Module 1: Tissues I – Epithelial and Connective
Learning Objectives:
By the end of this class, students will be able to:
- Define the characteristics and features of epithelial tissues.
- Describe the features and functions of each category of epithelial tissues.
- Analyze how the structure of the different types of epithelial tissue governs the function of that tissue and its potential location in the body.
- Explain how the characteristics of epithelial tissue can contribute to pathology.
- Analyze how the structure of the different types of connective tissue governs the function of that tissue and its potential location in the body.
- Describe the characteristics of connective tissue and compare different types of connective tissue in the body
Terms to Know
|
Epithelial Tissue
|
Connective Tissue
Other Terms
*Covered only in lecture, not in this text
|
The Building BLocks
*This content will be reviewed and built upon in lecture.
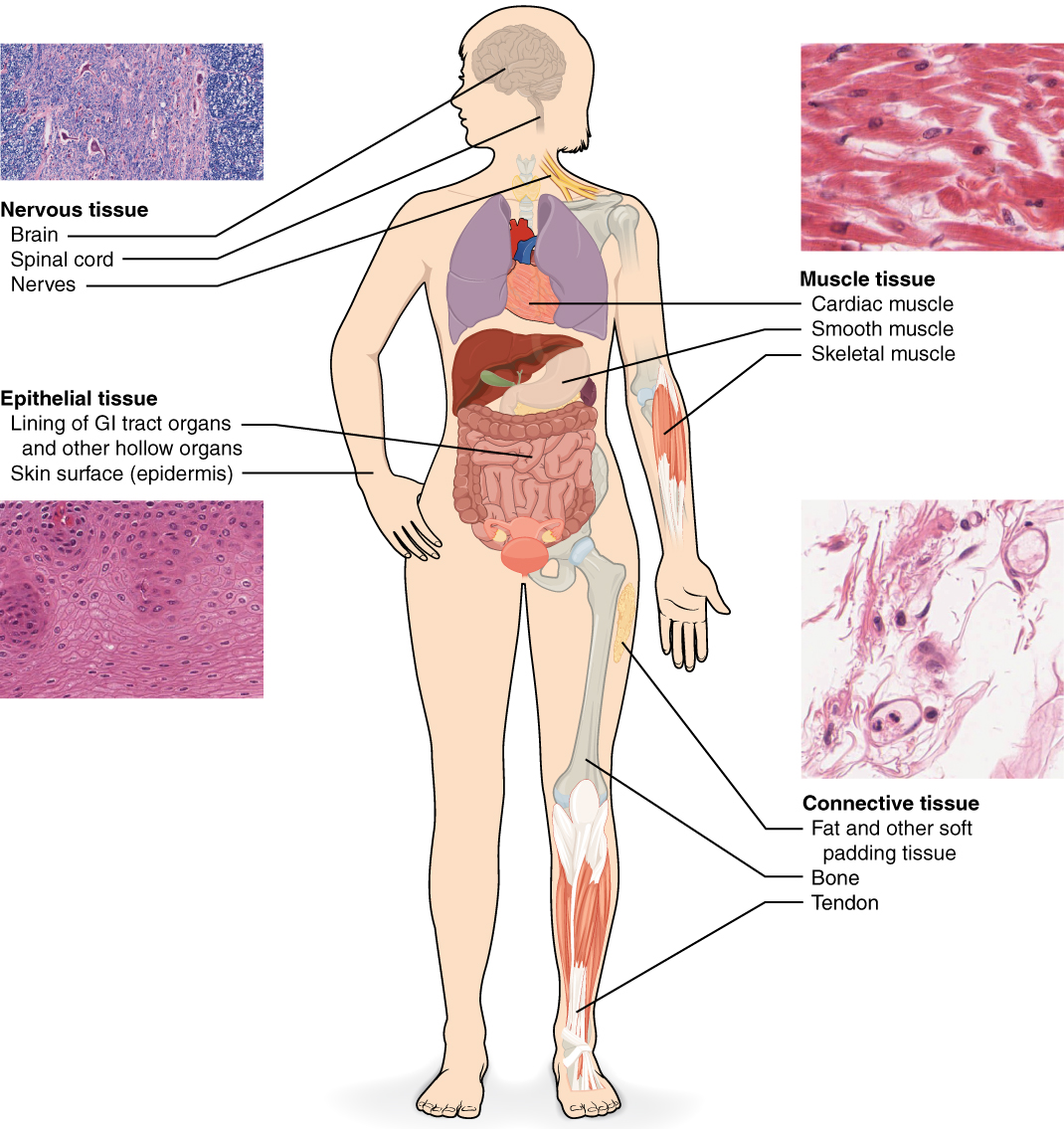
Before you begin to study the different structures and functions of the human body, it is helpful to consider its basic architecture; that is, how its smallest parts are assembled into larger structures ((Figure)). Though this organization begins at the atomic and chemical levels, in this course we will only discuss structures as small as the cellular level, and only in the context of the cells that make up specific tissues. You will learn more about the cellular, molecular, and chemical levels of organization in other courses.
