Lab 16: Neurovasculature of the Upper Extremity
Learning Objectives:
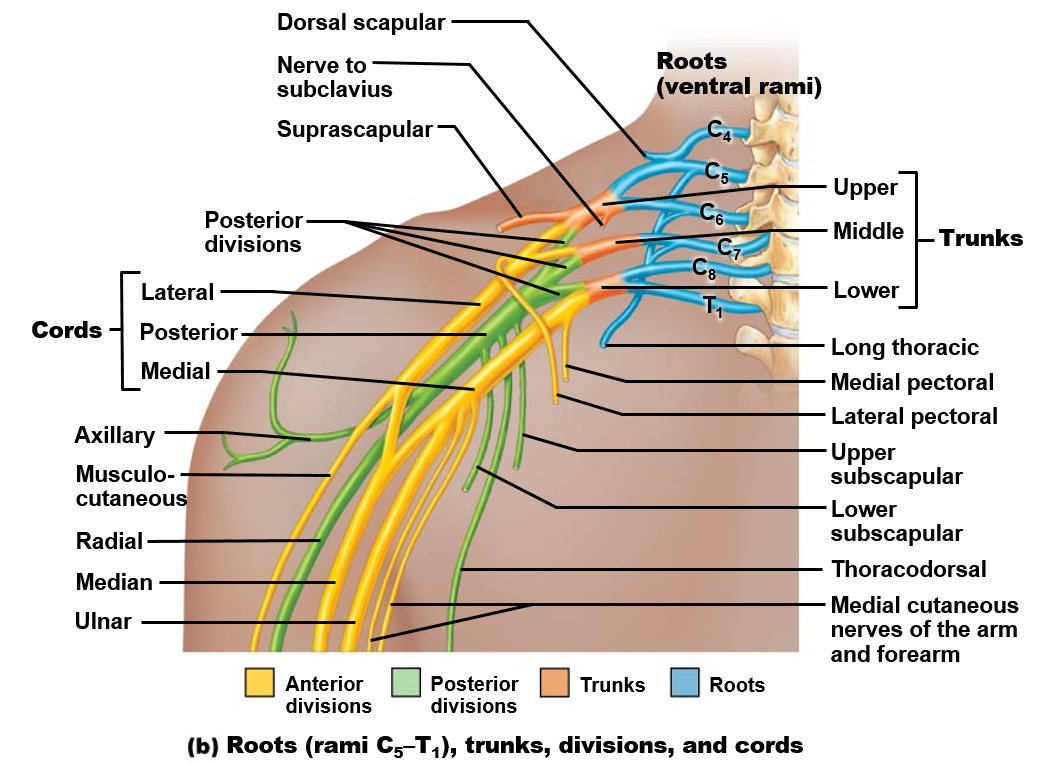
- Describe the brachial plexus and its branches.
- Identify the components of the brachial plexus.
- Describe the vasculature of the upper extremity and identify the regions supplied or drained by each vessel.
- Identify the major arteries and veins of the upper extremity.
Terms to Know
|
Arteries of the Upper Extremity
Veins of the Upper Extremity
|
Brachial Plexus
|
Introduction
In this lab, you will learn about the neurovasculature of the upper extremity. You will learn about the brachial plexus, which eventually branches into all nerves that innervate the upper extremity. You will also learn about the subclavian, axillary, and brachial arteries and their branches that eventually provide the whole upper extremity with blood. You are responsible for the information in this lab guide on the muscles or structures innervated or supplied by these nerves and arteries.
Lab Activity 1: Neurovasculature of the upper extremity – Donor tissue
Observe the nerves and vessels of the upper extremity on the donor tissue. Remember to use landmarks to help you identify the neurovasculature! For example, if you know which muscles are innervated by a specific nerve and follow a nerve to that muscle, you can identify that nerve.
Nerves of the upper extremity:
Explore the brachial plexus. In general, your first step should be looking for the “M” formed by the parts of the medial and lateral cords coming together to form the median nerve. This will help you get your orientation of what is medial and what is lateral. Once you know which is the medial or lateral cord, you can narrow down the branches coming from them. The “M” sits just anterior to the axillary artery. This also makes it easier to identify the posterior cord sitting posterior to the “M” and the axillary artery.
