Module 13: Heart and Great Vessels
Learning Objectives:
By the end of this class, students will be able to:
- Explain the internal and external anatomy of the heart.
- Describe the pericardium, including its layers, and its functions.
- Distinguish how valves regulate blood flow through the heart.
- Outline the pattern of blood flow through the heart.
- Identify and describe the location, origins, and branches of the coronary blood vessels.
- Describe the general pattern of circulation.
- Describe electrical conduction through the heart.
- Identify and describe the great vessels carrying blood immediately to and from the heart and the major vessels of the thoracic, abdominal, and pelvic cavities.
Terms to Know
General
Pericardium
Heart Anatomy
Heart Development
Cardiac Cycle
*Covered only in lecture, not in this text |
Coronary Circulation
Innervation and Conducting System of the Heart
Great Vessels
|
Introduction to the Heart
This content is primarily covered in the reading and assignment as self-study. It will be only briefly reviewed in lecture.
The heart is located within the thoracic cavity, medially between the lungs in the mediastinum. The dorsal surface of the heart lies near the bodies of the vertebrae, and its anterior surface sits deep to the sternum and costal cartilages. The great veins, the superior and inferior venae cavae, and the great arteries, the aorta and pulmonary trunk, are attached to the superior surface of the heart, called the base. The inferior tip of the heart, the apex, lies just to the left of the sternum, and the right surface of the heart sits inferiorly on the diaphragm.
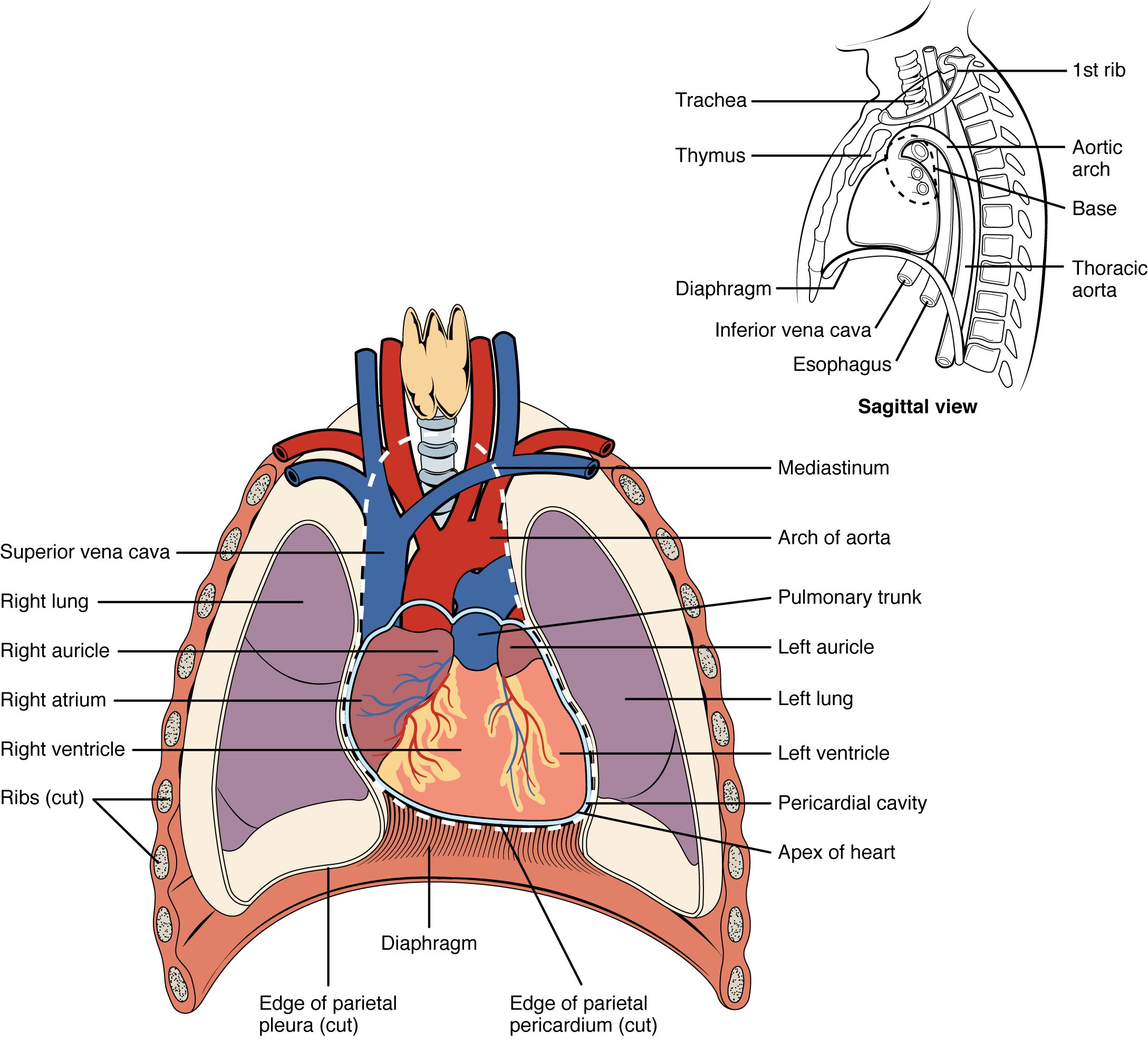
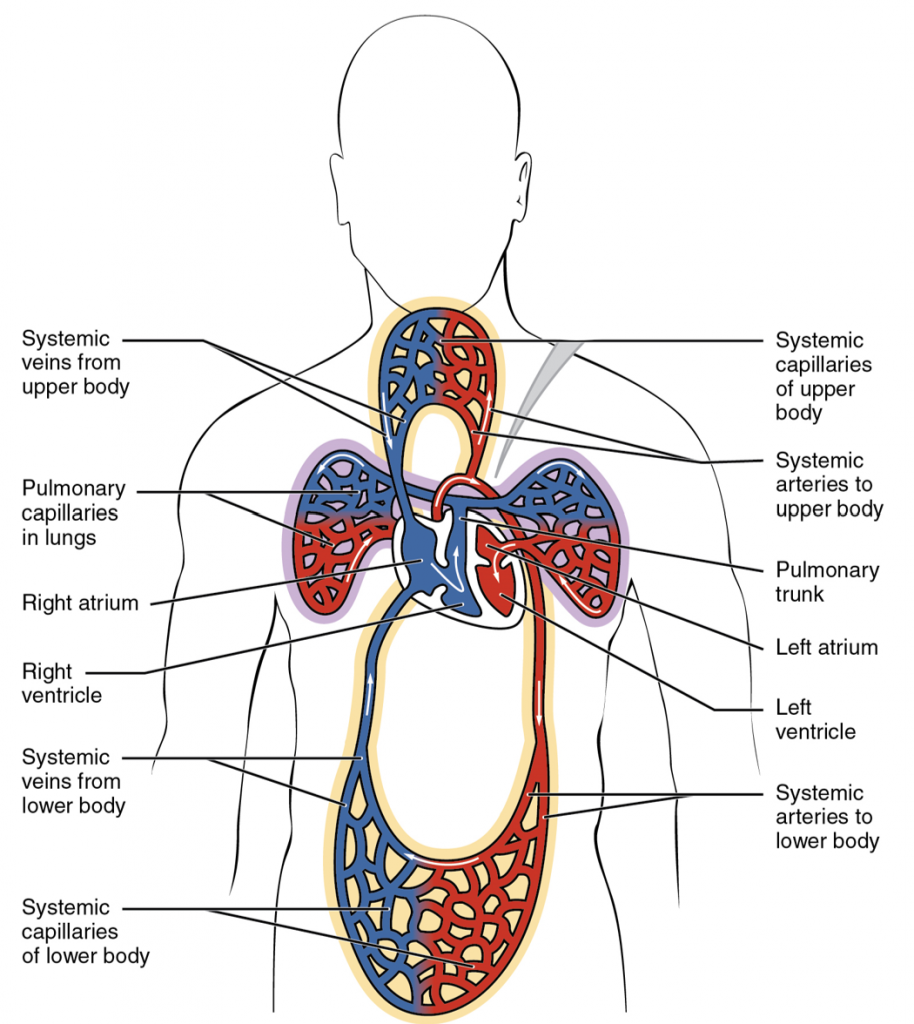
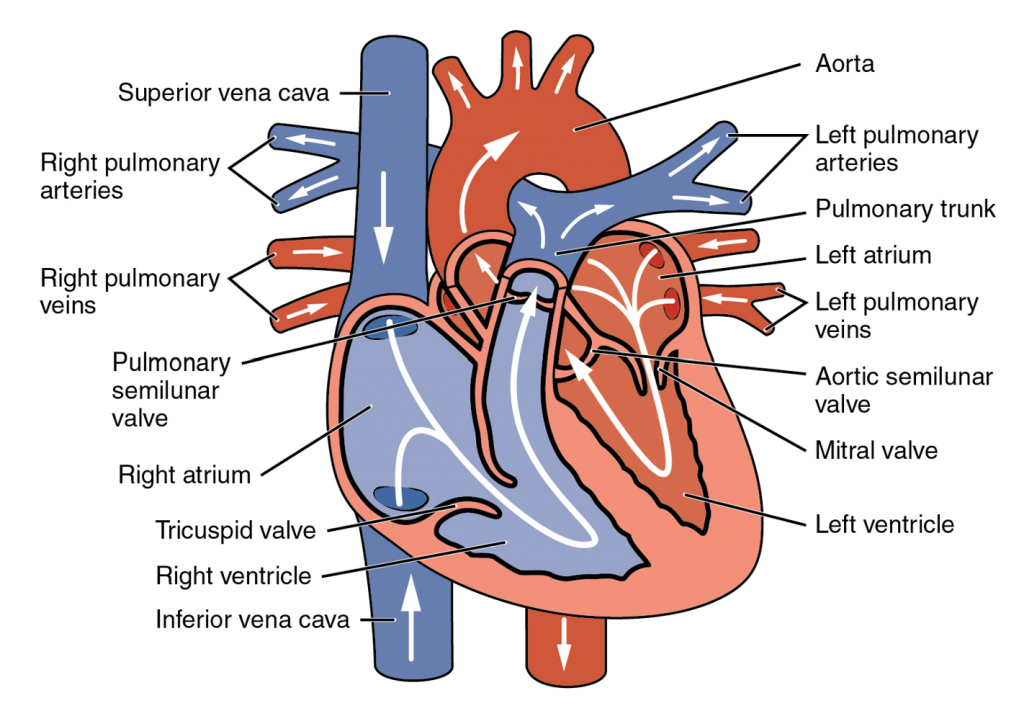
There are two distinct but linked circuits in the cardiovascular system called the pulmonary and systemic circuits. Pulmonary circulation transports blood to and from the lungs, where it picks up oxygen and delivers carbon dioxide for exhalation. Systemic circulation transports oxygenated blood to virtually all of the tissues of the body and returns relatively deoxygenated blood and carbon dioxide to the heart to be sent back to the pulmonary circulation.
THe Pericardium and the heart wall
This content is covered in the assignment and reviewed and built upon in lecture.
