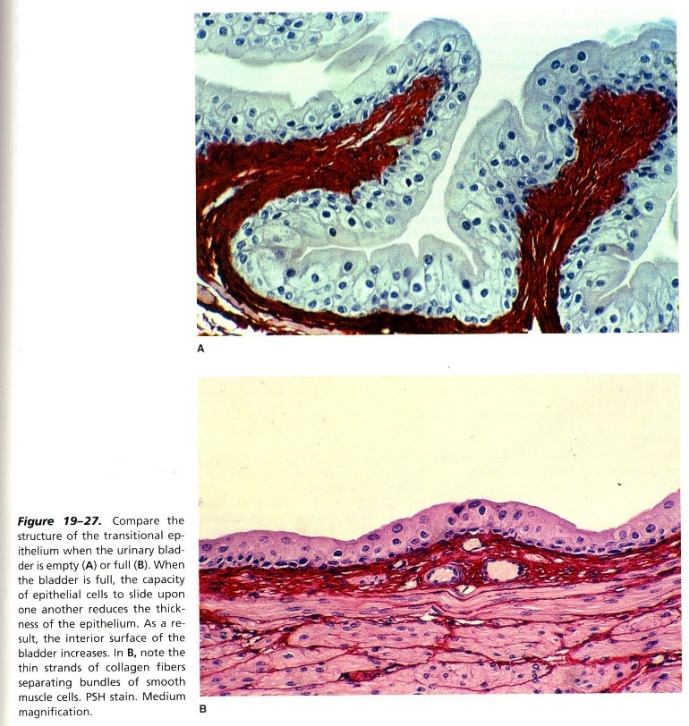
One feature shared by all structures and organs in the collecting system from the minor calyx through the proximal portion of the urethra is their epithelium. They are all lined by urothelium or transitional epithelium. When the organ is relatively full of urine, the epithelium will be stretched and flattened and have fewer layers; when the organ is relatively empty, and collapsed, its epithelium will be thicker, with the characteristic, domed surface cells at the apex of the epithelium. As this transition in the epithelium occurs, the cells and their relationships change dramatically. Cell junctions can break down and be reassembled, and the cell may add or remove plasmalemma (extra cell membrane) from its surface as it changes shape. This is possible because the epithelial cells contain a reservoir of plasmalemma vesicles in the cytoplasm that can quickly be inserted or removed as needed.
The ureter is lined with urothelium and surrounded by two layers of smooth muscle. The inner smooth muscle layer is mostly longitudinal and the outer layer is mostly circumferential, but they blend with each other so that the layers are not as discrete as they are in the gut. The muscle contracts through peristalsis to force the urine toward the urinary bladder for storage.
There is not a sphincter at the entry to the bladder to prevent backflow. Instead, the ureter passes obliquely through the wall of the bladder so that as the bladder fills with urine, it compresses the opening of the ureter (ureteric orifice) to prevent backflow. This is essential for preventing an infection in the urinary bladder from ascending to the kidney.
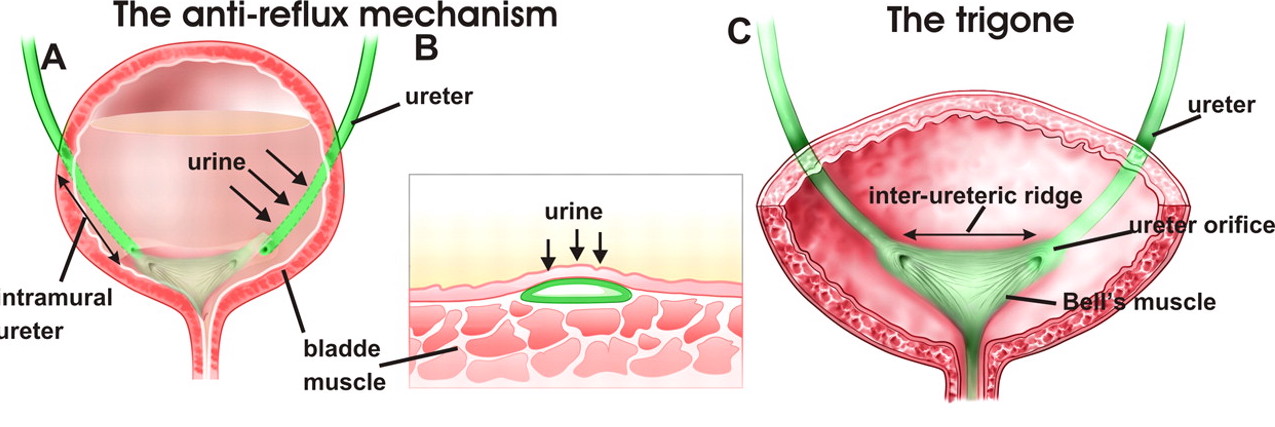
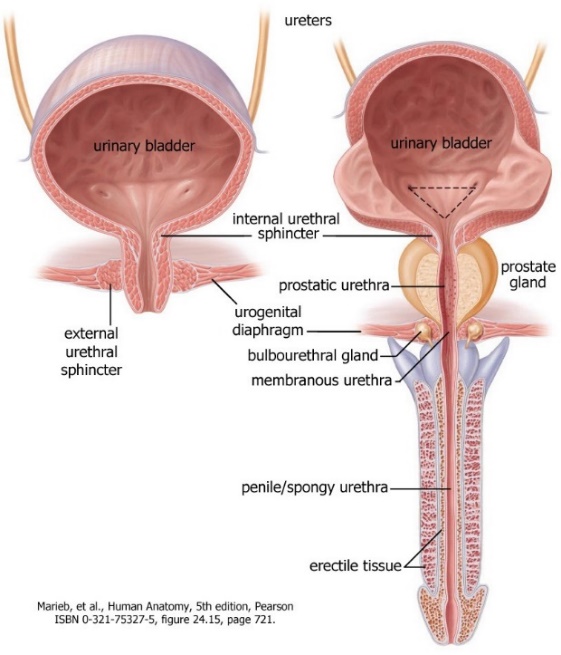
The urinary bladder stores the urine until urination is convenient. Structurally, the bladder looks similar to the ureter except that it is larger and it has three thick layers of smooth muscle in its muscularis layer. These three layers of muscle are known collectively as the detrusor muscle. This muscle contracts to empty the bladder during urination (micturition). The innervation of the detrusor muscle is explained below in section IX. The triangle at the base of the bladder created by the ureteric and urethral orifices is known as the trigone. It does not stretch or contract during urination and is of a different embryologic origin than the rest of the bladder.