- Here are a few tips for specific nerves in the axillary region:
- Dorsal scapular nerve: This nerve is not present on the donor tissue, but you will be able to identify it in images. This nerve will emerge very early from the brachial plexus, near the neck, and you will be able to see it running posteriorly to the rhomboids and levator scapulae.
- Suprascapular nerve: This nerve will run posteriorly from the brachial plexus towards the scapula. It runs through the suprascapular notch inferior to a ligament forming a bridge across the notch (called the transverse scapular ligament) to reach the supraspinatus and then through the spine of the scapula to reach the infraspinatus. In the deep dissection, this nerve has been dissected through its entire path to the infraspinatus.
- Lateral pectoral nerve: This nerve may not be present in the donor tissue. On an image, you may see it run from the brachial plexus to the pectoralis major. You can also know that it is the lateral pectoral nerve rather than the medial because it will branch off the lateral cord.
- Medial pectoral nerve: This nerve also may not be present in the donor tissue. This nerve is usually the first branch from the medial cord, and it runs through the pectoralis minor, innervating it on its path to the pectoralis major.
- Medial brachial and medial antebrachial cutaneous nerves: These nerves will branch distal to the medial pectoral nerve off of the medial cord. They run to the skin of the medial arm and forearm. One of these is present in the donor tissue, but we cannot tell which it is because it is cut, and we cannot follow it to its destination. These are visible on the plastinated tissue, superficial to the muscles.
- Long thoracic nerve: This nerve is easy to spot in images, as it runs tight to the thoracic wall, innervating the serratus anterior muscle. This is also visible running with the serratus anterior on the superficial dissection.
- Thoracodorsal nerve: Observe this nerve branching off the posterior cord and running to the latissimus dorsi muscle.
- Upper subscapular and lower subscapular nerves: These nerves branch from the posterior cord, with the upper branching proximal to the thoracodorsal nerve and the lower branching distal to the thoracodorsal nerve in most cases. They run posteriorly to the subscapularis and teres major (lower only) muscles. These are also clearly visible on the plastinated tissue.
- Axillary nerve: This nerve branches from the posterior cord and runs posterolaterally. It travels with the posterior circumflex humeral artery through a space between the surgical neck of the humerus, the long head of the triceps, teres minor, and teres major to reach the deltoid.
- Radial nerve: Observe this nerve branching from the posterior cord and running to the posterior side of the arm. It is larger than the axillary nerve.
- Ulnar nerve: The ulnar is the most medial branch of the brachial plexus, branching from the medial cord. It continues along the medial side of the arm and passes around the medial epicondyle of the humerus on its path to the forearm. This nerve is responsible for our “funny bone.” You can also see it enter the hand, and it sends branches to the skin of the 5th digit and the lateral aspect of the 4th digit. It also innervates most muscles in the hand, except the thenar eminence muscles and lateral two lumbricals. It is challenging to discern in the brachium (arm) on the plastinated tissue, but it travels around the medial epicondyle into the forearm and hand.
- Median nerve: In the axilla, the median nerve is evident as the middle nerve formed from the “M” of the brachial plexus, as it receives contributions from both the medial and lateral cords. It travels through the anterior arm and forearm to enter the hand and supply the skin of the lateral half of the 4th digit and digits 1-3 and the muscles of the thenar eminence and lateral two lumbricals. This nerve is also clearly visible on the plastinated tissue.
- Musculocutaneous nerve: The musculocutaneous nerve pierces (and supplies) the coracobrachialis muscle in the arm and then runs between the biceps brachii and brachialis muscles. It emerges on the lateral aspect of the arm as the lateral antebrachial cutaneous nerve. Be aware that the medial cord on the deep dissection abnormally pierces the coracobrachialis muscle, then sends its contribution to the median nerve. The musculocutaneous nerve then pierces the coracobrachialis again and follows its normal path. While this branching pattern is abnormal, anomalies like this frequently occur with nerves and arteries. In the plastinated tissue, this nerve is not visible in the brachium. However, you can see it emerge in the forearm as the lateral antebrachial cutaneous nerve, where it innervates the skin of the lateral forearm.
arteries of the upper extremity:
Observe the arteries of the upper extremity.