Within the mediastinum, the heart is separated from the other mediastinal structures by a tough membrane known as the pericardium, or pericardial sac. The pericardium consists of two distinct sublayers:
-
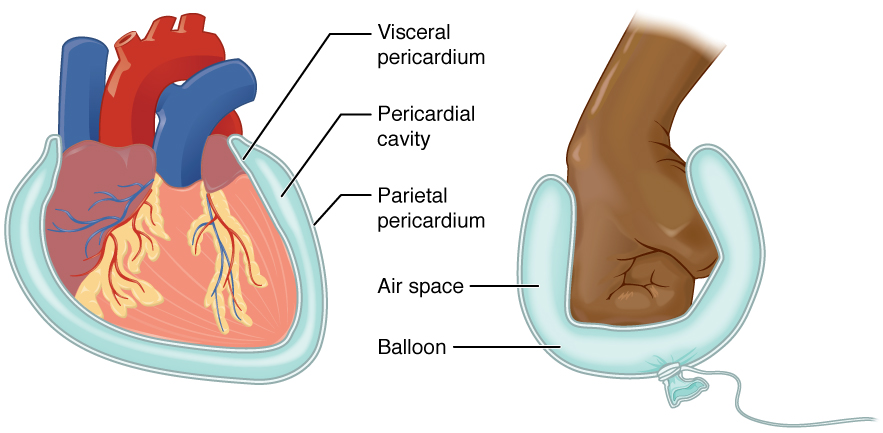
The Pericardium: The pericardium is the serous membrane that encloses the pericardial cavity and reflects back to cover the heart—much the same way that an underinflated balloon would form two layers surrounding a fist. The pericardial cavity reduces friction between the heart and the wall of the pericardium. Fibrous pericardium: This is the tough outer layer made of dense connective tissue that protects the heart and maintains its position in the thorax.
- Serous pericardium: The inner serous pericardium consists of two layers designed in a similar way to the pleura surrounding the lungs and the peritoneum of the abdominopelvic cavity:
-
- Parietal pericardium: This is the outer layer of the serous pericardium, and it is fused to the fibrous pericardium.
- Visceral pericardium: This inner layer lines the heart itself. It actually forms part of the heart wall, called the epicardium (more on that later).
The parietal and visceral layers of pericardium are continuous with each other, forming a thin, flat sac. The thin space within this sac is called the pericardial cavity, and it is filled with lubricating serous fluid that cushions and reduces friction on the heart as it beats.
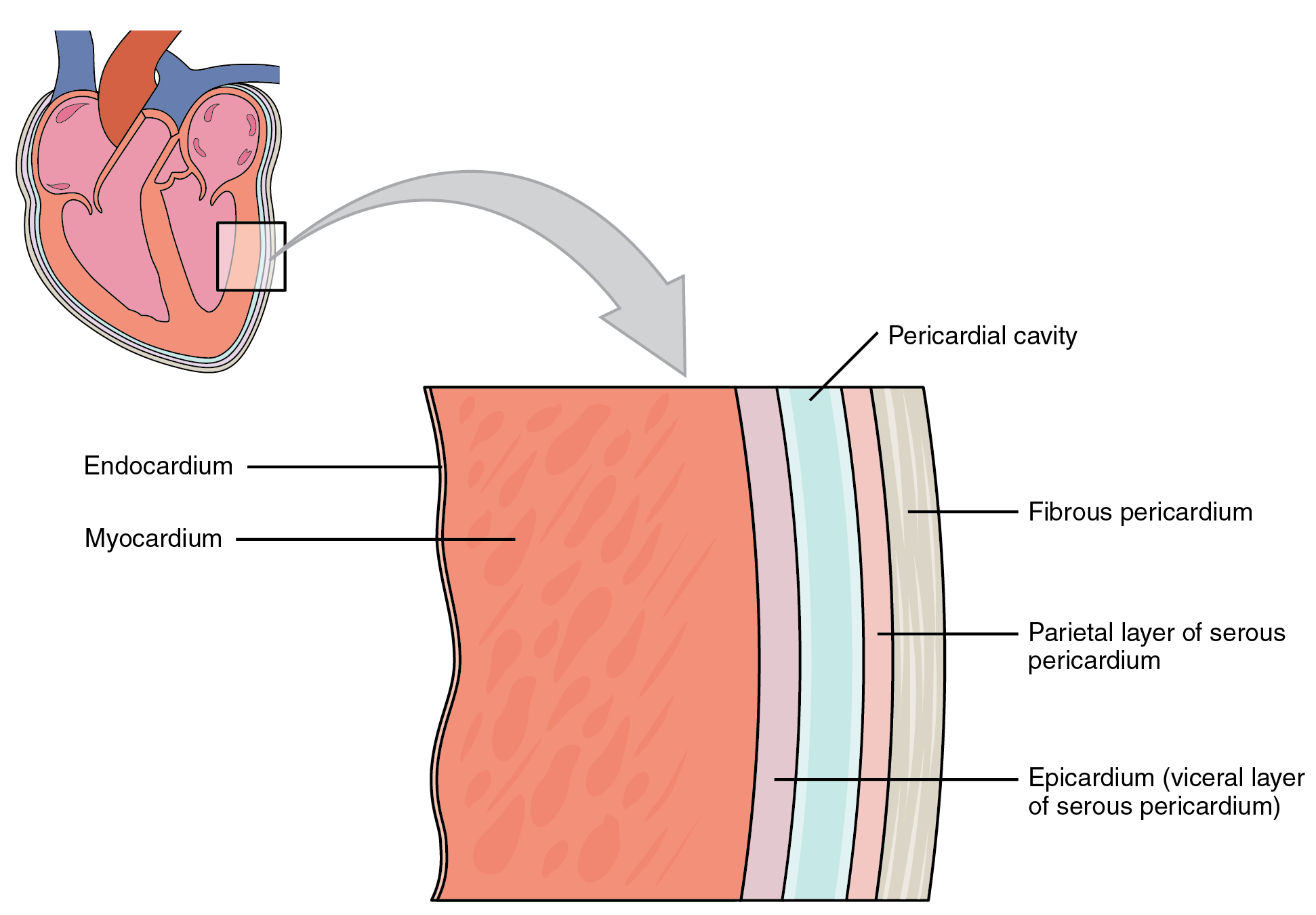
The wall of the heart is composed of three layers of unequal thickness. From superficial to deep, these are the:
-
Heart Musculature: The swirling pattern of cardiac muscle tissue contributes significantly to the heart’s ability to pump blood effectively. Epicardium: The outermost layer of the wall of the heart is also the innermost layer of the serous pericardium, or the visceral pericardium discussed earlier.
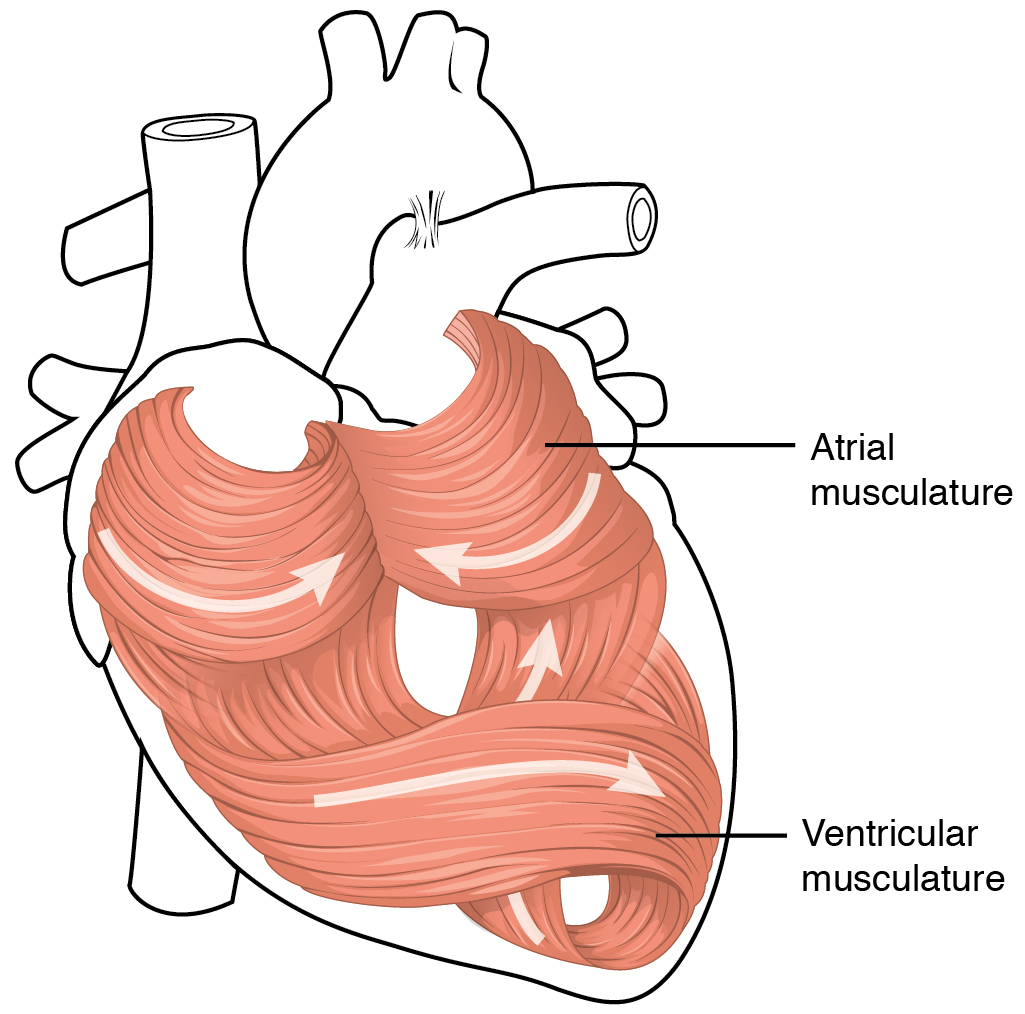
- Myocardium: This is the middle and thickest of the heart wall. It is composed of the heart muscle, or cardiac myocytes. Contraction of the myocardium pumps blood through the heart and into the major arteries. The muscle cells are arranged in a figure 8 pattern around the atria and ventricles, allowing the heart to squeeze and pump blood more effectively than a simple linear pattern would.
- Endocardium: This inner layer of the heart wall lines the chambers where the blood circulates and covers the heart valves. It is made of simple squamous epithelium called endothelium, which is continuous with the endothelial lining of the blood vessels.
Chambers and Circulation through the Heart
 This content is covered in the assignment and reviewed and built upon in lecture.
This content is covered in the assignment and reviewed and built upon in lecture.