The urethra is the organ that delivers urine from the urinary bladder to the outside. Because it connects an internal surface with an external surface, its epithelium changes from the typical transitional epithelium on its proximal end to nonkeratinized stratified squamous epithelium on its distal end. There are two sphincters that control when urine passes through the urethra. The internal urethral sphincter is a smooth muscle sphincter at the junction between the bladder and the urethra. The external urethral sphincter is a skeletal muscle sphincter that forms where the urethra penetrates a sheet of skeletal muscle called the urogenital diaphragm. Both sphincters must relax during urination/micturition. The innervation of each urinary sphincter is discussed below in section IX. The male urethra will be discussed further in the Human Family Tree (HFT) course.
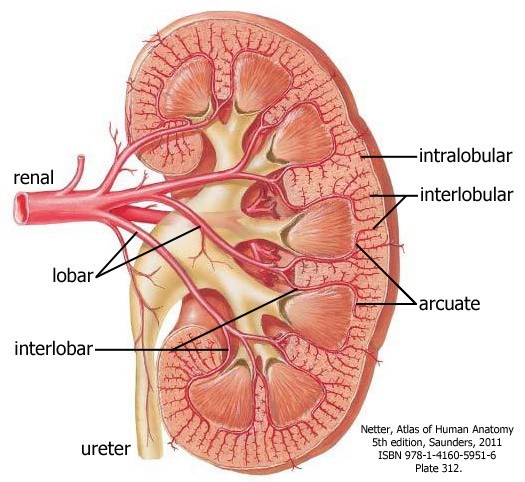
Because the kidneys are specialized to clean the blood, they receive a disproportionately high volume of blood for their size; ~25% of the cardiac output goes to the kidneys. Every minute the kidneys filter ~1 liter of blood. Blood enters the kidneys at the hilum through the renal arteries, direct branches of the abdominal aorta that arise at about the level of the superior mesenteric artery. In about 30% of individuals, there are additional polar arteries that enter either the superior of inferior pole of the kidney. These are formed as the kidney ascends from the pelvis to its adult position and sometimes do not degenerate as they normally would. Branching off of the renal artery is the inferior adrenal (suprarenal) artery as the inferior-most of three arteries that supply the adrenal (suprarenal) gland. This is why we consider the adrenal gland to be anatomically, but not functionally, related to the kidney.
As the renal arteries approach the hilum, they branch into lobar (segmental) arteries, and then into interlobar arteries, which pass between the renal pyramids. At the junction between the cortex and medulla, they arch to pass along the base of the renal pyramid as arcuate arteries. These arteries branch at 90˚ again, forming the interlobular arteries, which enter the cortex. Finally, a small branch called an intralobular artery, which is the afferent arteriole, flows into a capillary bed called a glomerulus. This is where filtration occurs. There are no arterial anastomoses between the lobar arteries; a lobe of the kidney will become necrotic if a lobar (segmental) artery is occluded.
