Module 25: Oral Cavity and Taste
Learning Objectives:
By the end of this class, students will be able to:
- Name the muscles of mastication, and explain how each affects mandibular movement.
- Describe the muscles and movements of the tongue.
- Define and describe the structure, location, and innervation pathway of gustatory receptors.
- Explain the anatomy and function of the various structures in the oral cavity, including the tongue, palate, and salivary glands
Terms to Know
|
Oral Cavity General
Salivary Glands
|
Teeth
Gustation
|
The Oral Cavity
The cheeks, tongue, and palate frame the mouth, which is also called the oral cavity (or buccal cavity). At the entrance to the mouth are the lips, or labia (singular = labium). Their outer covering is skin, which transitions to a mucous membrane in the oral vestibule. Lips are very vascular with a thin layer of keratin; hence, they are “red.” The lips cover the orbicularis oris muscle, which regulates what comes in and goes out of the mouth. The labial frenulum is a midline fold of mucous membrane that attaches the inner surface of each lip to the gum. The cheeks make up the oral cavity’s sidewalls. While their outer covering is skin, their inner covering is mucous membrane. This membrane is made up of non-keratinized, stratified squamous epithelium. Between the skin and mucous membranes are connective tissue and buccinator muscles. The next time you eat some food, notice how the buccinator muscles in your cheeks and the orbicularis oris muscle in your lips contract, helping you keep the food from falling out of your mouth. Additionally, notice how these muscles work when you are speaking.
The pocket-like part of the mouth framed on the inside by the gums and teeth and the outside by the cheeks and lips is called the oral vestibule. Moving farther into the mouth, the opening between the oral cavity and throat (oropharynx) is called the fauces (like the kitchen “faucet”). The mouth’s main open area, or oral cavity proper, runs from the gums and teeth to the fauces.
When you are chewing, you do not find it difficult to breathe simultaneously. The next time you have food in your mouth, notice how the arched shape of the roof of your mouth allows you to handle both digestion and respiration at the same time. This arch is called the palate. The anterior region of the palate serves as a wall (or septum) between the oral and nasal