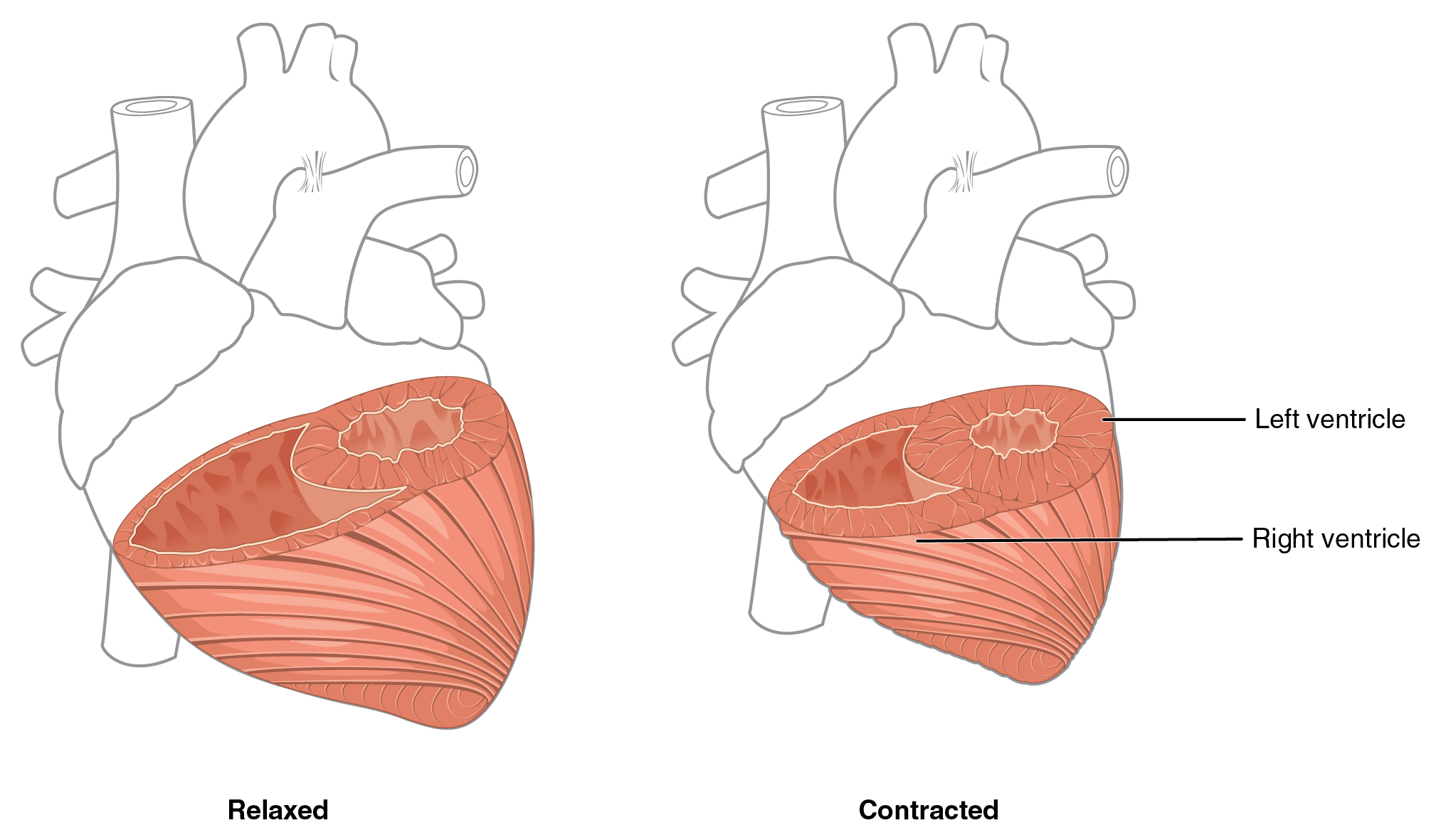
The human heart consists of four chambers. Each of the upper chambers, the right and left atria, acts as a receiving chamber and contracts to push blood into the lower chambers, the right and left ventricles. There is a superficial extension of the atria near the superior surface of the heart, one on each side, called an auricle (someone once thought it looked like an ear).
The ventricles serve as the primary pumping chambers of the heart, propelling blood to the lungs or to the rest of the body. Although the ventricles on the right and left sides pump the same amount of blood per contraction, the muscle of the left ventricle is much thicker and better developed than that of the right ventricle. In order to pump blood into the long systemic circuit, the left ventricle must generate a great amount of pressure. The right ventricle does not need to generate as much pressure, since the pulmonary circuit is shorter. The walls of both ventricles are lined with trabeculae carneae, ridges of cardiac muscle covered by endocardium.
The septa are muscular walls located between chambers of the heart.
- Interatrial septum: between the atria. It contains the fossa ovalis in the adult heart, the remnant the fetal opening called the foramen ovale. (See more in the Heart Development section.)
- Interventricular septum: between the ventricles. It is substantially thicker than the interatrial septum, since the ventricles generate far greater pressure when they contract.
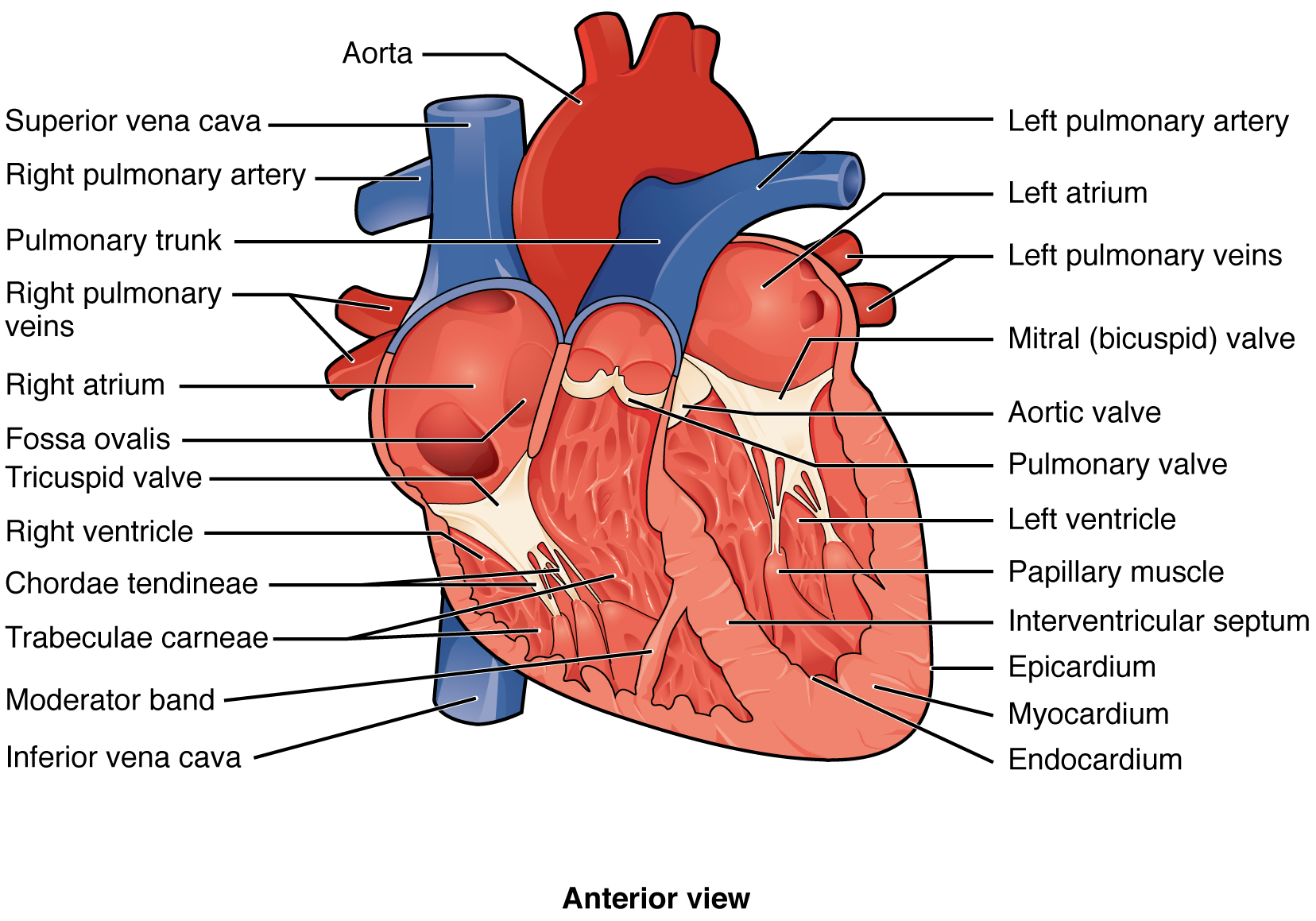
Right Atrium
The right atrium serves as the receiving chamber for blood returning to the heart from the systemic circulation. The two major systemic veins, the superior and inferior venae cavae, and the large coronary vein called the coronary sinus that drains the heart myocardium empty into the right atrium. The superior vena cava drains blood from regions superior to the diaphragm: the head, neck, upper limbs, and the thoracic region. The inferior vena cava travels alongside the descending aorta and drains blood from areas inferior to the diaphragm: the lower limbs and abdominopelvic region of the body. The coronary sinus drains most of the coronary veins that return systemic blood from the heart. The right atrium also has parallel muscular ridges called pectinate muscles.