Depending on the position of the glomerulus within the cortex, there are two options for where the blood flows from here.
- If the glomerulus is near the capsule, the efferent arteriole flows into a second capillary bed called the peritubular capillaries, which wrap around the convoluted tubules. Finally, the blood leaves the kidney by following a path of veins that parallel the arteries, ultimately cava, and back to the heart.
- If the glomerulus is near the corticomedullary junction, the efferent arteriole contributes to the capillary plexus in the cortex and long straight branches called vasa recta (straight vessels), which descend into the renal pyramid then ascend back toward the cortex to drain into the arcuate or interlobular veins. The vasa recta are essential to form a concentration gradient in the pyramid, allowing concentration of the filtrate.
The veins in the kidney parallel the arteries. Ultimately, the renal veins drain into the inferior vena cava (IVC). Because the vena cava is to the right of the aorta, the left renal vein is longer than the right renal vein. The renal veins are anterior to the renal arteries, so in radiographs you will see the left renal vein cross anterior to the aorta to enter the IVC.
The passage of the left renal vein just inferior to the origin of the superior mesenteric artery (SMA) is clinically significant because the left renal vein can be compressed by the SMA if the angle of the SMA off of the abdominal aorta does not allow enough space for the left renal vein to cross over the aorta to drain into the IVC, leading to stasis of blood flow out of three organs: left kidney, left suprarenal gland, and the left gonad.
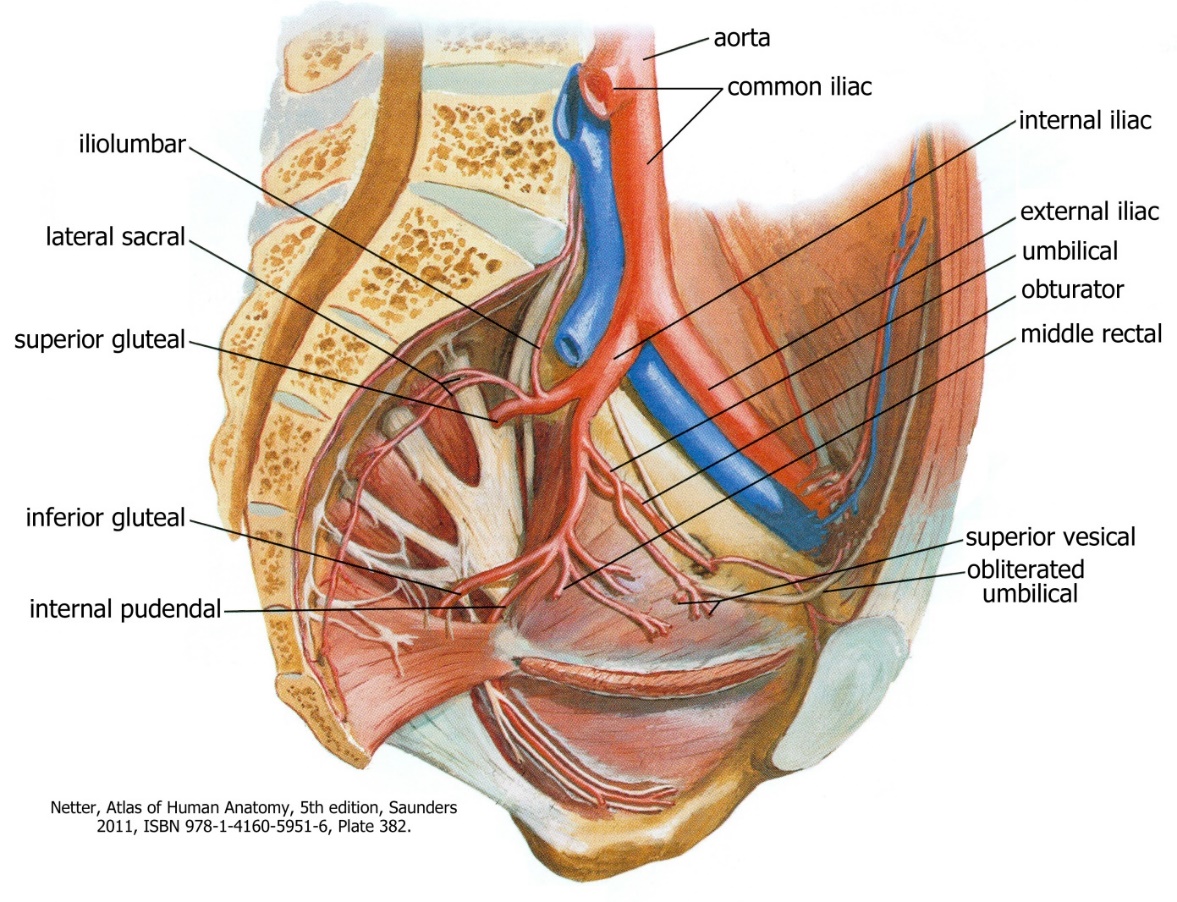
VII. Blood Supply to the Urinary Bladder
The internal iliac artery is the main blood supply to the structures of the pelvis. Other vessels supplying the area include the ovarian/testicular, superior rectal, and the median sacral arteries. The internal iliac is one of the terminal branches of the common iliac artery. It descends into the pelvis medial to the psoas major muscle to the level of the greater sciatic foramen where it branches. There is great variation in its branching pattern. In general the branches are in three groups: to the viscera, pelvic wall, and lower limb/perineum.