- Subclavian artery: This is the primary artery providing the arm with blood. It is not visible on the donor limbs, but a portion is visible on the full donor, and it can also be viewed in images.
- Axillary artery: This artery is continuous with the subclavian artery from the lateral border of the first rib to the inferior border of the teres major muscle. There are several branches you should be able to identify off of the axillary artery.
- Suprascapular artery: The origin of this artery has been cut, but you can observe it in the deep dissection running over the transverse scapular ligament of the suprascapular notch and traveling to the supraspinatus. This artery runs posteriorly with the suprascapular nerve to supply the supraspinatus and infraspinatus.
- Superior thoracic artery: This is the only branch off of the first part of the axillary artery. It will run inferiorly to the superior thoracic wall. It has been cut in the dissections, so you cannot follow it to its destination. It may be seen in atlas images.
- Lateral thoracic artery: This artery branches from the second part of the axillary artery and runs with the long thoracic nerve along the lateral thoracic wall to supply the lateral wall and the serratus anterior. Don’t confuse the lateral thoracic artery and the long thoracic nerve! This can be observed in atlas images.
- Thoracoacromial trunk: This is a short trunk off the superior side of the second part of the axillary artery. It branches almost immediately into four parts that supply the acromion, deltoid, pectoral muscles, and clavicle. You can see its branches traveling to the pectoralis muscles. However, the other branches of this trunk have been cut in the donor tissue.
- Posterior and anterior circumflex humeral arteries: These arteries branch from the third part of the axillary artery. They wrap around the surgical neck of the humerus and anastomose (join) with each other to provide circulation to this region via multiple routes. They sometimes branch from a common trunk, or they can branch separately from the axillary artery. The posterior circumflex humeral artery runs posteriorly around the humerus with the axillary nerve, while the anterior circumflex humeral artery runs anteriorly around the humerus.
- Subscapular artery: The subscapular artery is a short branch off of the third part of the axillary artery. As it runs inferiorly, it gives off two branches, both of which are visible on the donor tissue. You can also observe these on the plastinated tissue.
- Circumflex scapular artery: This runs posteriorly around the lateral scapula.
- Thoracodorsal artery: This artery runs with the thoracodorsal nerve to the latissimus dorsi muscle.
- Brachial artery: This artery is continuous with the axillary artery at the inferior border of the teres major. It continues through the brachium to supply muscles of the anterior arm. This can be best observed on the deep dissection and plastinated tissue.
- Deep brachial artery: This is the only branch of the brachial artery you are responsible for in this unit. It branches from the brachial artery in the mid-arm region and runs posteriorly. This is difficult to see in the donor tissue.
- Ulnar and radial arteries: The brachial artery divides into the radial and ulnar arteries in the cubital fossa. They run on the side of the antebrachium (forearm) of the bone with the same name. These are visible in the deep dissection, though the ulnar artery is cut in the forearm.
- Superficial and deep palmar arches: The superficial palmar arch is visible in the plastinated tissue, and both are visible in images. These are formed from the ulnar and radial arteries.
- Digital arteries: These branch from the superficial and deep palmar arches and travel to the sides of each digit.
Veins of the upper extremity:
Most of the veins have been removed from the dissected donor tissue. However, they are visible in atlas images and on the plastinated tissue. Two primary veins originate in the superficial forearm:
- The cephalic vein runs on the lateral aspect of the forearm and arm, while the basilic vein runs on the medial aspect of the forearm and arm.
- In the cubital fossa, the median cubital vein joins the basilic and cephalic veins. The median cubital vein is a common site for blood draws.
- The brachial vein drains the muscles of the arm and then joins the basilic vein to become the axillary vein. The cephalic vein drains into the axillary vein, and then the axillary vein becomes the subclavian vein at the border of the first rib.
Lab Activity 2: Neurovasculature of the Upper Extremity in the Visible Body Digital Atlas
Click on the tab marked Systems, then under Circulatory System Views, click 1. Circulatory System. On the left side of the screen, open the systems tab and click the venous system to DE-select it. Now you should only see the arterial system.