Right Ventricle
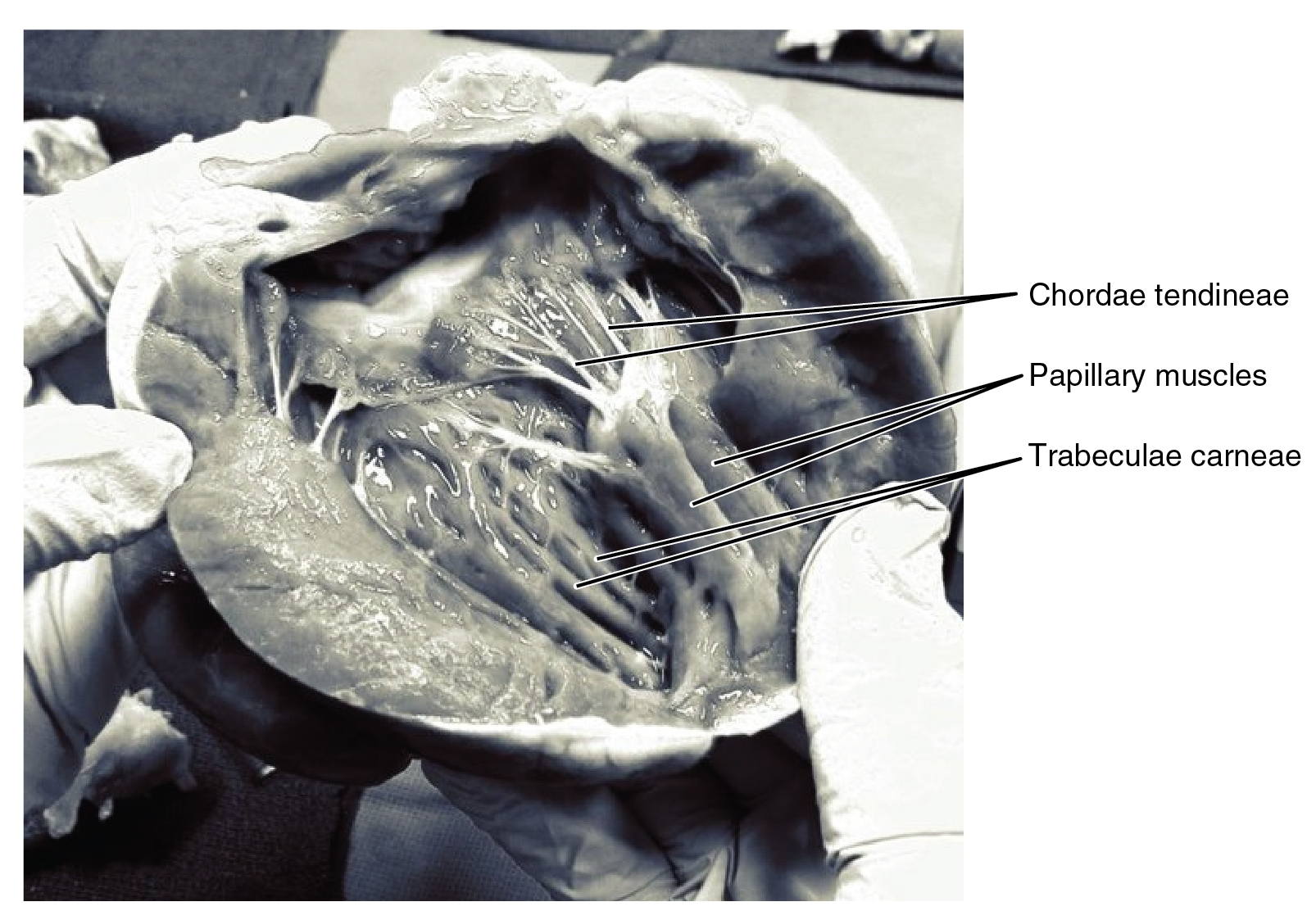
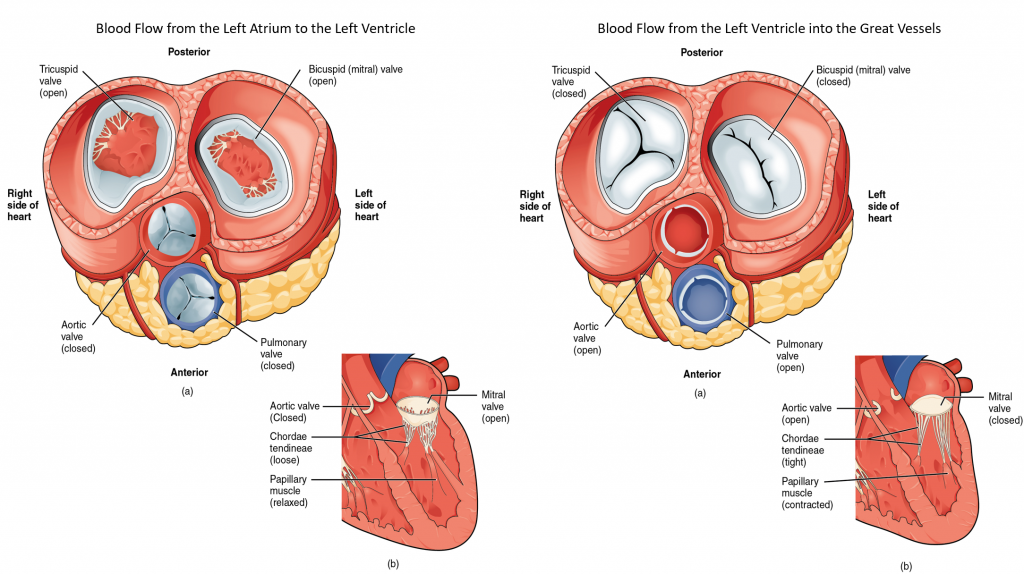
The right ventricle receives blood from the right atrium through the right atrioventricular, or tricuspid valve. Each flap of the valve is attached to several strong strands of connective tissue, the chordae tendineae. They connect each of the flaps to a papillary muscle that extends from the inferior ventricular surface.
When the myocardium of the ventricle contracts, pressure within the ventricular chamber rises. Blood, like any fluid, flows from higher pressure to lower pressure areas, in this case, toward the pulmonary trunk and the atrium. To prevent any potential backflow, the papillary muscles also contract, generating tension on the chordae tendineae. This prevents the flaps of the valves from being forced into the atria and regurgitation of the blood back into the atria during ventricular contraction.
When the right ventricle contracts, it ejects blood into the pulmonary trunk, which branches into the left and right pulmonary arteries that carry it to each lung. At the base of the pulmonary trunk is the pulmonary semilunar valve that prevents backflow from the pulmonary trunk.
Left Atrium
After exchange of gases in the pulmonary capillaries, blood returns to the left atrium high in oxygen via one of the four pulmonary veins. When the left atrium contracts, blood is pumped into the ventricle, though some blood naturally enters the left ventricle as it relaxes, without the push from the left atrium.
Left Ventricle
The left atrioventricular, or bicuspid, or mitral valve, is connected to papillary muscles via chordae tendineae. Recall that, although both sides of the heart will pump the same amount of blood, the muscular layer is much thicker in the left ventricle compared to the right.
The left ventricle is the major pumping chamber for the systemic circuit; it ejects blood into the aorta through the aortic semilunar valve.
Heart Valve Structure and Function
The valves are specialized structures that ensure unidirectional blood flow through the heart. Between the right atrium and the right ventricle is the right atrioventricular valve, or tricuspid valve. It typically consists of three flaps, or leaflets, made of endocardium reinforced with additional connective tissue. The flaps are connected by chordae tendineae to the papillary muscles, which control the opening and closing of the valves.
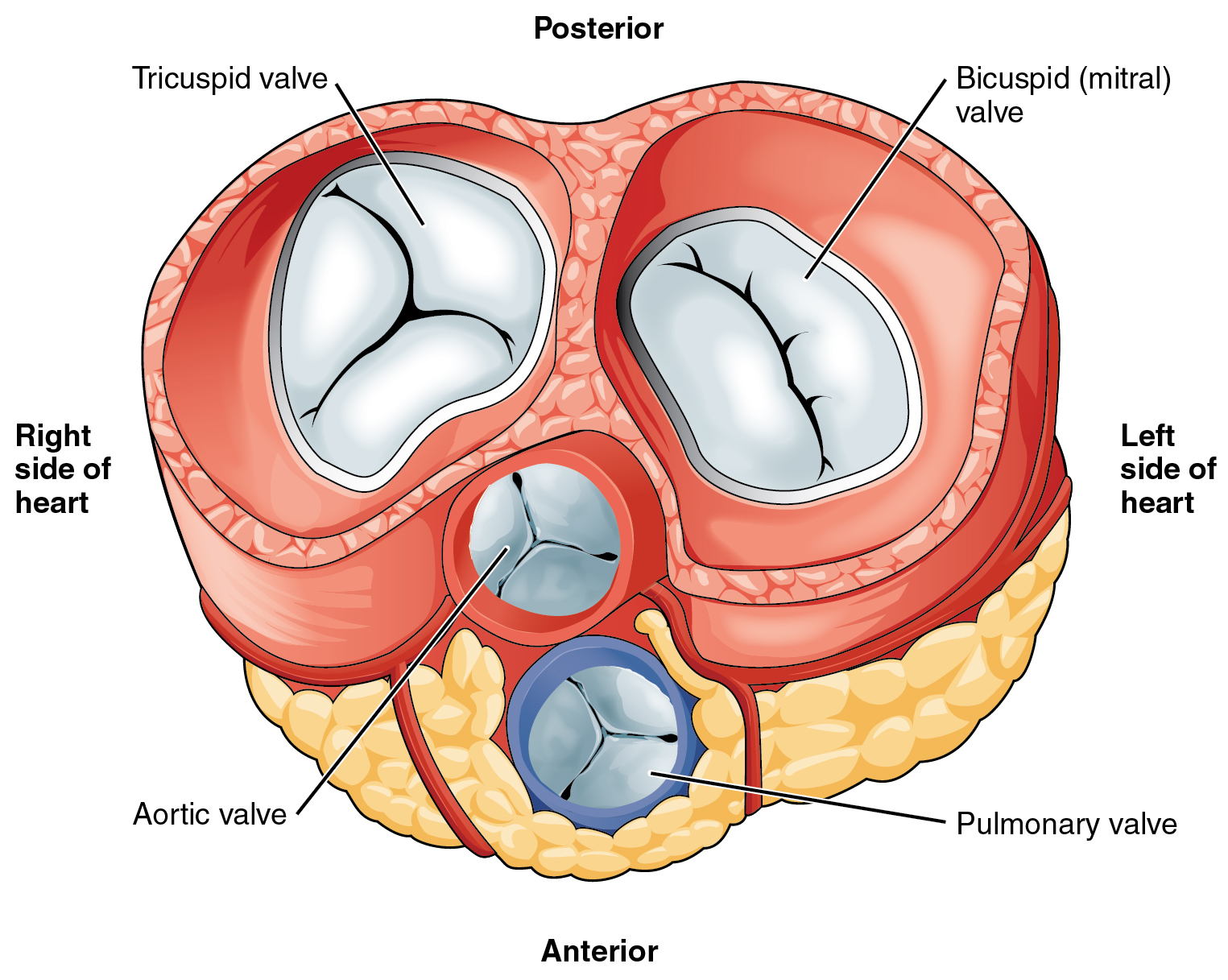
Emerging from the right ventricle at the base of the pulmonary trunk is the pulmonary semilunar valve. It is comprised of three small flaps of endothelium reinforced with connective tissue. When the ventricle relaxes, the pressure differential causes blood to flow back into the ventricle from the pulmonary trunk. This flow of blood fills the pocket-like flaps of the pulmonary semilunar valve, causing the valve to close. Unlike the atrioventricular valves, there are no papillary muscles or chordae tendineae associated with the pulmonary valve.
Located at the opening between the left atrium and left ventricle is the mitral valve, also called the bicuspid valve or the left atrioventricular valve. Structurally, this valve consists of two cusps, compared to the three cusps of the tricuspid valve. In a clinical setting, the valve is referred to as the mitral valve, rather than the bicuspid valve. The two cusps of the mitral valve are attached by chordae tendineae to two papillary muscles that project from the wall of the ventricle.
At the base of the aorta is the aortic semilunar valve, which prevents backflow from the aorta. It normally is composed of three flaps. When the ventricle relaxes and blood attempts to flow back into the ventricle from the aorta, blood will fill the cusps of the valve, causing it to close.
Cardiac Cycle
This content will be covered in lecture.