The visceral branches include the umbilical, superior vesical, and inferior vesical in males, uterine and vaginal in females, and the middle rectal arteries. We are only concerned with the three bolded vessels below that supply the urinary bladder. Of these, the umbilical and superior vesical arteries are the easiest to identify.
Usually branching off of the umbilical artery, the superior vesical artery supplies the upper margin of the bladder. After the superior vesical artery branches, the umbilical artery becomes obliterated (closed) in adults. This artery was once crucial for fetal circulation as it transferred blood from the fetus to the placenta. In males, the inferior vesical artery supplies the lower portion of the bladder and the prostate gland. In females the inferior vesical is replaced by the uterine artery, which courses medially, passing over the ureter, toward the cervix of the uterus and vagina. We will revisit the internal iliac artery and its other branches when we look at the digestive and reproductive systems in FFF and HFT, respectively.
Knowledge Check
VIII. Nerves of the Posterior Abdominal Wall and Pelvis
Abdomen
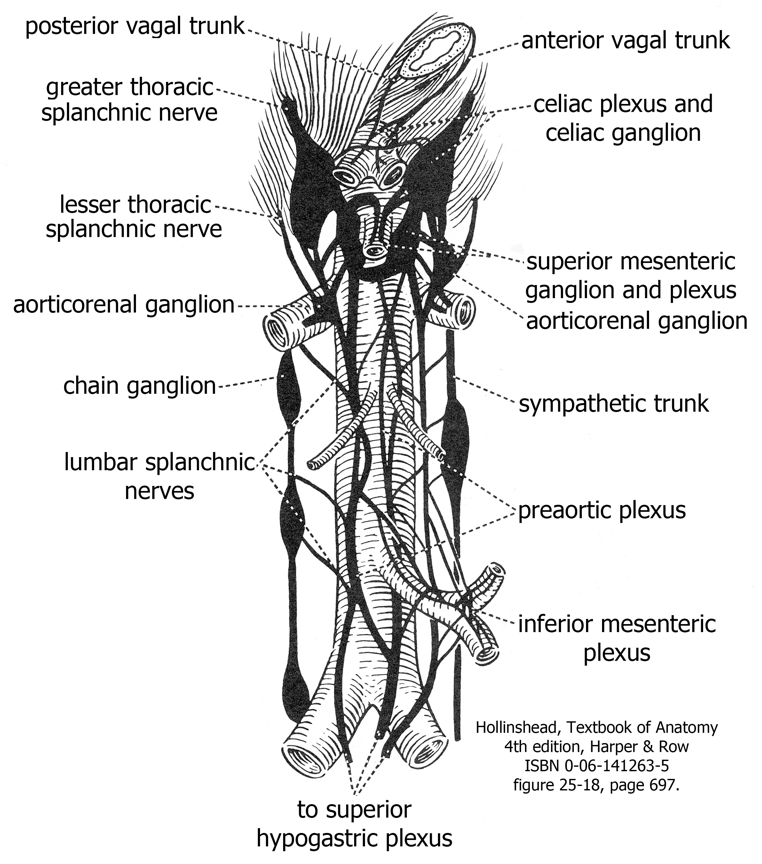
Thoracic and lumbar sympathetic splanchnic nerves innervate the abdominal organs. The preganglionic nerves synapse on postganglionic cell bodies in collateral ganglia (celiac, superior mesenteric, aorticorenal, inferior mesenteric etc.). These ganglia are all interconnected by nerves to form the preaortic plexus. The postganglionic axons follow blood vessels to their target organs. We asked you to follow the greater thoracic splanchnic nerve in the posterior mediastinum. Other splanchnic nerves enter other collateral ganglia. You do not have to know all the details of which splanchnic nerve synapses in which ganglion if you understand the principle—sympathetic splanchnic nerves synapse in collateral ganglia. Know the greater thoracic splanchnic as the most graphic example of this principle. Sympathetic innervation inhibits activity of the digestive tract by reducing blood flow. Postganglionic sympathetic fibers travel to the kidneys to regulate blood flow in the arteries (primarily the afferent and efferent arterioles) and to regulate fluid flow in the nephron (primarily in the proximal tubule).