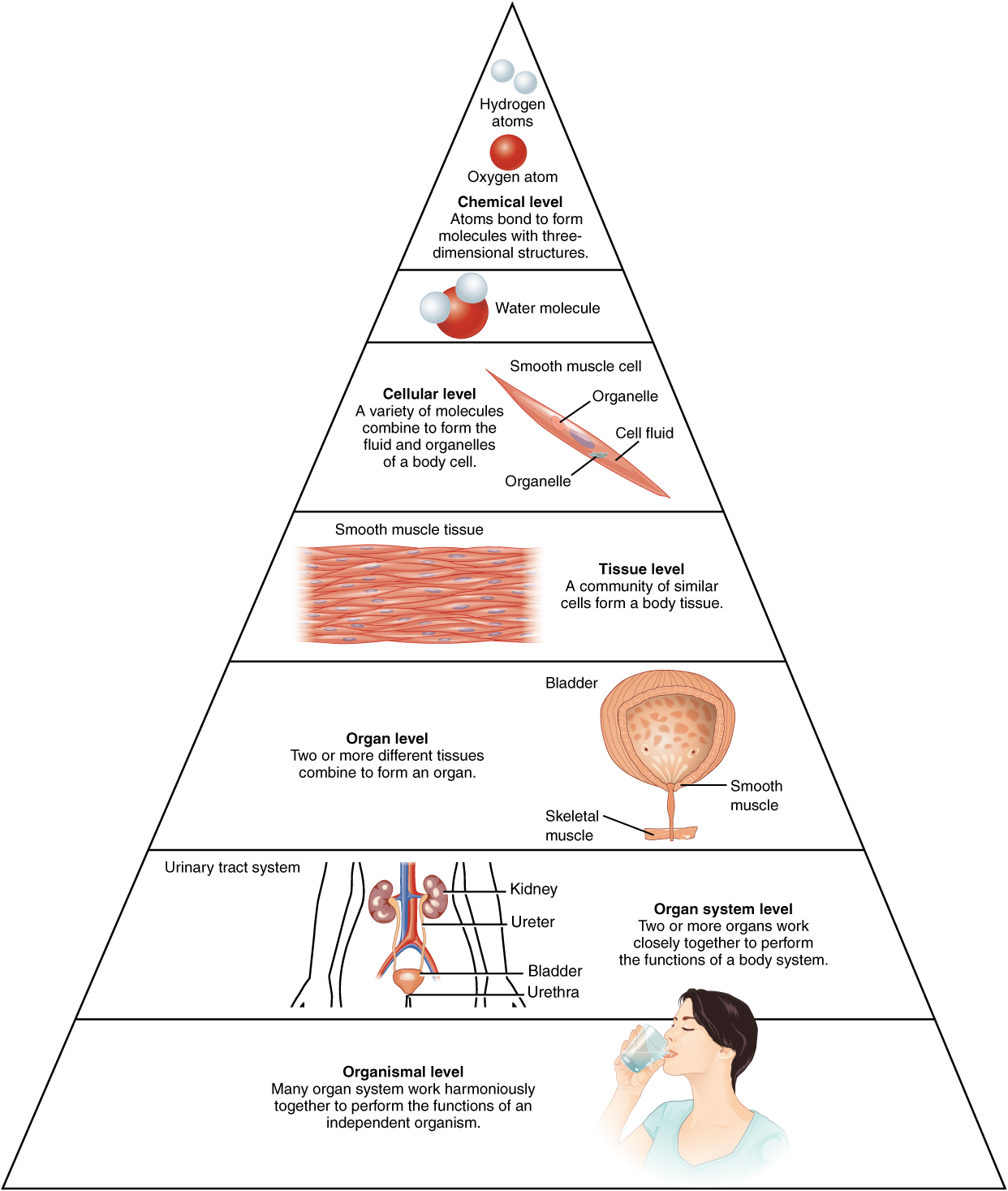
- A cell is the smallest independently functioning unit of a living organism.
- Tissues are composed of many cells that work together to perform a specific function.
- An organ is an anatomically distinct structure of the body composed of two or more tissue types. Each organ performs one or more specific physiological functions.
- An organ system is a group of organs that work together to perform major functions or meet physiological needs of the body.
There are four categories of tissues: epithelial, connective, muscle, and nervous. Epithelial tissue, also referred to as epithelium, refers to the sheets of cells that line all surfaces of the body. Connective tissue binds together, protects, and supports structures of the body. We will cover epithelial tissue and connective tissue in this module. Muscle tissue and nervous tissue will be covered in the next module. Muscle tissue contracts to cause movement, while nervous tissue sends electrical signals to allow communication throughout the body.
Epithelial Tissue
*Some of this content will be reviewed or built-upon in lecture, while some of the epithelial tissue content will be covered in the assignment and interactive activity as self-study material.
Epithelial tissues line all surfaces of the body. This includes the surfaces exposed to the outside world, the surface of organs, and the openings within hollow organs. Epithelium also forms much of the glandular tissue of the body.
Functions
Epithelial tissues have several functions. You will learn about the different functions of specific types of epithelium later in this module. However, you should know these general functions of epithelial tissue.
- Protection: Epithelial tissues provide the body’s first line of protection from physical, chemical, and biological wear and tear.
- Selective permeability: The cells of an epithelium act as gatekeepers of the body controlling permeability and allowing selective transfer of materials across a physical barrier. All substances that enter the body must cross an epithelium. Some epithelia often include structural features that allow the selective transport of molecules and ions across their cell membranes.
- Diffusion: selective, simple transport of substances through a thin layer of tissue
- Absorption (transcellular transport): absorption of substances through the cell, where it is processed to some degree before being released into the blood and/or underlying tissue. This is called transcellular transport because it is going through the cell.
- Secretion: Many epithelial cells are capable of producing and secreting specific chemical compounds onto their apical surfaces.
- Sensation: Specialized epithelia can detect light, taste, sound, smell, and hearing.
- Surface parallel transport: Transport of substances across the free surface of the epithelium.
Characteristics & Features
All epithelia share some important structural and functional features:
- This tissue is highly cellular, with little or no extracellular material present between cells.