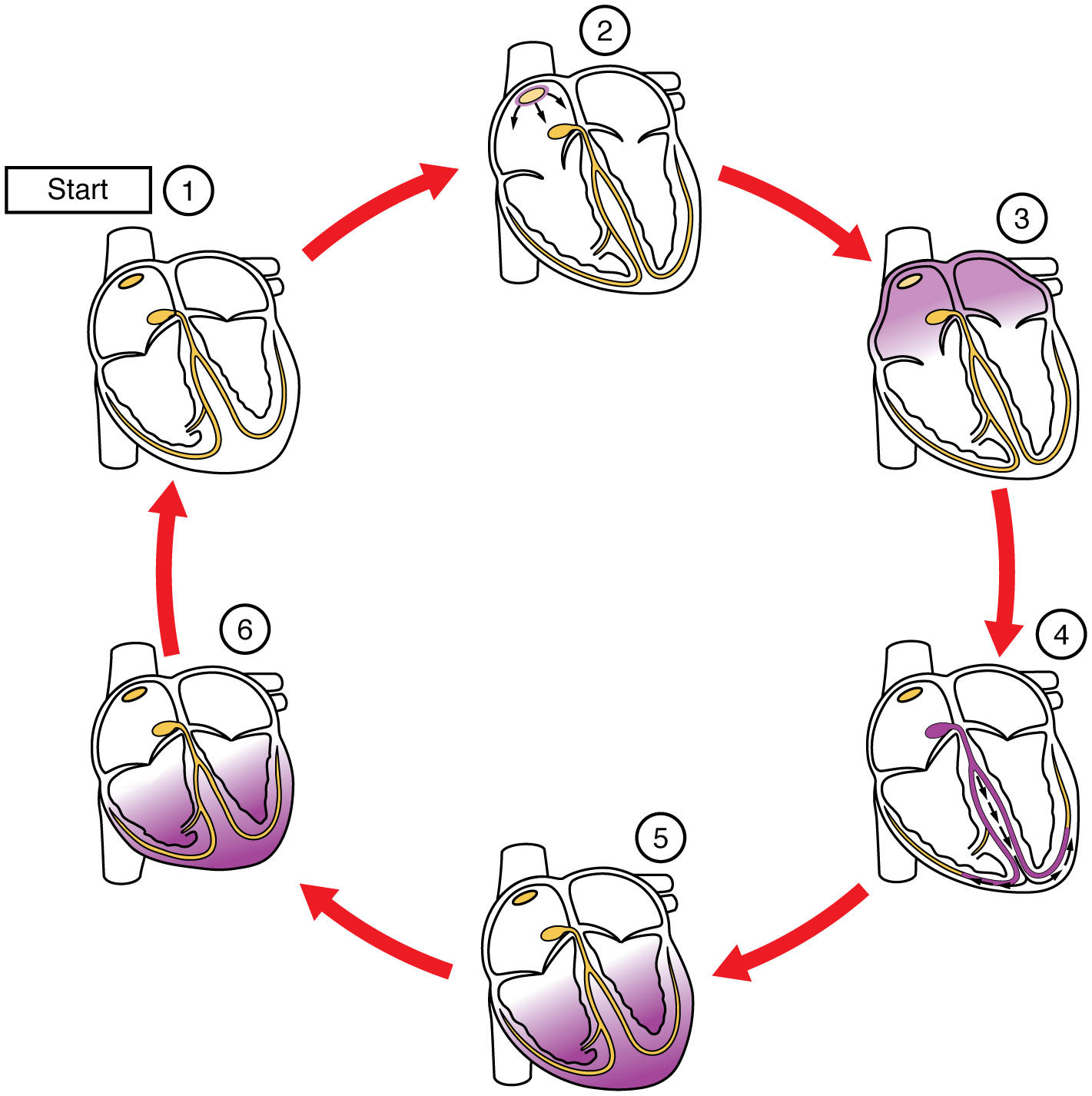
The period of time that begins with contraction of the atria and ends with ventricular relaxation is known as the cardiac cycle. The period of contraction that the heart undergoes while it pumps blood into circulation is called systole. The period of relaxation that occurs as the chambers fill with blood is called diastole.
Both the atria and ventricles undergo systole and diastole, and these components are carefully coordinated to ensure blood is pumped efficiently to the body.
- When the atria are in systole (contracting), the ventricles are in diastole (relaxed). The atrioventricular valves will be open to allow blood to flow from the atria into the ventricles as the atria contract. The semilunar valves will be closed to prevent the blood in the aorta and pulmonary trunk from flowing backwards into the relaxed ventricles.
- When the ventricles are in systole, the atria are in diastole. The atrioventricular valves will be closed to prevent blood from flowing backwards into the atria as the ventricles contract. The semilunar valves will be open to allow blood to flow into the aorta and pulmonary trunk as the ventricles contract.
A Review of Blood Flow Through the Heart
This content is primarily self-study and will be built upon and applied to cases in lecture.
The right ventricle pumps deoxygenated blood into the pulmonary trunk, which bifurcates (splits into two parts) into the left and right pulmonary arteries that carry blood to the lungs. These vessels in turn branch many times before reaching the pulmonary capillaries, where gas exchange occurs. The pulmonary trunk, arteries, and their branches are the only arteries that carry relatively deoxygenated blood. Highly oxygenated blood returns to the heart via the pulmonary veins—the only veins in the body that carry highly oxygenated blood. The pulmonary veins conduct blood into the left atrium, which pumps the blood into the left ventricle. The left ventricle pumps oxygenated blood into the aorta and on to the many branches of the systemic circuit.
Blood returning to the heart travels through one of two major systemic veins, the superior vena cava and the inferior vena cava, which return blood to the right atrium (except for blood returning from the heart wall itself, more on that later). The blood in the superior and inferior venae cavae flows into the right atrium, which pumps blood into the right ventricle.
Heart Development
This content will be covered in lecture.
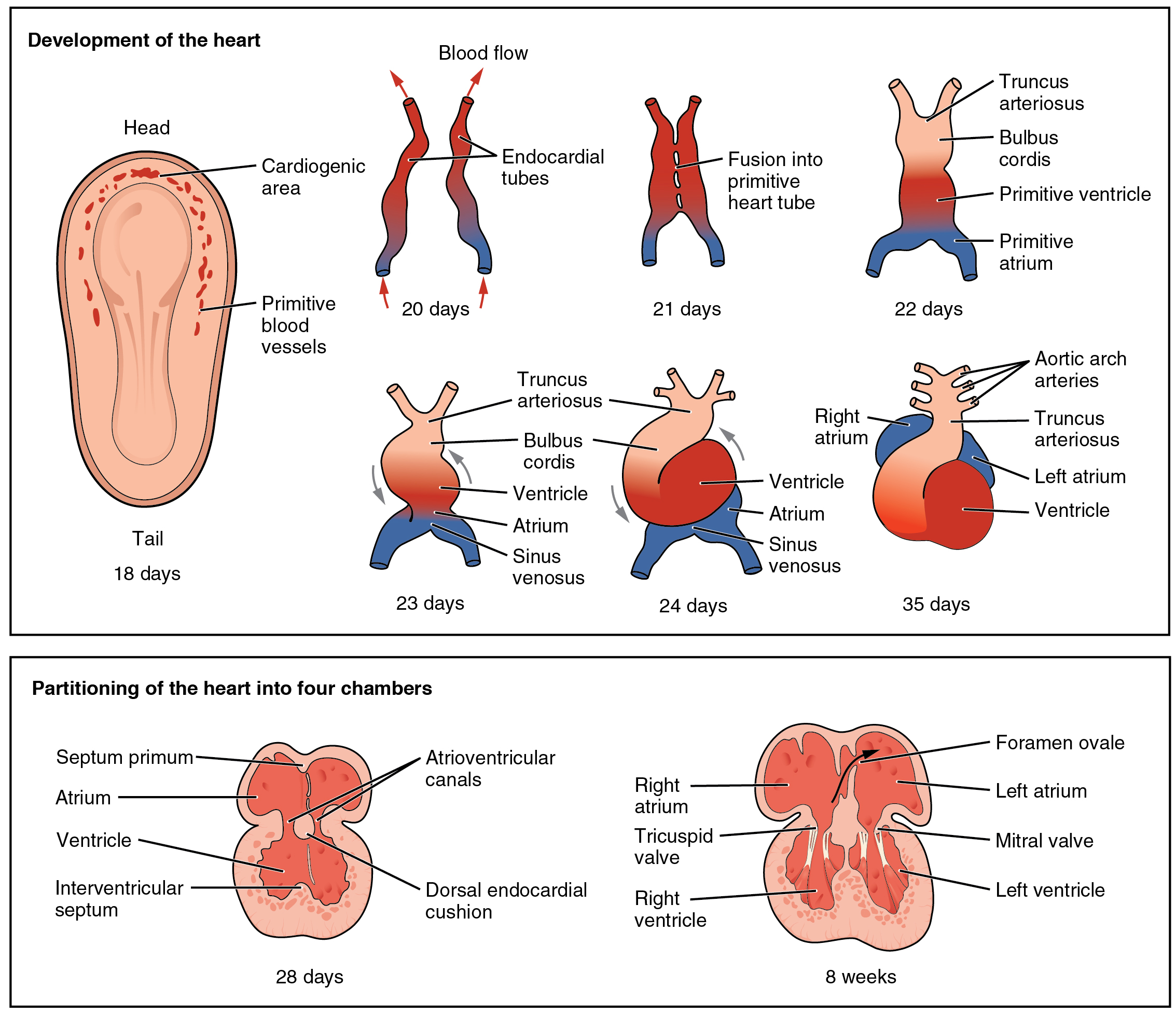
The human heart is the first functional organ to develop. It begins beating around day 21 or 22. This emphasizes the critical nature of the heart in distributing blood with vital nutrients and oxygen and removing wastes throughout the developing baby.
The heart begins as two separate tubes. The tubes fuse to form a single primitive heart tube. As the primitive heart tube elongates, it begins to fold, eventually forming an S shape, which places the chambers and major vessels into an alignment similar to the adult heart.
The Fetal Circulatory System
This content will be covered in lecture.
During prenatal development, the fetus receives oxygen and nutrients from the placenta. As a result, the fetal cardiovascular system includes circulatory shortcuts, or shunts, that allow blood flow to bypass immature organs such as the lungs and liver until childbirth.
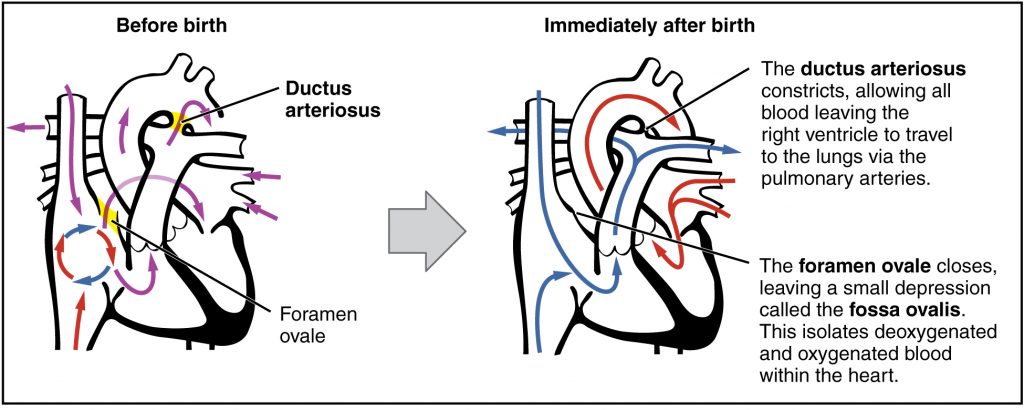
The fetal lungs are nonfunctional, so fetal circulation bypasses the lungs by sending some of the blood through the foramen ovale, a shunt that directly connects the right and left atria. It allows blood to move directly from the right atrium to the left atrium, avoiding the pulmonary circuit. From the left atrium, blood travels to the left ventricle and out into systemic circulation.
A second shunt, the ductus arteriosus, connects and diverts blood directly from the pulmonary artery to the aorta. This ensures that only a small volume of oxygenated blood passes through the immature pulmonary circuit.