Explore the upper extremity arterial structure. You will need to use finger gestures to zoom and rotate the image into the best position to get the best view. Look for the following:
- Subclavian artery
- Thyrocervical trunk
- Suprascapular artery
- Axillary artery
- Superior thoracic artery
- Thoracoacromial (trunk) artery – (hide clavicle to see)
- Lateral thoracic artery
- Anterior circumflex humeral artery
- Posterior circumflex humeral artery
- Subscapular artery
- o Thoracodorsal artery
- o Circumflex scapular artery
- Brachial Artery
- Deep Brachial Artery – **labeled as profunda brachii in the digital atlas
- Radial Artery
- Ulnar Artery
Highlight each of the structures outlined above and look at the box on the upper right-hand side of the screen and review the information provided (click on the book for more information on the structure highlighted). Review as many of the visible vasculature structures as possible. Be sure to rotate the structure to appreciate multiple points of view.
Here are a few tips for identifying arteries of the axilla and arm:
- The subclavian becomes the axillary artery at the lateral border of the first rib.
- The axillary artery becomes the brachial artery at the inferior border of the teres major.
- The axillary artery is divided into three parts by the pectoralis minor muscle. The first part is medial to the muscle, the second part is deep to the muscle, and the third part is lateral to the muscle. The first part has one branch, the second part has two branches, and the third part has three branches.
Click on the tab marked Systems, then under Circulatory System Views, click 1. Circulatory System. Open the systems tab on the left side of the screen, and click the arterial system to DE-select it. Now you should only see the venous system.
Explore the upper extremity venous structures. You will need to use finger gestures to zoom and rotate the image into the best position to get the best view. Look for the following:
- Cephalic vein
- Basilic vein
- Median cubital vein
- Brachial vein
- Axillary vein
- Subclavian vein
Lab Activity 3: Brachial Plexus Exercise (Card Placement + atlas)
- On the table, you will see a poster with an unlabeled brachial plexus. You will also see labels for nerves (blue) and muscles (red). Using the visible body atlas and laminated images, first use the blue nerve labels to correctly label the brachial plexus branches. Then, using muscle charts, place the muscles next to the nerve that innervates them.
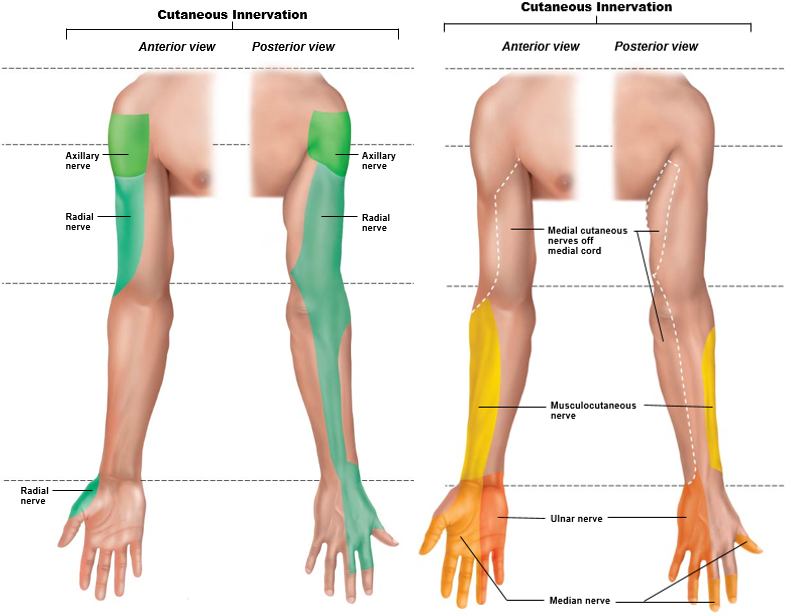
- You should also be aware of the region of skin innervated by each terminal branch of the brachial plexus. Knowing both the muscles innervated by each branch and the region of skin innervated by the terminal branches has clinical relevance. It can help you determine which nerve (or nerve root, as explained in the lecture) may be damaged. The region of skin innervated by each terminal branch of the brachial plexus is shown in this figure: