M6 | Integrative action of the sensorimotor system – Cerebellum & Basal ganglia
Basal Ganglia Disorders
Hyperkinesia
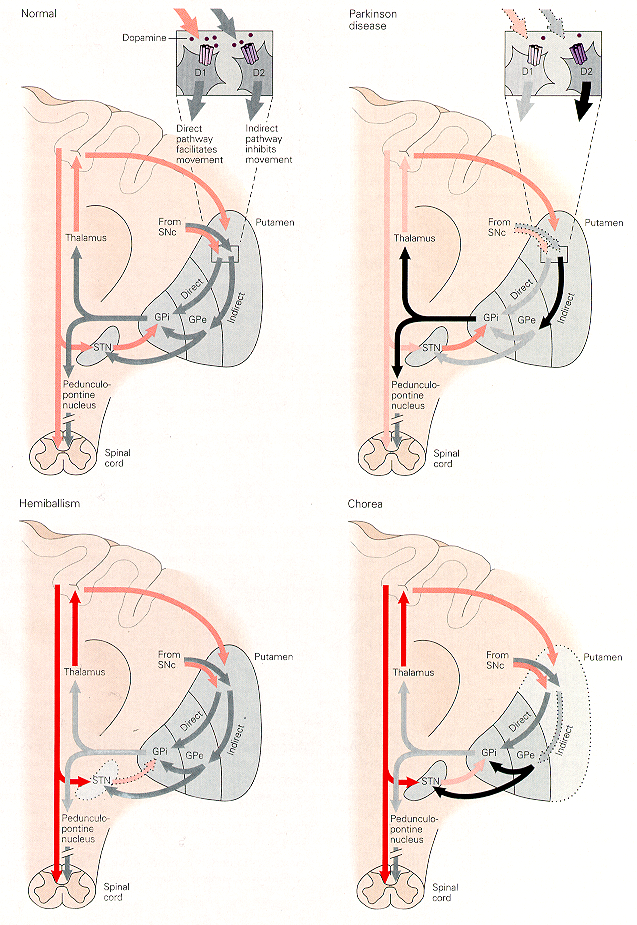
Ballism and chorea are two common hyperkinetic disorders. Ballism occurs after lesions of the STN and is characterized by uncontrollable rapid movements of the contralateral arm and leg. Lesions of the STN result in a loss of excitatory drive to the GPI and SNPR –> reduced inhibitory output of the BG –> release extra, unwanted movement.
Chorea is a major symptom of Huntington’s disease. Degeneration of the striatal neurons of the indirect pathway result in less inhibition of GPE cells –> increased inhibition of the STN. The effect of increased inhibition of STN is similar to STN lesions. Both results in excessive movement.
 Hypokinesia
Hypokinesia
Parkinson’s disease (PD) is the most common disorder of the BG and is an example of a hypokinetic disorder. PD is caused by selective degeneration of the dopaminergic innervation of the striatum from the SNPC. This has two effects:
- Removal of DA excitation to the direct pathway to the GPI, which results in reduced inhibition of GPI
- Removal of inhibition to the indirect pathway via the GPE, which results in excessive inhibition of GPE –> over activity in the STN –> excessive facilitation of the GPI.
Thus, the GPI is overactive because of reduced inhibition through the direct pathway and extra facilitation through the indirect pathway. The extra inhibitory output reduces the excitatory input from thalamic neurons to cerebral cortex and leads to hypokinesia and bradykinesia.
Symptoms of Parkinson’s disease
- Akinesia: poverty of associated and spontaneous movements.
- Face has mask-like expression
- Arms do not swing while walking
- Patients sit or stand motionless
- Tremor: especially of hands (pill-rolling). In early stages of disease this tremor disappears during movements –> rest tremor (frequency: 4-6Hz). In later stages, tremor persists during movement (action tremor, 6-8 Hz).
- Rigidity: In relaxed patients, passive manipulation of joints meets with higher resistance than normal. The increased tone is equally distributed between extensor and flexor muscles (unlike spasticity where flexor tone –> extensor tone) and may be accompanied by phenomenon called cog-wheeling. This is due to superposition of tremor onto the increased muscle tone, giving the examiner the feeling of moving the joint through a ratchet-like device.
- Bradykinesia: slowing of movement, this gives impression of a very deliberate and careful action.
- Postural instability: firm unexpected push to shoulders may easily overbalance patients. Stepping reactions are lost, and there is a failure to throw the limbs out to protect the body during falling. The result is that not only do patients with PD fall more frequently but they also damage themselves more than normal when they do fall. In addition, patients with PD have defective anticipatory postural adjustments.
Clinical management and potential treatments of Parkinson’s disease
- Increase DA level by administration of L-DOPA, a precursor of DA.
- Implantations of DA rich fetal mesencephalic brain tissue into the striatum of patients.
- Deep brain stimulation
- Stem cells
Primate model of Parkinson’s disease
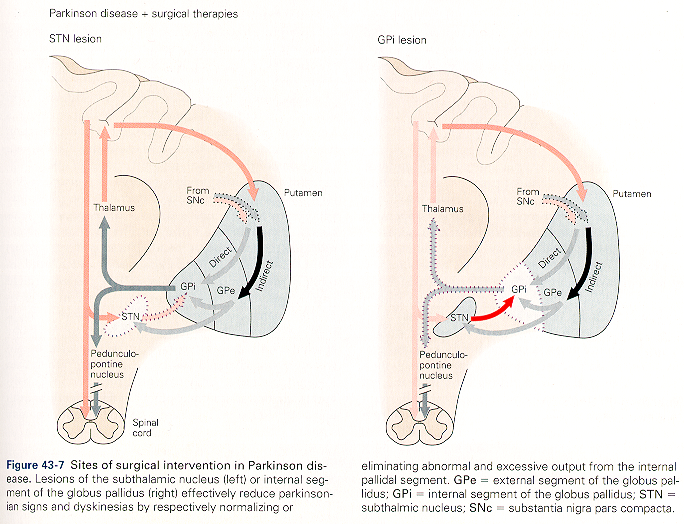
MPTP is a neurotoxin that, when administered systemically, selectively destroys the dopaminergic cells of the SNPC and causes acute, severe, and irreversible Parkinsonian symptoms. STN lesions in MPTP-induced PD can alleviate most symptoms, including tremor, rigidity, and akinesia. This is an important discovery because of the possibility of developing a new surgical or pharmacological treatment for PD involving inactivation of the STN.