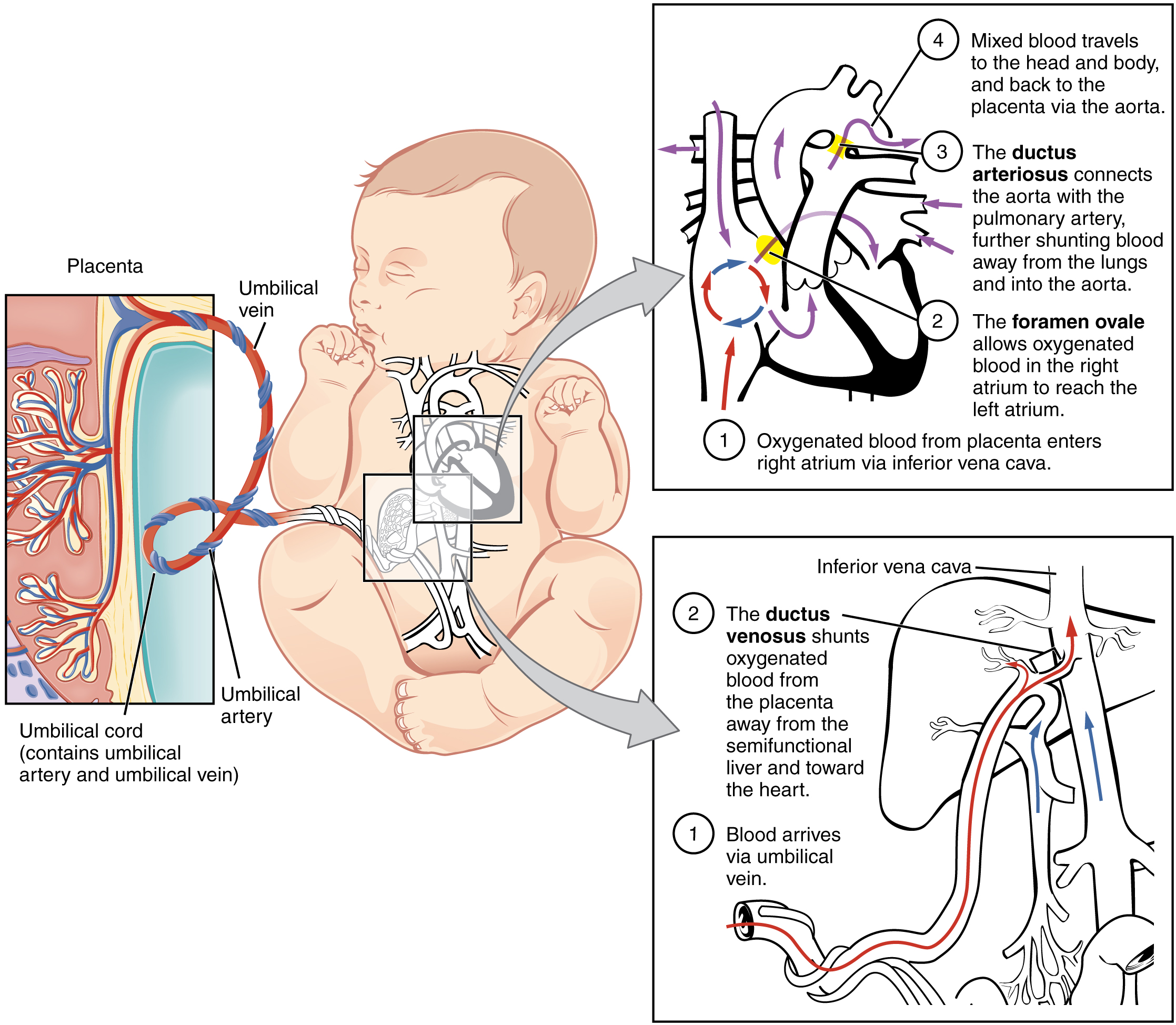
As the newborn takes its first breath, inflation of the lungs decreases blood pressure in the pulmonary circuit. This causes blood flow through the foramen ovale to reverse, and two flaps of tissue move over this opening, blocking it. This occurs soon after birth, and the tissue usually fuses over the following months, turning the foramen ovale into the fossa ovalis. The ductus arteriosus constricts, flattens, and becomes the ligamentum arteriosum. Closing of the foramen ovale and ductus arteriosus establishes the adult pattern of circulation through the heart and ensures blood travels to the lungs for oxygenation.
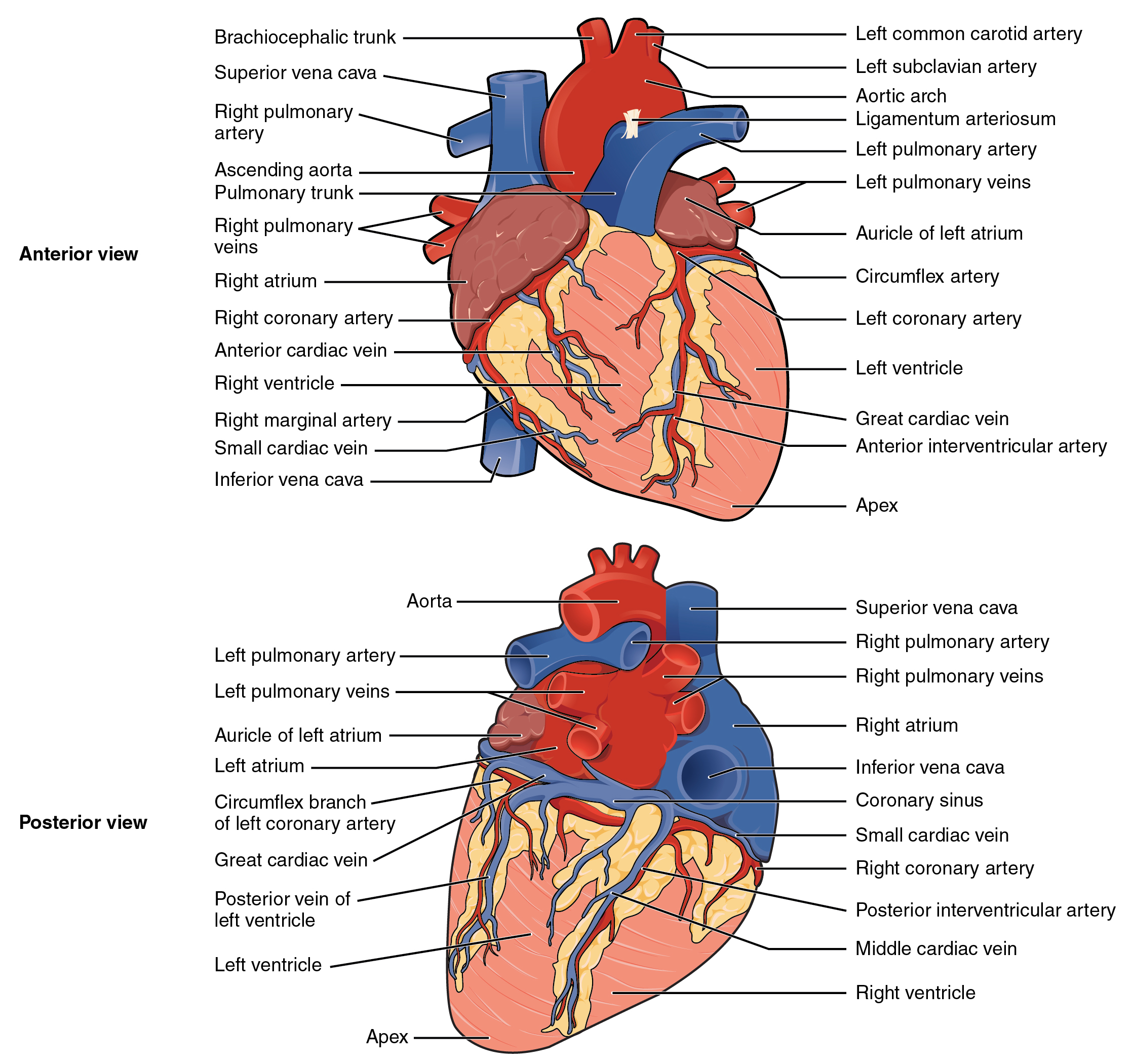
Coronary Circulation
This content will be covered in lecture.
The surface of the heart has several fat-filled grooves called sulci (singular = sulcus). Major coronary vessels are located in these sulci. The deep coronary sulcus is located between the atria and ventricles. Located between the left and right ventricles are two additional sulci that are not as deep. The anterior interventricular sulcus is visible on the anterior surface of the heart, whereas the posterior interventricular sulcus is visible on the posterior surface of the heart.
Cardiomyocytes require a reliable supply of oxygen and nutrients, and a way to remove wastes, so it needs a dedicated, complex, and extensive coronary circulation. Coronary arteries supply blood to the myocardium and other components of the heart.
The first portion of the aorta after it arises from the left ventricle gives rise to the coronary arteries.
- The left coronary artery distributes blood to the left side of the heart, the left atrium and ventricle, and the interventricular septum.
- The circumflex artery arises from the left coronary artery and follows the coronary sulcus to the left to supply the left atrium and ventricle.
- The larger anterior interventricular artery, also known as the left anterior descending artery (LAD) follows the anterior interventricular sulcus. It supplies that anterior aspect of the ventricles and the interventricular septum.
- The right coronary artery proceeds along the coronary sulcus and distributes blood to the right atrium, portions of both ventricles, and the heart conduction system.
- The right marginal artery supplies blood to the superficial portions of the right ventricle.
- On the posterior surface of the heart, the right coronary artery gives rise to the posterior interventricular artery, also known as the posterior descending artery. It runs along the posterior portion of the interventricular sulcus toward the apex of the heart, suppling the interventricular septum and portions of both ventricles.
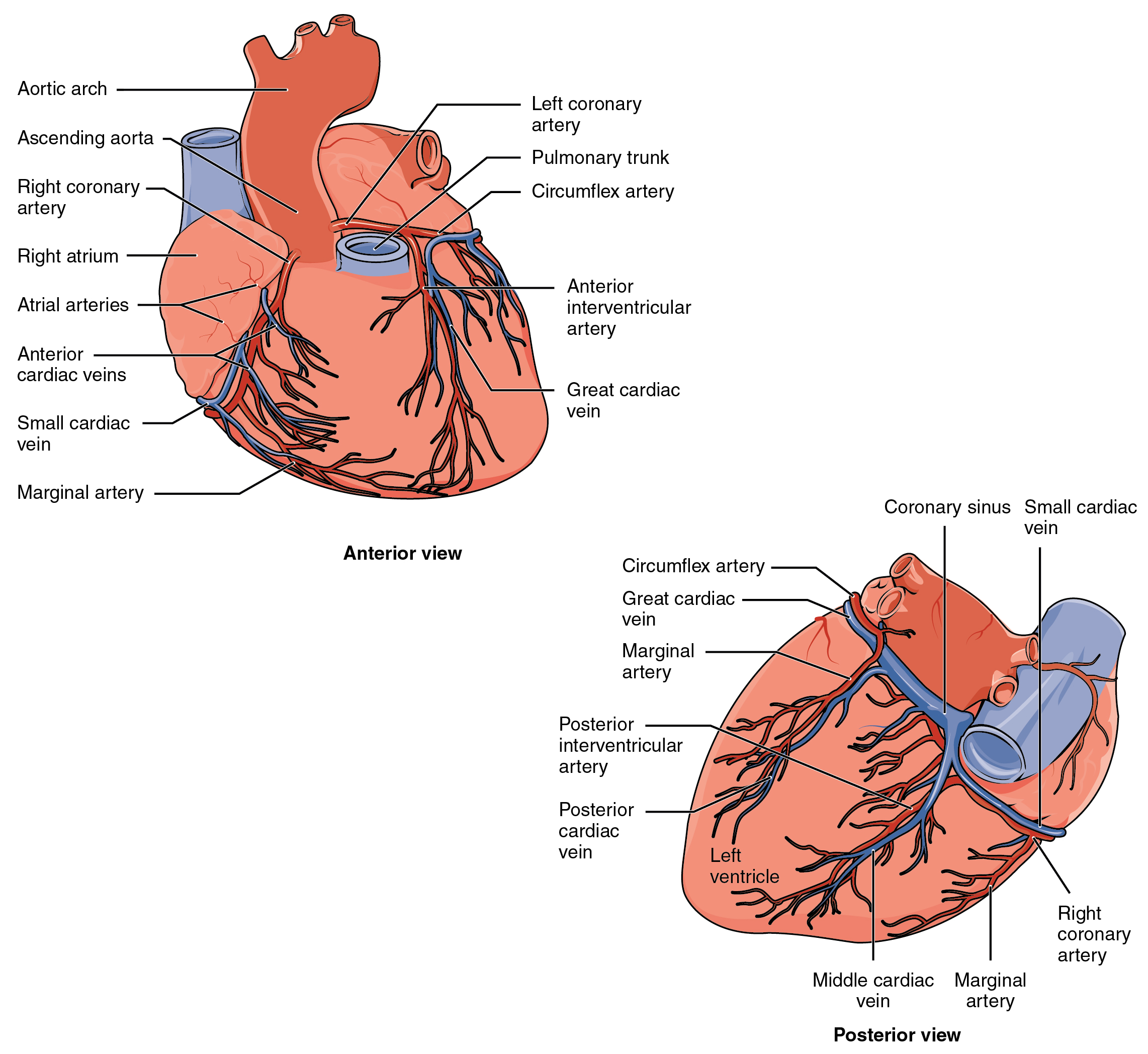
Coronary veins drain the heart and generally parallel the arteries. The great cardiac vein parallels the anterior interventricular artery and drains the areas supplied by this vessel. The middle cardiac vein parallels and drains the areas supplied by the posterior interventricular artery. The small cardiac vein parallels the right coronary artery and drains the blood from the posterior surfaces of the right atrium and ventricle. The coronary sinus is a large, thin-walled vein on the posterior surface of the heart lying within the atrioventricular sulcus and emptying directly into the right atrium. The coronary veins drain into the coronary sinus.
The Conduction System and Autonomic Innervation of the Heart
 This content will be covered in lecture.
This content will be covered in lecture.
Cardiac muscle has the ability to initiate an electrical potential at a fixed rate that spreads rapidly from cell to cell to trigger the contractile mechanism. This property is known as autorhythmicity. The components of the cardiac conduction system include the sinoatrial node, the atrioventricular node, the atrioventricular bundle, the atrioventricular bundle branches, and the Purkinje cells. The gap junctions and intercalated discs of the cardiac myocytes allow the signal to propagate easily and quickly from cell to cell, helping the myocytes contract synchronously.
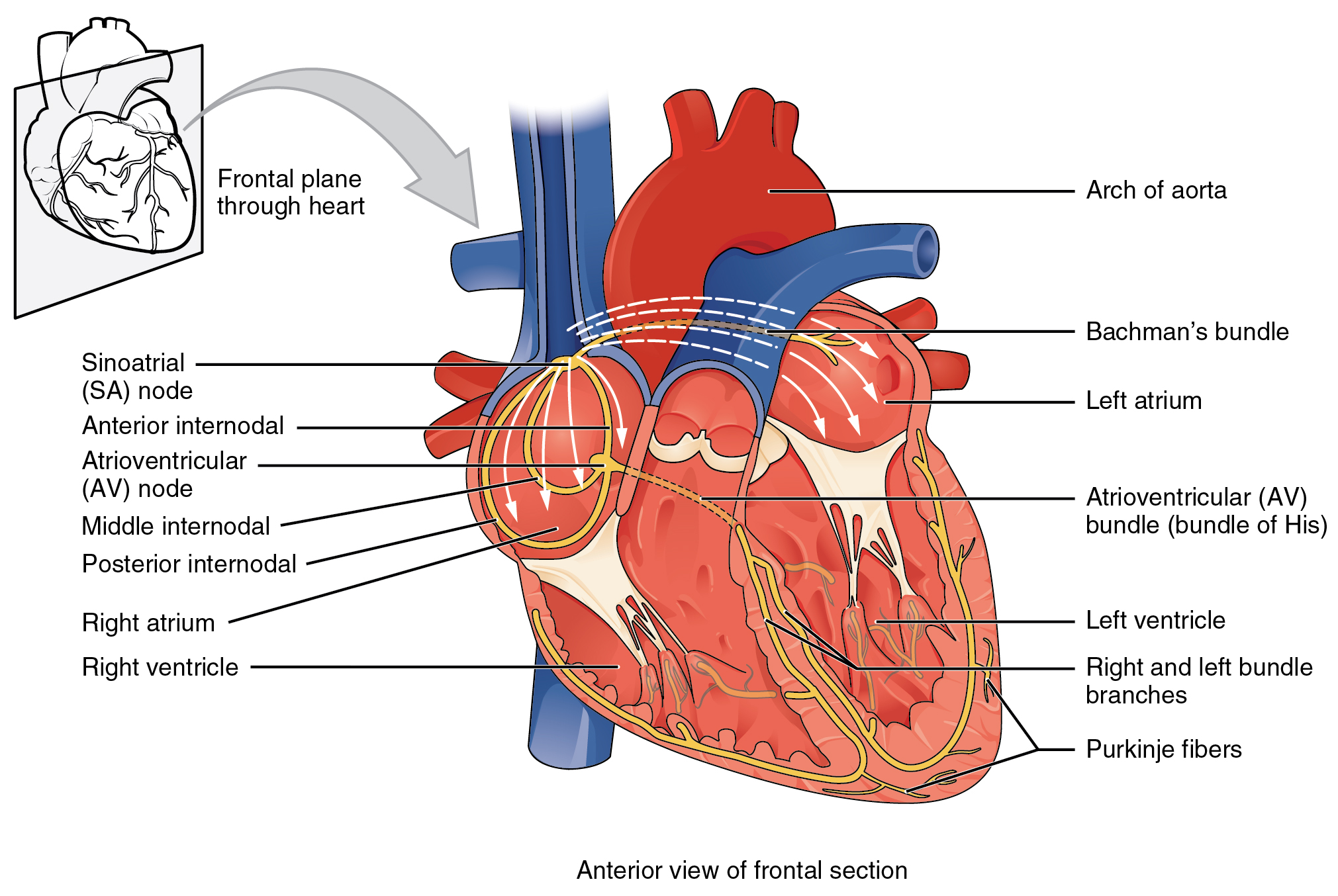
- Normal cardiac rhythm is established by the sinoatrial (SA) node, located in the superior and posterior walls of the right atrium. The SA node is known as the pacemaker of the heart. It initiates the sinus rhythm, or normal electrical pattern followed by contraction of the heart.
- This impulse spreads from its initiation in the SA node throughout the atria through internodal pathways, to the atrioventricular node.
- The atrioventricular (AV) node is located in the inferior portion of the right atrium within the atrioventricular septum. The septum prevents the impulse from spreading directly to the ventricles without passing through the AV node. There is a critical pause of about 100 ms before the AV node depolarizes and transmits the impulse to the atrioventricular bundle. This pause is critical to heart function, as it allows the atria to complete their contraction that pumps blood into the ventricles before the impulse is transmitted to the the ventricles.
- Arising from the AV node, the atrioventricular bundle, or bundle of His, travels through the interventricular septum before dividing into the left and right bundle branches. The left bundle branch supplies the left ventricle, and the right bundle branch the right ventricle. Both bundle branches descend and reach the apex of the heart where they connect with the Purkinje fibers.
- The Purkinje fibers are additional myocardial conductive fibers that spread the impulse to the myocardial contractile cells in the ventricles. They extend throughout the myocardium from the apex of the heart toward the atrioventricular septum and the base of the heart. Since the electrical stimulus begins at the apex, the contraction also begins at the apex and travels toward the base of the heart, similar to squeezing a tube of toothpaste from the bottom. This allows the blood to be pumped out of the ventricles and into the aorta and pulmonary trunk.
Autonomic Control of Heart Rate
 This content will be covered in lecture.
This content will be covered in lecture.
The SA node, without nervous or endocrine control, would initiate a heart impulse approximately 80–100 times per minute. Autonomic control over heart rate is initiated in cardiovascular centers of the medulla oblongata of the midbrain and travels through sympathetic and parasympathetic pathways to get to the heart.
Sympathetic fibers originate from the T1-T5 levels and travel to the heart via the postganglionic sympathetic pathway. Parasympathetic fibers travel through the vagus nerve (cranial nerve X). Both sympathetic and parasympathetic stimulations flow through a complex network of nerve fibers known as the cardiac plexus near the base of the heart.
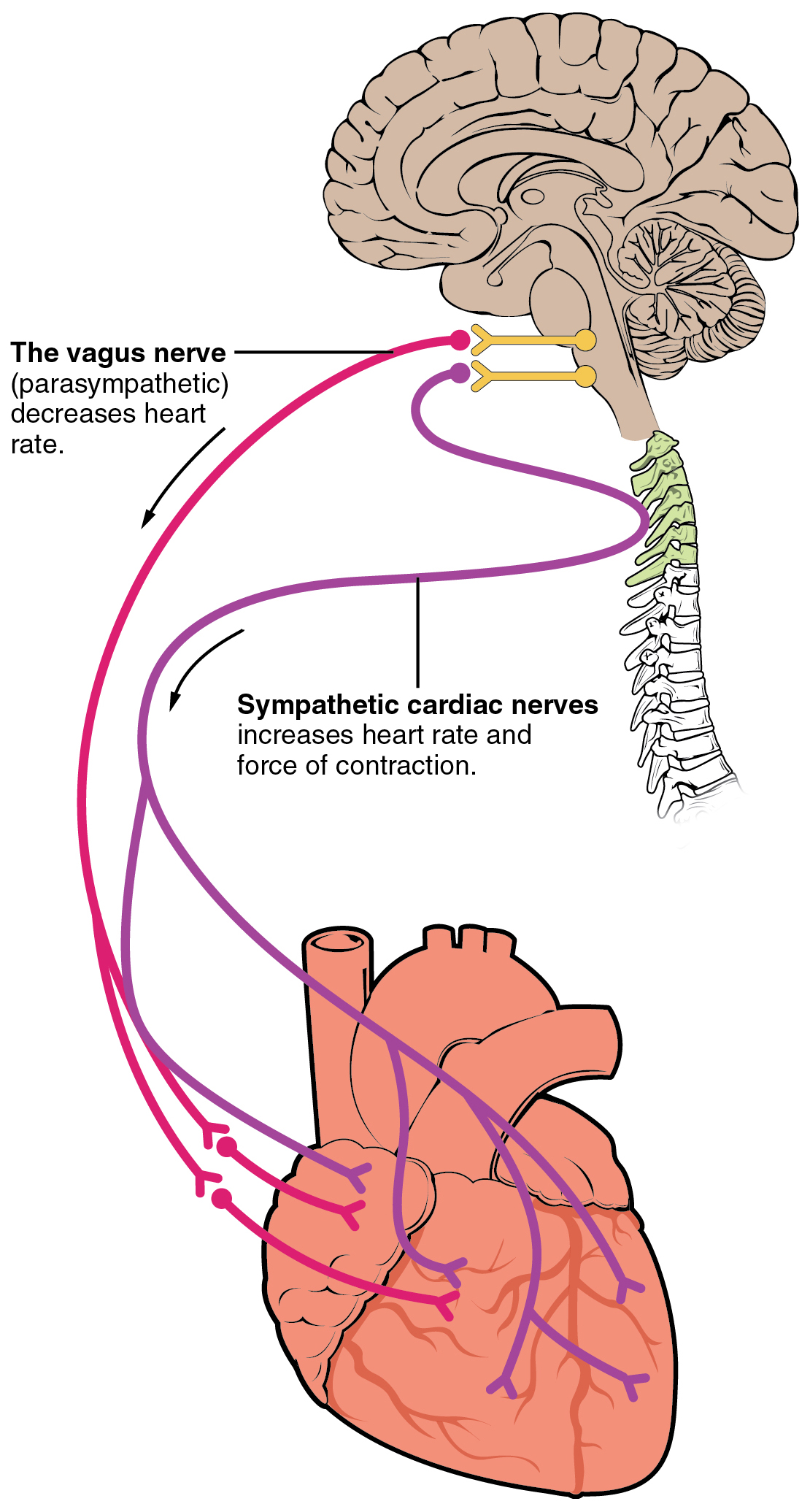
The two divisions have opposing functions:
- Sympathetic division
- Fibers travel to the SA and AV node and cause heart rate to increase. This would occur with fear or with exercise, for example.
- Other fibers travel to the walls of the ventricles, causing an increase in the strength of contraction of the heart muscle.
- Parasympathetic division
- Fibers travel to the SA and AV node and cause the heart rate to decrease. Since resting heart rates are typically less than the 80-100 beats per minute set by the SA node, it is clear that parasympathetic stimulation normally slows heart rate at rest.
- As you can see in the image at the right, the parasympathetic fibers do not travel to the ventricles like the sympathetic fibers do. As a result, they do not influence the strength of contraction. However, strength of contraction still slows at rest. Imagine driving down a road at 30mph. You don’t have to press the brake to slow down. You can slow down by simply taking your foot off of the gas. Similarly, strength of contraction of the heart decreases simply due to a lack of sympathetic innervation at rest.
Great Vessels
This content will be covered in lecture.
Great Vessels in Pulmonary Circulation
The single vessel exiting the right ventricle is the pulmonary trunk. As the pulmonary trunk reaches the superior surface of the heart, it curves posteriorly and rapidly bifurcates (divides) into two branches, a left and a right pulmonary artery. The pulmonary arteries in turn branch many times within the lung. Four pulmonary veins, two on the left and two on the right, return blood to the left atrium.
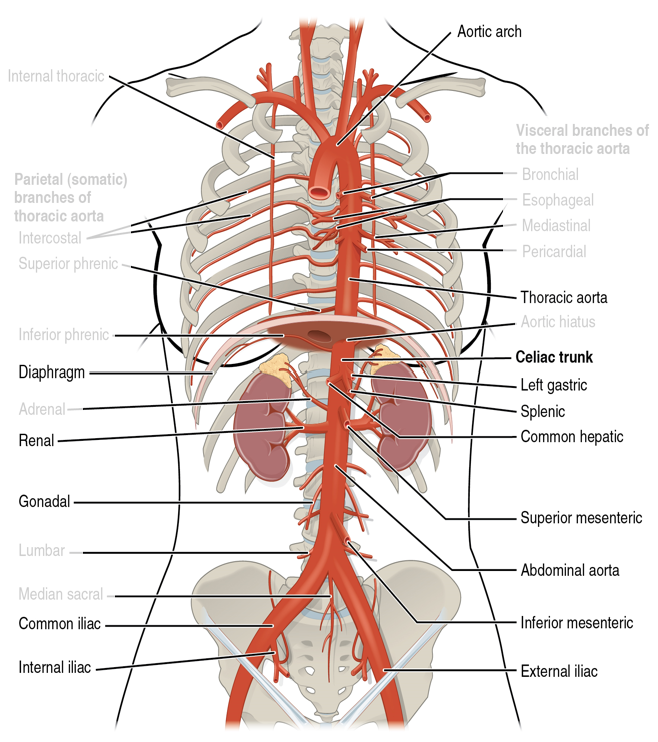
Systemic Circulation: Great Vessels and Major Branches of the Aorta
The aorta is the largest artery in the body. It arises from the left ventricle. After exiting the heart, the ascending aorta moves in a superior direction for approximately 5 cm. Then it reverses direction, forming an arc to the left, called the aortic arch. The aortic arch runs inferiorly a short distance and then becomes the descending aorta. It travels just anterior and to the left of the to the vertebral bodies and passes through an opening in the diaphragm. Superior to the diaphragm, it is called the thoracic aorta, and inferior to the diaphragm, it is called the abdominal aorta. The abdominal aorta terminates when it bifurcates into the two common iliac arteries at the level of the fourth lumbar vertebra. The common iliac arteries split into external and internal iliac arteries and provide blood to the pelvic region and ultimately to the lower limbs.
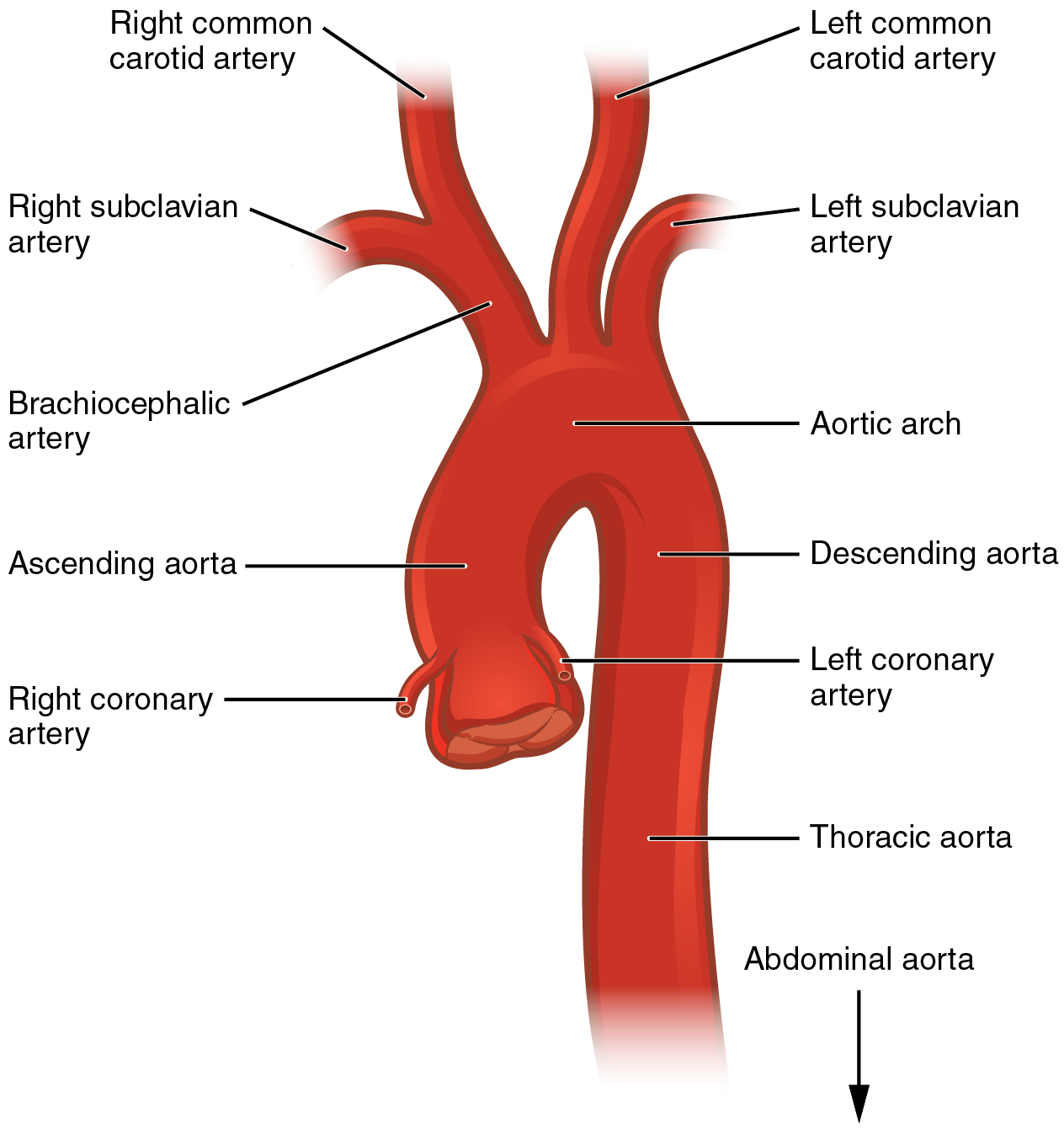
- Ascending aorta
- The right and left coronary arteries are the only branches off the ascending aorta. They travel to supply the walls of the heart with blood.
- Aortic arch: There are three branches off of the aortic arch that result in two pairs of arteries. The arteries to the left branch directly off of the aorta, because the arch of the aorta already travels towards the left of midline. The branches to the right begin as a common trunk to travel to the right of midline before branching into two arteries.
- Brachiocephalic trunk: the first branch off of the aortic arch. It travels towards the right across the midline. It then branches into two arteries that go on to supply the head and upper extremity (brachio- = arm, cepalic = head). There is no corresponding trunk on the left.
- Right common carotid artery: ascends to supply the right side of the head, neck, and brain.
- Right subclavian artery: travels laterally deep to the clavicle to supply the right upper extremity.
- Left common carotid artery: the middle branch off of the aortic arch that ascends to supply the left side of the head, neck, and brain.
- Left subclavian artery: the last branch off of the aortic arch that travels laterally deep to the clavicle to supply the left upper extremity.
- Brachiocephalic trunk: the first branch off of the aortic arch. It travels towards the right across the midline. It then branches into two arteries that go on to supply the head and upper extremity (brachio- = arm, cepalic = head). There is no corresponding trunk on the left.
- Descending aorta
- Thoracic aorta: There are branches off of the thoracic aorta, including the intercostal arteries. We won’t talk about any of these branches here.
- Abdominal aorta, from superior to inferior:
- Celiac trunk: single central, short trunk that branches from the abdominal aorta just inferior to the diaphragm. It branches into three arteries that supply the foregut organs and spleen. We will discuss those branches in a later module.
-
Superior mesenteric artery: single midline artery that arises just inferior to the celiac trunk and branches into several major vessels that supply blood to the midgut organs.
-
Renal arteries: paired right and left arteries that branch just inferior to the superior mesenteric artery and supply the kidneys.
-
Gonadal arteries: paired right and left arteries that branch just inferior to the renal arteries to supply blood to the gonads, or reproductive organs. In the male sex it is referred to as the testicular artery, and in the female sex it is referred to as the ovarian artery.
-
Inferior mesenteric artery: single midline artery that arises a few cm superior to the branching of the abdominal aorta into the common iliac arteries, and it supplies blood to the hindgut organs.