- Epithelial tissues are avascular, meaning they do not contain blood vessels. Instead, they receive nutrients by diffusion or absorption from the underlying tissues or occasionally from substances on the surface.
- Many epithelial tissues are capable of regeneration, or rapidly replacing damaged and dead cells. Sloughing off of damaged or dead cells is a characteristic of surface epithelium and allows our airways and digestive tracts to rapidly replace damaged cells with new cells.
- The epithelial cells exhibit polarity, with differences in structure and function between the exposed or apical surface of the cell, the free surface away from underlying tissue, and the basal surface attached to the underlying tissue.
The basement membrane sits just below the basal surface of epithelial cells and anchors the cells to the underlying tissue. It is formed of two layers: the basal lamina, which attaches to the basal aspect of the cells, and the reticular lamina, which is attached to the underlying connective tissue.
Apical Features
Two microscopic extensions can be found on the apical surface of some cells.
- Cilia: extensions from the apical surface of the cell that beat in unison to move fluids as well as trapped particles across the surface of the epithelium (surface parallel transport).
- Microvilli: extensions that serve to increase the surface area of the apical aspect of the cell for absorption. More surface area means more space for substances to contact the apical surface and be absorbed into the cell.
Intercellular Junctions
Epithelial cells are closely connected and are not separated by intracellular material. These cells are held together or interact with each other via junctions, or connections between the cells. Three of these junctions hold the cells together, while one allows for cell-to-cell communication.
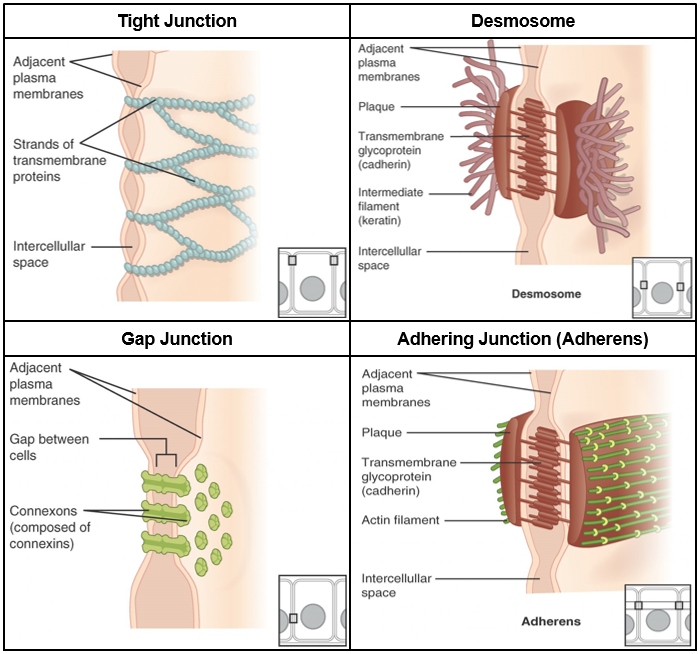
- Tight junction: Holds cells together so there is no extracellular space between them. Tight junctions prevent substances from moving between the cells, instead forcing them to go through the cells. This enables the epithelia to act as a selective barrier.
- Adhering junction (adherens): Acts like a belt holding the epithelial cells together for support and stability of the tissue.
- Desmosome: Holds cells together like a push button on a jacket to provide support and stability of the tissue.
- Gap junction: Forms an intercellular passageway between the membranes of adjacent cells to facilitate the movement of small molecules and ions between the cytoplasm of adjacent cells. These junctions allow electrical and metabolic coupling of adjacent cells, which coordinates function in large groups of cells.
Classification of Epithelial Tissues
*This information will not be reviewed in lecture. Be sure to understand what is written here in the text and the table. Your assignment and the interactive activity on the Canvas page will help you review this material.
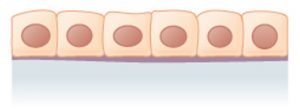
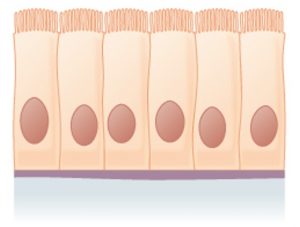
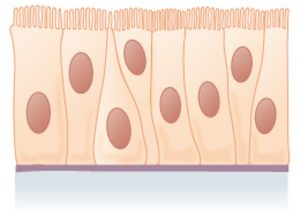
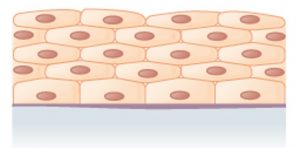
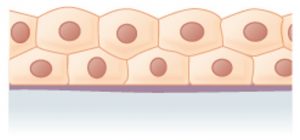
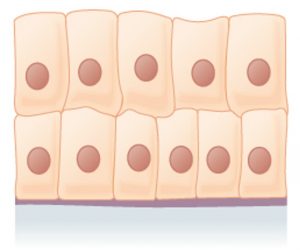
Epithelial tissues are classified according to the shape of the cells and number of the cell layers formed ((Figure)).
- Shape:
- Squamous: Flattened and thin
- Cuboidal: Like a cube or box, wide as it is tall
- Columnar: Like a rectangular cube, taller than it is wide.
- Number of cell layers
- Simple: A single layer of cells, with every cell resting on the basal lamina of the basement membrane
- Stratified: More than one layer of cells, with only the basal layer resting on the basal lamina of the basement membrane. This can be just a few layers or dozens of layers depending on the location.
- Pseudostratified: Only one layer of cells, but the height of the cells vary, giving the appearance of more than one layer (pseudo- = false). Only some of the cells have an apical surface that reaches the free surface of the epithelium.