Some of the preganglionic sympathetic fibers entering the celiac ganglion pass through it without synapsing. Instead, they synapse directly on target cells in the adrenal medulla. This is the one exception to the rule that there are “always” two neurons in a sympathetic pathway. It is perfectly logical because the cells in the adrenal medulla and the postganglionic neurons of the sympathetic nervous system both develop from neural crest cells. When stimulated by the preganglionic neurons, the adrenal cells release neurotransmitters (norepinephrine and epinephrine) directly into the blood to produce a generalized sympathetic response.
The majority of abdominal organs receive parasympathetic innervation from the vagus nerves. The anterior and posterior vagal trunks enter the abdomen along with the esophagus through the diaphragm. These preganglionic fibers join the preaortic plexus. One of the main functions of parasympathetic innervation in the abdomen is the increase of gut motility. The remaining portion of the gut found in the abdomen is innervated by the pelvic splanchnic nerves from spinal cord levels S2, 3, 4 (see next section). The kidneys do not receive parasympathetic innervation.
Pelvis
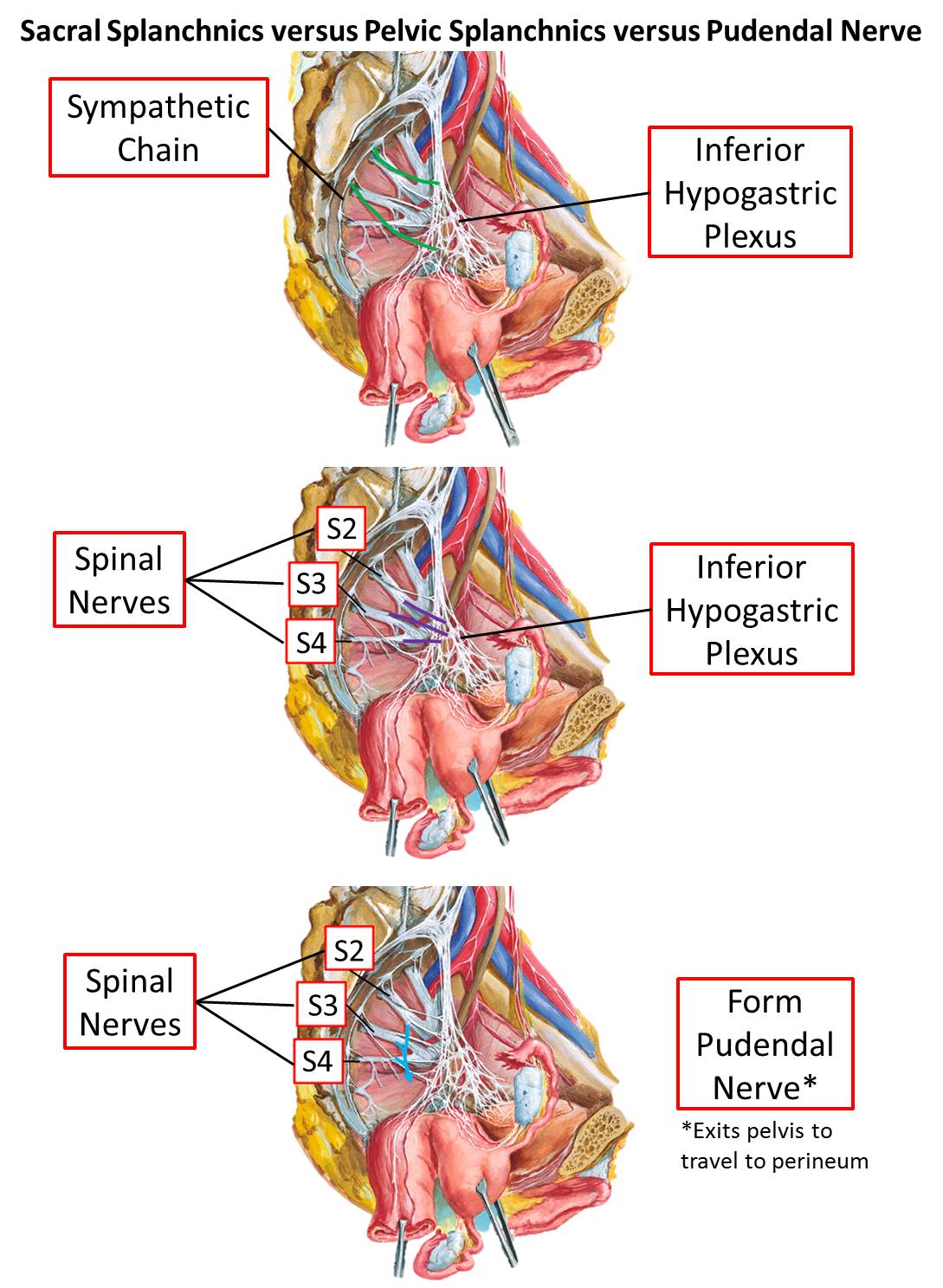
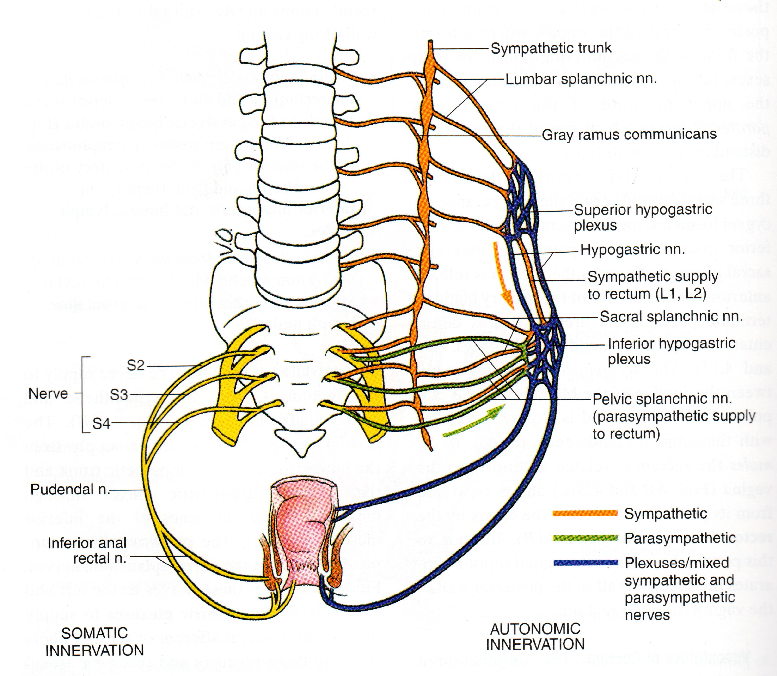
The nerves found in the pelvis can be grouped into somatic and visceral. The large ventral rami of spinal nerves L4-S4 make up the somatic (motor and sensory) portion of this group and can be seen joining together to make a plexus (the sacral plexus). The ventral rami of L4 and L5 join together to form the lumbosacral trunk and pass inferiorly into the pelvis to join the sacral ventral rami. The largest branch of the sacral plexus is the sciatic nerve. We will revisit this plexus in Mind & Motion (M&M) with the lower limb. Another branch of the sacral plexus is the pudendal nerve. This spinal nerve innervates structures in the perineum (i.e. the external urethral sphincter, see Innervation of the Urinary Bladder) and will be covered in more depth in HFT.
The visceral plexuses contain sympathetic, parasympathetic, and viscerosensory fibers. The autonomic plexuses in the lower abdomen and pelvis are continuous and are roughly the shape of an upside-down Y. Superiorly, near the bifurcation of the aorta (at about the L5 vertebral level) is the superior hypogastric plexus. The plexus descends inferiorly and splits into left and right hypogastric nerves (these are more conglomerations of nerve fibers than a single, streamlined nerve). The hypogastric nerves continue to travel inferiorly along either side of the rectum, and split up into inferior hypogastric plexuses. These plexuses will turn anteriorly and run alongside the organs of the pelvis. As they pass the different organs they are renamed for the organ that they are closest to (for example, uterovaginal plexus or prostatic plexus). Removal of pelvic organs (prostatectomy, hysterectomy, abdominoperineal resection) may damage the autonomic plexuses that pass next to them. Damage can result in urinary or fecal incontinence or impotence.
Sympathetic fibers enter the hypogastric plexuses through lumbar and sacral splanchnic nerves extending from the sympathetic trunk. Parasympathetic fibers in the hypogastric plexuses arise from levels S2, 3, 4 of the spinal cord (this is the sacral portion of the “craniosacral” system). Preganglionic parasympathetic fibers travel on the ventral rami of spinal nerves S 2,3,4 until they can exit as pelvic splanchnics to join the inferior hypogastric plexus. Some of these fibers ascend along the hypogastric nerves to reach the superior hypogastric plexus and the inferior mesenteric plexus. The fibers follow the left colic and sigmoidal branches of the inferior mesenteric artery to reach these target organs. Sympathetic and parasympathetic fibers distribute to pelvic viscera as branches from the inferior hypogastric plexus. Most branches accompany vessels to the target organ.
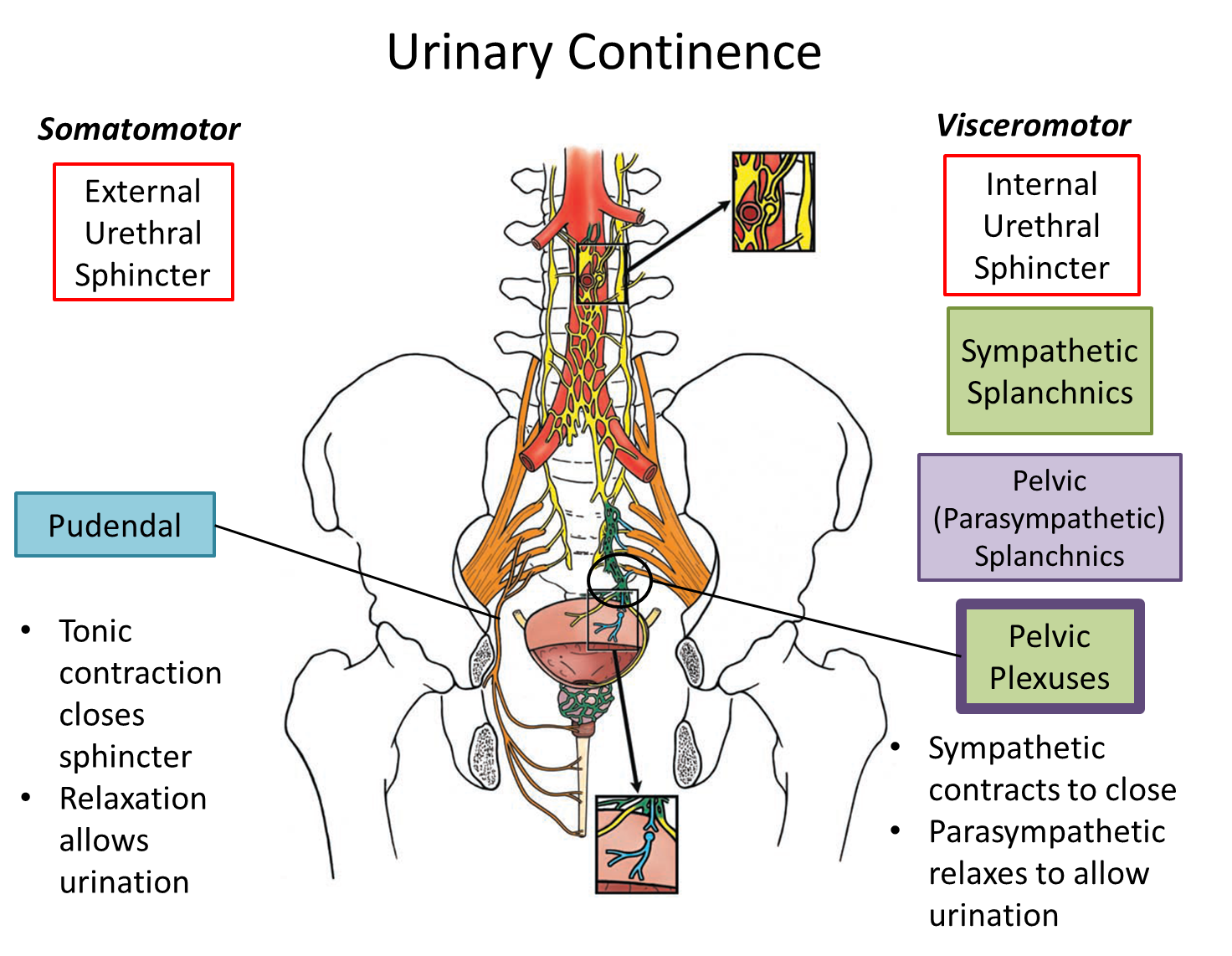
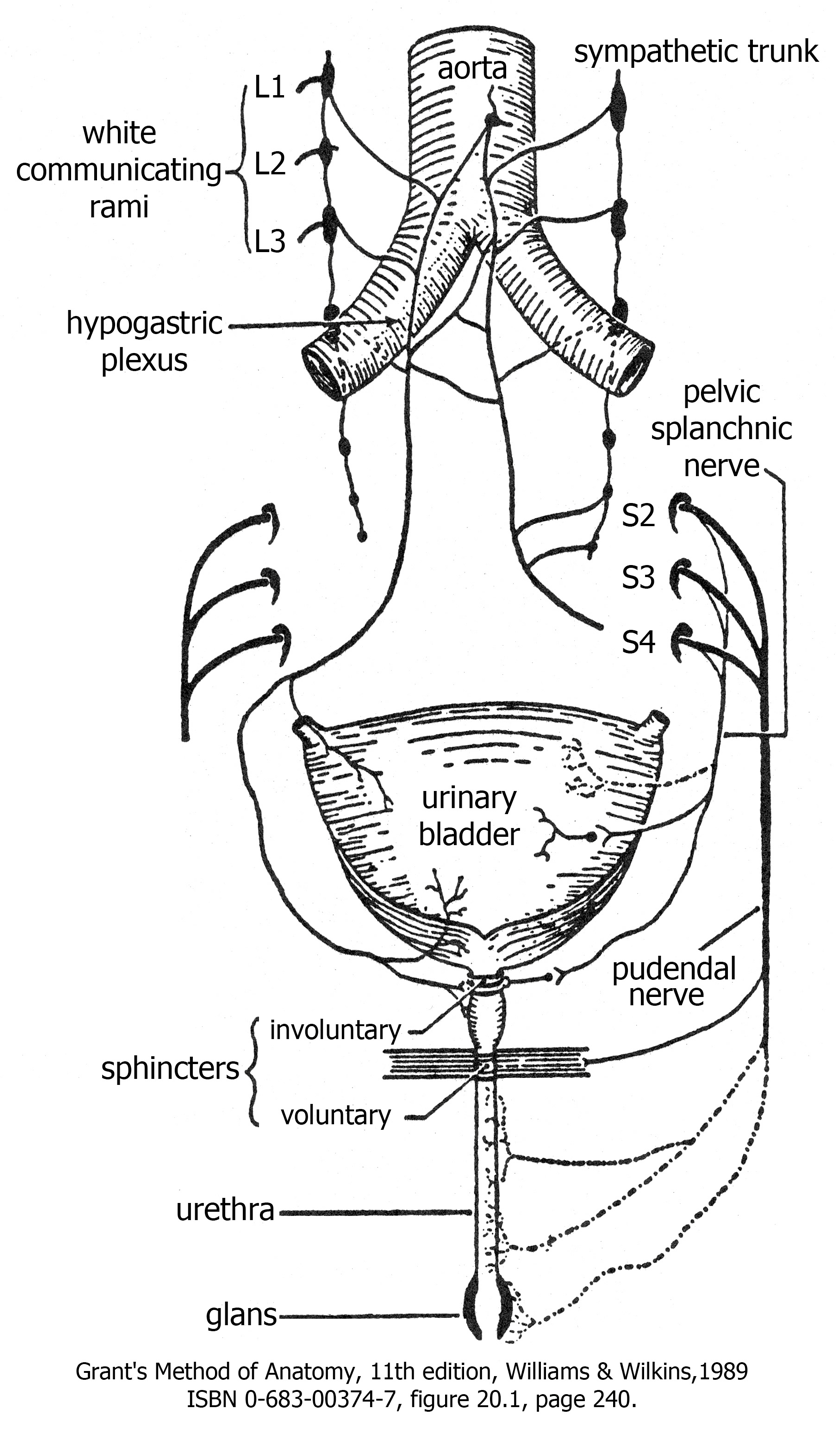
IX. Innervation of the Urinary Bladder
The bladder is innervated by sympathetic, parasympathetic, and sensory fibers. They monitor the stretch of the bladder and coordinate the contraction of the detrusor muscle (smooth muscle) in the wall of the bladder and two sphincters in the urethra. The involuntary internal urethral sphincter is made of smooth muscle and is found at the junction of the bladder and the urethra. The voluntary external urethral sphincter made of skeletal muscle is located in the urogenital diaphragm.
As the bladder fills with urine, the sympathetic neurons relax the detrusor muscle and contract the involuntary sphincter. Somatomotor fibers from the pudendal nerve contract the external urethral sphincter.
As the bladder becomes filled with urine, stretch receptors send sensory information to the central nervous system that stimulates parasympathetic neurons in the sacral spinal cord. Preganglionic parasympathetic axons exit the spinal cord with sacral spinal nerves S2, 3, 4 and form pelvic splanchnic nerves, which pass to and synapse in terminal ganglia in the wall of the bladder. The postganglionic fibers cause contraction of the detrusor muscle and relaxation of the involuntary sphincter.
For urination (micturition) to occur, it is also necessary to relax the external urethral sphincter. This requires inhibition of the somatomotor neurons in the pudendal nerve that innervate the voluntary sphincter.
Knowledge Check