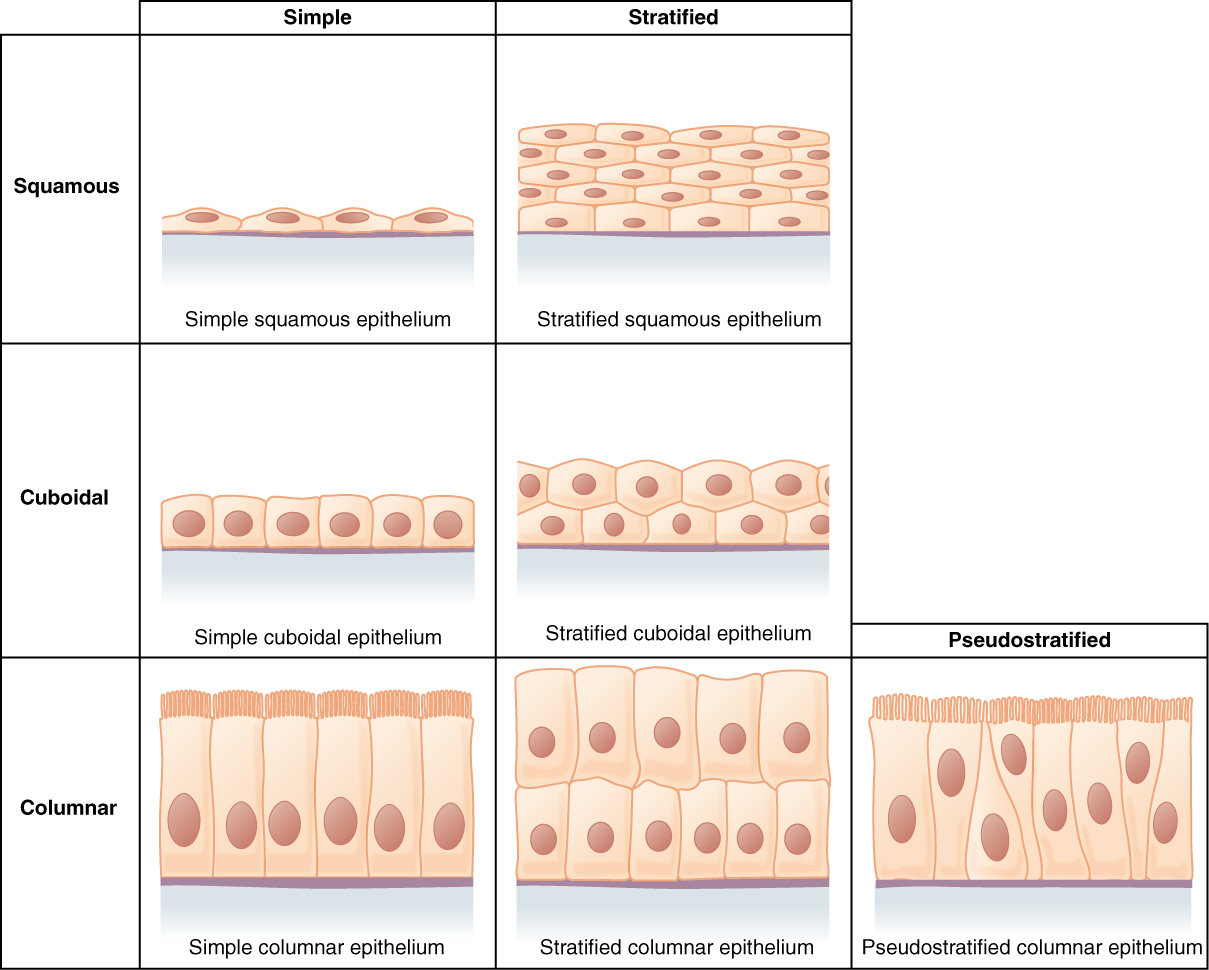
Thinner epithelium allows for faster and easier transport of substances across the surface, so it functions to allow transcellular (through the cell) transport via simple diffusion. The thicker the epithelium is (cuboidal to columnar), the more space there is for intracellular machinery needed to produce substances for secretion or process substances that have been absorbed before releasing it into the underlying tissue. Stratified epithelium has multiple layers, meaning there are more layers to lose before damaging the underlying tissue. Therefore, stratified epithelium always has a protective function.
There are several different kinds of epithelium based on different combinations of the shape and number of layers of cells. Note that the name of stratified epithelium is determined by the shape of the cell at the most superficial layer, furthest from the underlying connective tissue. You are responsible for knowing the information in the following table:
| Type of Epithelium | Structure | Function | Location |
|
Simple Squamous
|
A single layer of flat, thin cells. | Allows materials to pass through quickly via simple diffusion or filtration. | Located in places where we need substances to pass quickly and relatively easily through the epithelium. Example: The alveoli, or air sacs, in our lungs. |
|
Simple Cuboidal
|
A single layer of cuboidal-shaped cells, as wide as they are tall. May have microvilli on the surface in some locations. | Secretion & absorption | The cuboidal shape allows for some space for intracellular processing of absorbed substances or production of substances to be secreted without being overly-thick. It is located in regions that benefit from this structure-function relationship. Example: Certain glands, kidney tubules |
|
Simple Columnar
|
A single layer of cells that are taller than they are wide. These epithelial cells sometimes have microvilli. | Absorption & secretion | The columnar shape allows ample space for intracellular processing of absorbed substances or production of substances to be secreted. It is located in areas that benefit from this structure-function relationship. Example: Digestive tract |
|
Pseudostratified Columnar
|
A single layer of cells of different shapes and sizes, with only some of the cells reaching the free surface of the tissue. This gives it a stratified appearance despite actually being a single layer of cells. It contains cilia on the apical surface. | Surface parallel transport (moving substances across the free surface of the epithelium). Also secretion of mucous | The cilia function to move substances along the surface of the epithelium primarily in locations without smooth muscle to move the substances through a tract. Example: Trachea |
|
Stratified Squamous
|
Multiple layers of flat, thin cells. Cells at the basal surface may be thicker, more cuboidal in shape, but they flatten as they reach the apical surface. | Protection | More layers means more layers to lose before damage reaches the underlying tissue. Therefore, it is found in places exposed to physical and chemical wear and tear. Example: Skin (keratinized epithelium, keratin is found in the cells in the superficial layers), esophagus (non-keratinized) |
|
Stratified Cuboidal
|
Multiple layers of cells with the most superficial cells being cuboidal in shape. ***This epithelium is rare, and we will not ask you about it on an exam. | Protection | Example: Found in some glands |
|
Stratified Columnar
|
Multiple layers of cells with the most superficial cells being columnar in shape. ***This epithelium is rare, and we will not as you about it on an exam. | Protection & secretion | Example: Male urethra, some glands |
|
Transitional
|
Special epithelium with layers of epithelial cells that stretch when the organ is distended. | Allows urinary organs to expand and stretch, such as when the bladder fills with urine. | Example: Bladder, ureters, urethra |
Glandular Epithelium
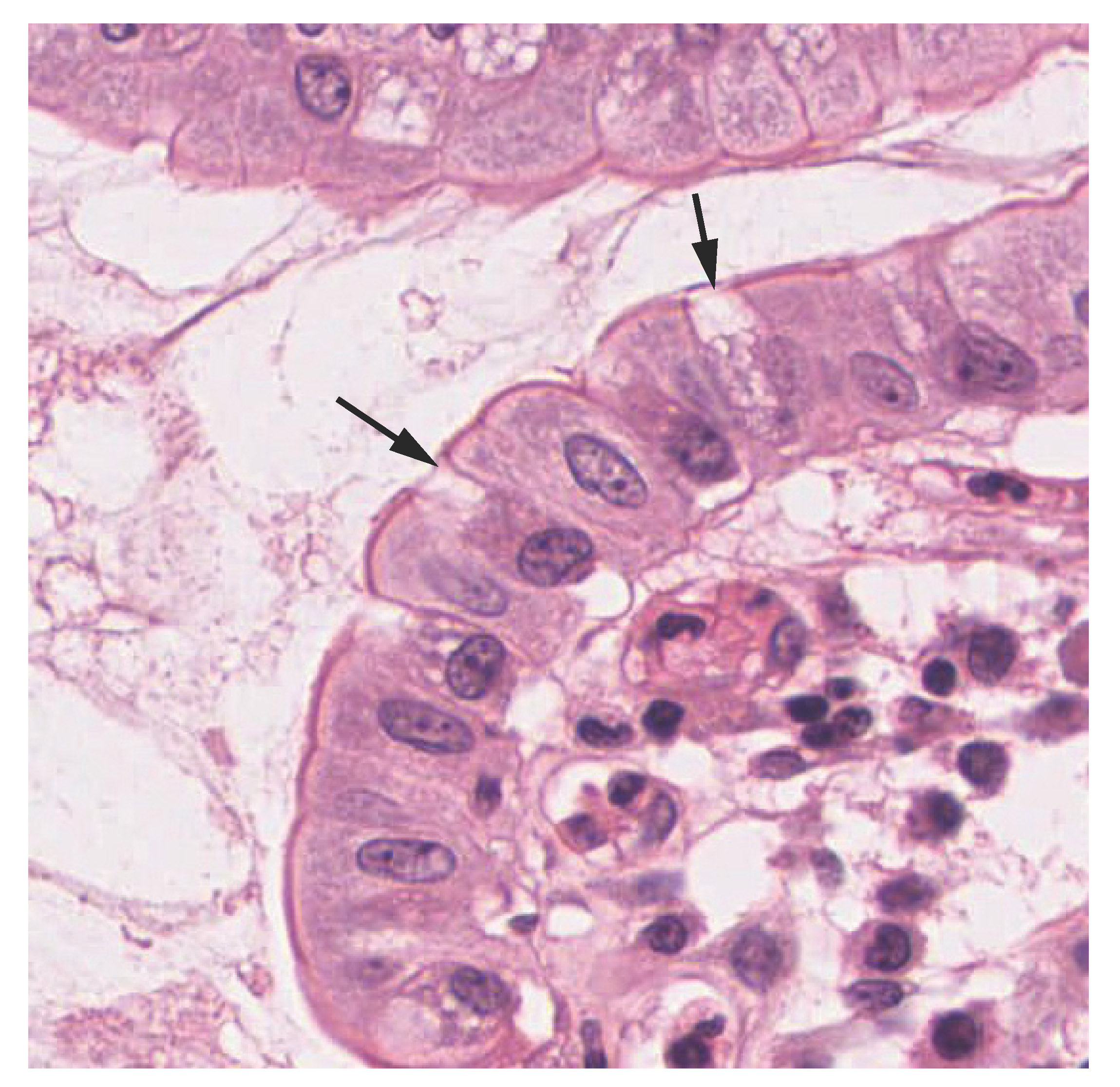
A gland is a structure made up of one or more cells modified to synthesize and secrete chemical substances. Most glands consist of groups of epithelial cells, though some cells themselves are considered glands. A goblet cell is a unicellular exocrine “gland” interspersed between the columnar or pseudostratified columnar epithelial cells of mucous membranes ((Figure)). Goblet cells secrete mucin, which becomes mucous when mixed with water.
A gland can be classified as an endocrine gland, a ductless gland that releases hormones directly into surrounding tissues and bloodstream (endo- = “inside”), or an exocrine gland whose secretions leave through a duct that opens directly, or indirectly, to a surface (e.g. skin, digestive tract, respiratory tract; exo- = “outside”). We will discuss these types of glands more in lecture.
Connective Tissue
Unlike epithelial tissue, which is composed of cells closely packed with little or no extracellular space in between, connective tissue cells are dispersed among an extracellular matrix (substances in the space around the cells) of ground substance and protein fibers produced by the cells of that connective tissue. The ground substance is usually a fluid, but it can also be mineralized and solid, as in bones.
Connective tissues come in a vast variety of forms, yet they typically have in common three characteristic components: cells, large amounts of ground substance, and protein fibers. The amount and structure of each component correlates with the function of the tissue.
Functions of Connective Tissues
- Supporting and connective tissues: Connective tissues support and connect other tissues; from the connective tissue sheath that surrounds muscle cells, to the tendons that attach muscles to bones, and to the skeleton that supports the positions of the body.
- Protection: Connective tissues provide cushioning as well as bony protection of organs.
- Defense: Specialized cells in connective tissue defend the body from microorganisms that enter the body.
- Transport: Transport of fluid, nutrients, waste, and chemical messengers is ensured by specialized fluid connective tissues, such as blood and lymph.
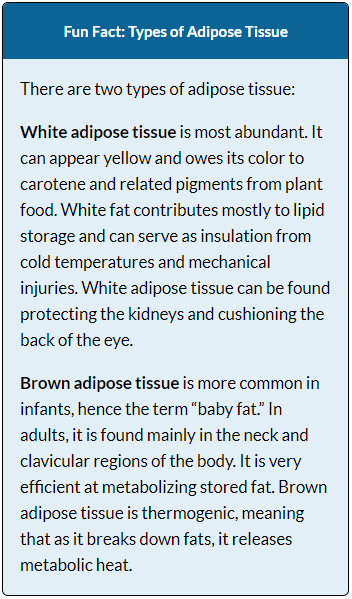
- Energy storage: Adipose cells store surplus energy in the form of fat and contribute to the thermal insulation of the body.
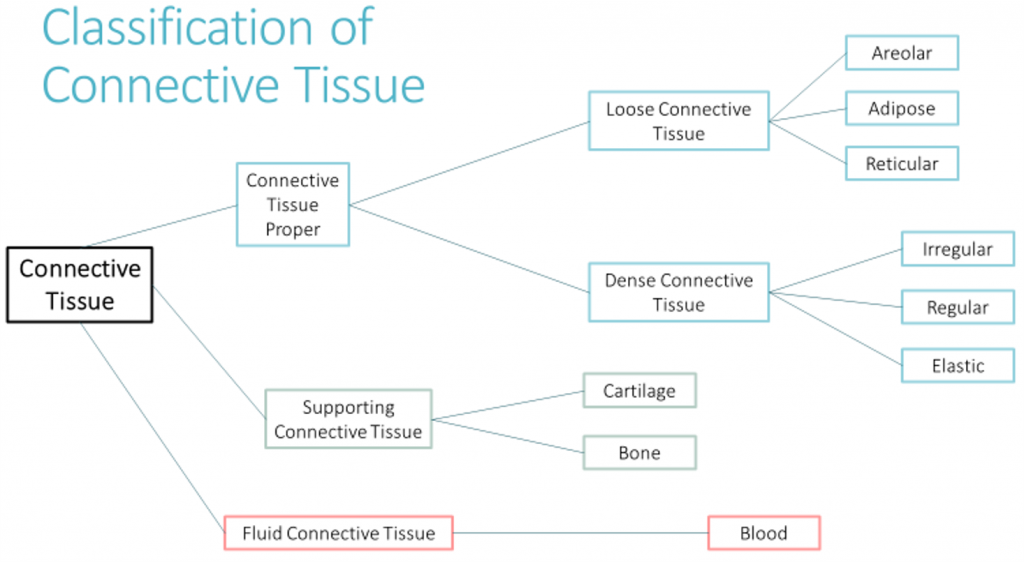
Classification of Connective Tissues
The three broad categories of connective tissue are classified according to the characteristics of their ground substance and the types of fibers found within the matrix. We will discuss connective tissue proper in this module. You will learn about supportive connective tissues and fluid connective tissues in upcoming modules.
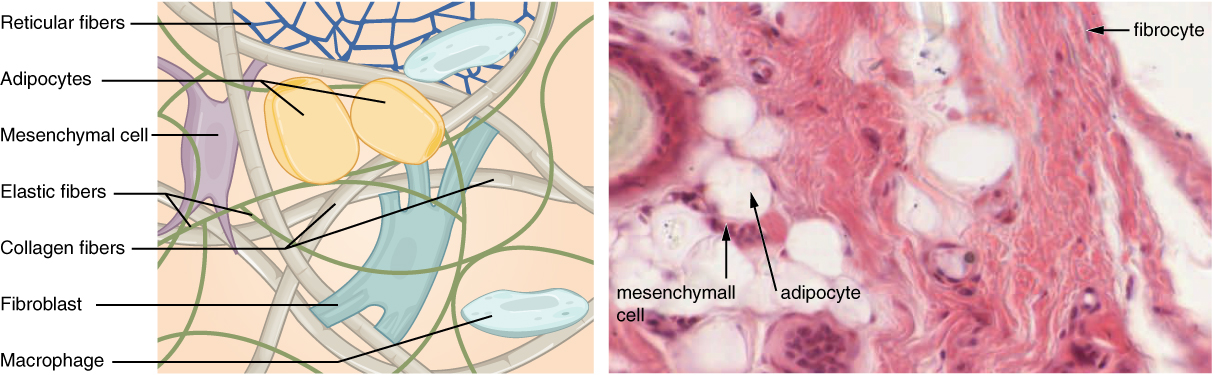
Connective Tissue Proper
Connective tissue proper is the largest category of connective tissue. The primary cell type of connective tissue proper is the fibroblast, which secretes the ground substance and protein fibers in the extracellular matrix. Three main types of fibers are secreted by fibroblasts: collagen fibers, elastic fibers, and reticular fibers. All of these fiber types are embedded in ground substance, which is secreted by fibroblasts. Some of these fibers can be found in other categories of connective tissue as well.
- Collagen fibers: Collagen fibers, while flexible, have great tensile strength, resist stretching, and give ligaments and tendons their characteristic resilience and strength. These fibers hold connective tissues together, even during the movement of the body.
- Elastic fibers: These fibers contain the protein elastin along. The main property of elastin is that after being stretched or compressed, it will return to its original shape.
- Reticular fibers: Reticular fibers are found throughout the body, but are most abundant in the reticular tissue of soft organs, such as liver and spleen, where they anchor and provide structural support to the organ while allowing space for blood and cells to move through the structure.
Connective tissue proper can be further subdivided into loose connective tissue and dense connective tissue.
Loose Connective Tissue
Loose connective tissue is found between many organs where it acts both to absorb shock and bind tissues together.
- Areolar connective tissue: Areolar tissue shows little specialization. It contains all the cell types and fibers distributed in a random, web-like fashion. It fills the spaces between muscle fibers, surrounds blood and lymph vessels, and supports organs in the abdominal cavity. Areolar tissue underlies most epithelia, including between our skin and our muscles or bone.
- Adipose tissue: This tissue consists mostly of fat storage cells, called adipocytes, with little extracellular matrix ((Figure)). A large number of capillaries allow rapid storage and mobilization of lipid (“fat”) molecules. The number and type of adipocytes depends on the tissue and location, and vary among individuals in the population.
- Reticular tissue: This tissue is a mesh-like, supportive framework for soft organs such as lymphatic tissue, the spleen, and the liver ((Figure)). It functions like a scaffolding that gives shape to these organs while also allowing space for blood and cells to pass through it. Reticular cells produce the reticular fibers that form the network onto which other cells attach.
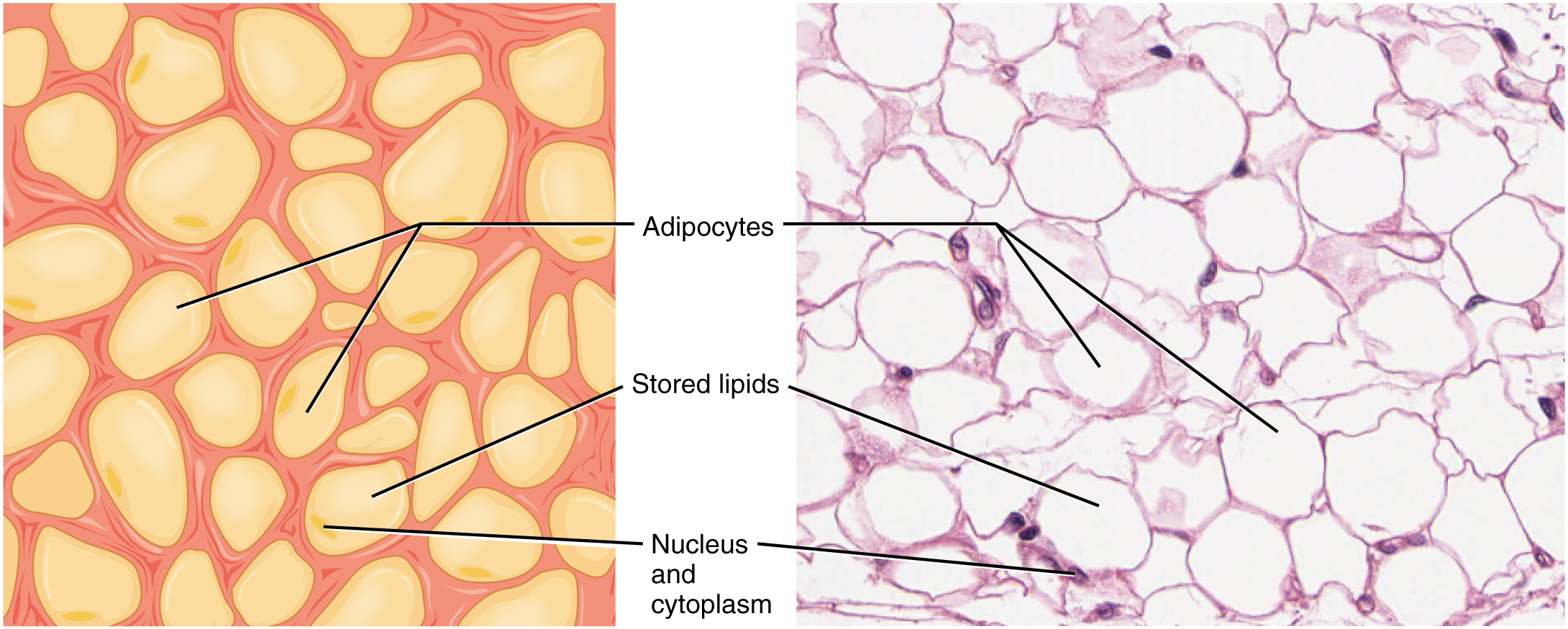
 Adipose & Reticular Tissue: The above image shows adipose tissue. Lipid molecules do not take up the stain used in preparation of the light micrograph, making the areas of stored lipids appear as an empty space in these images. (LM × 800). The bottom images show reticular tissue, made up of a network of dark-staining reticular fibers. (LM × 1600). (Micrographs provided by the Regents of University of Michigan Medical School © 2012)
Adipose & Reticular Tissue: The above image shows adipose tissue. Lipid molecules do not take up the stain used in preparation of the light micrograph, making the areas of stored lipids appear as an empty space in these images. (LM × 800). The bottom images show reticular tissue, made up of a network of dark-staining reticular fibers. (LM × 1600). (Micrographs provided by the Regents of University of Michigan Medical School © 2012)
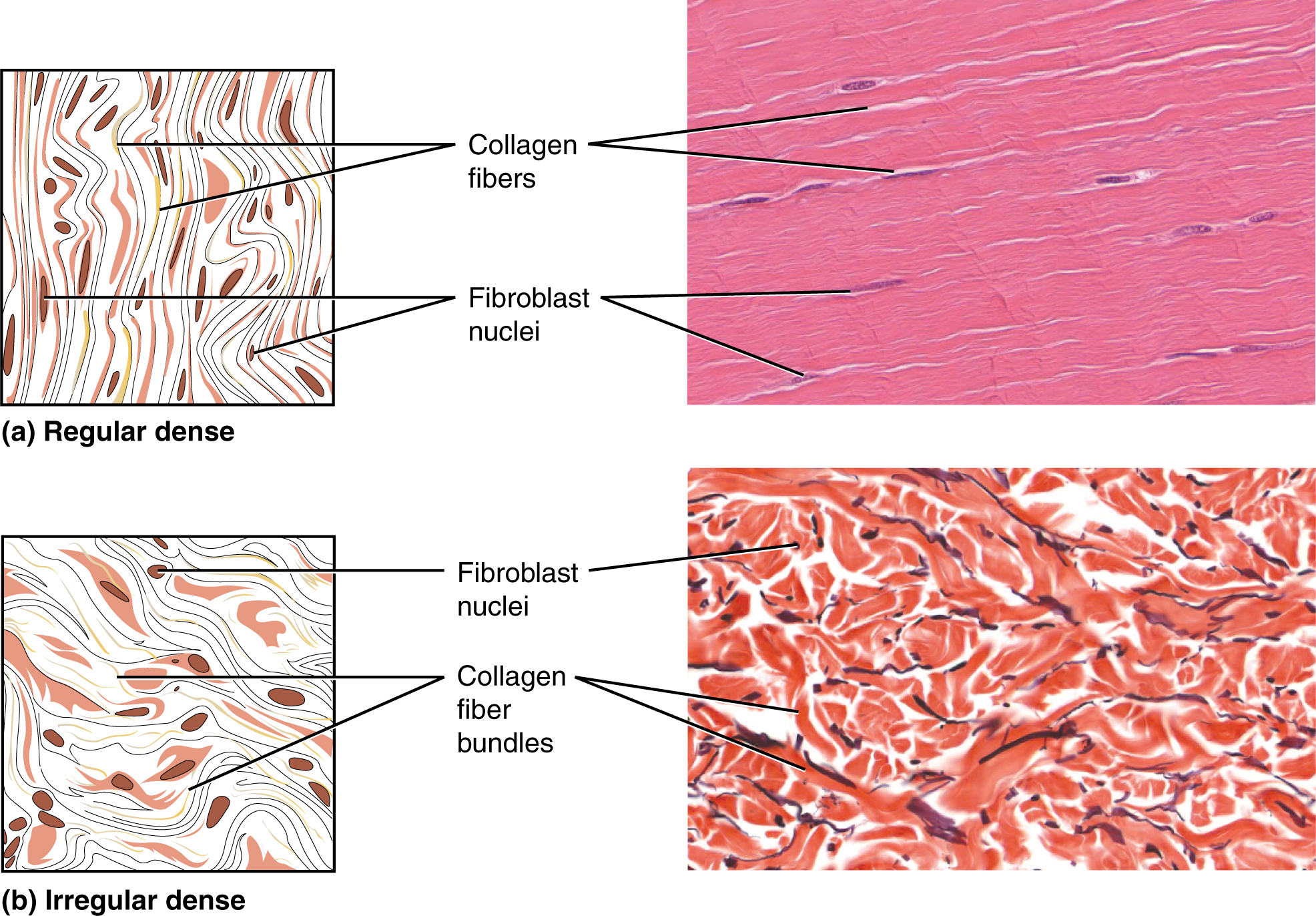
Dense Connective Tissue
Dense connective tissue contains more collagen fibers than does loose connective tissue. As a consequence, it displays greater resistance to stretching. There are three major categories of dense connective tissue:
- Dense regular connective tissue: In dense regular connective tissue, fibers are parallel to each other, enhancing tensile strength and resistance to stretching in the direction of the fiber orientations (and only that direction). For example, tendons are made of dense regular connective tissue.
- Dense irregular connective tissue: In dense irregular connective tissue, the direction of collagen fibers is random. This arrangement gives the tissue greater strength in all directions and less strength in one particular direction. The dermis of the skin is an example of dense irregular connective tissue rich in collagen fibers.
- Elastic connective tissue: Elastic tissue contains elastin fibers in addition to collagen fibers, which allows the tissue to return to its original length after stretching. This tissue can be found in the ligaments that form the vocal cords and the walls of large blood vessels, for example.