cavities, as well as a rigid shelf against which the tongue can push food. It is created by the maxillary and palatine bones of the skull and, given its bony structure, is known as the hard palate. If you run your tongue along the roof of your mouth, you’ll notice that the hard palate ends in the posterior oral cavity, and the tissue becomes fleshier. This part of the palate, known as the soft palate, is composed mainly of skeletal muscle. Therefore, you can subconsciously manipulate the soft palate—for instance, to yawn, swallow, or sing.
Oral Cavity
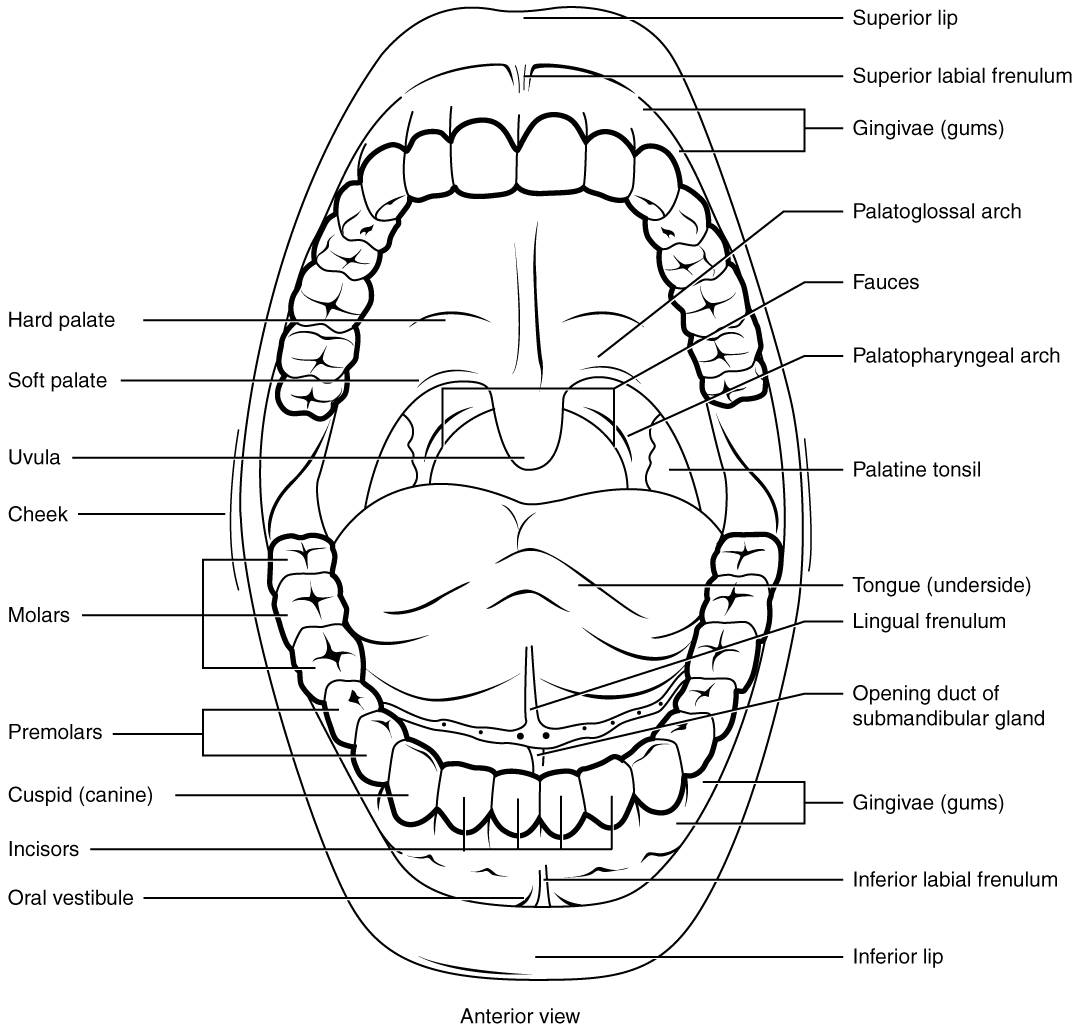
A fleshy bead of tissue called the uvula drops down from the center of the soft palate’s posterior edge. Although some have suggested that the uvula is a vestigial organ, it serves an important purpose. When you swallow, the soft palate and uvula move upward, helping to keep foods and liquid from entering the nasal cavity. Unfortunately, it can also contribute to the sound produced by snoring. Two muscular folds extend downward from the soft palate on either side of the uvula. Toward the front, the palatoglossal arch lies next to the base of the tongue; behind it, the palatopharyngeal arch forms the superior and lateral margins of the fauces. Between these two arches are the palatine tonsils, clusters of lymphoid tissue that protect the pharynx. The lingual tonsils are located at the base of the tongue.
The Tongue
The tongue facilitates ingestion, mechanical digestion, chemical digestion (lingual lipase), sensation (taste, texture, and temperature of food), swallowing, and vocalization. The tongue is attached to the mandible, the styloid processes of the temporal bones, and the hyoid bone. The hyoid is unique in that it only distantly/indirectly articulates with other bones. The tongue is positioned over the floor of the oral cavity. A medial septum extends the entire length of the tongue, dividing it into symmetrical halves.
Beneath its mucous membrane covering, each half of the tongue comprises the same number and type of intrinsic and extrinsic skeletal muscles. The intrinsic muscles (those within the tongue) allow you to change your tongue’s size and shape. The tongue’s extrinsic muscles allow you to move the tongue in space (protract, retract, elevate, and depress). Having such a flexible tongue facilitates both swallowing and speech.
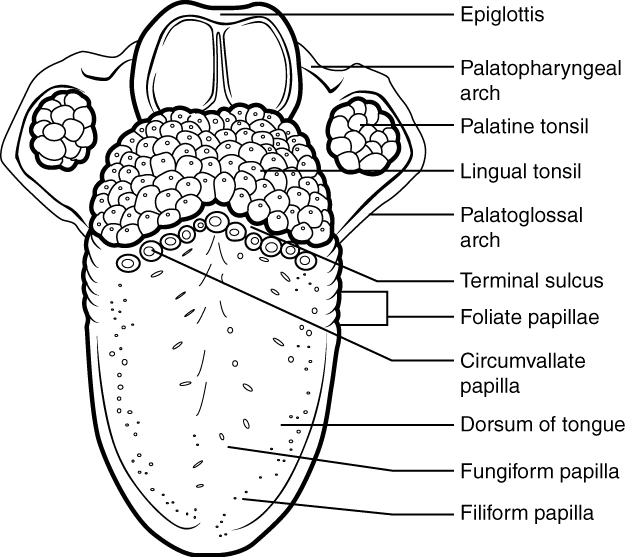
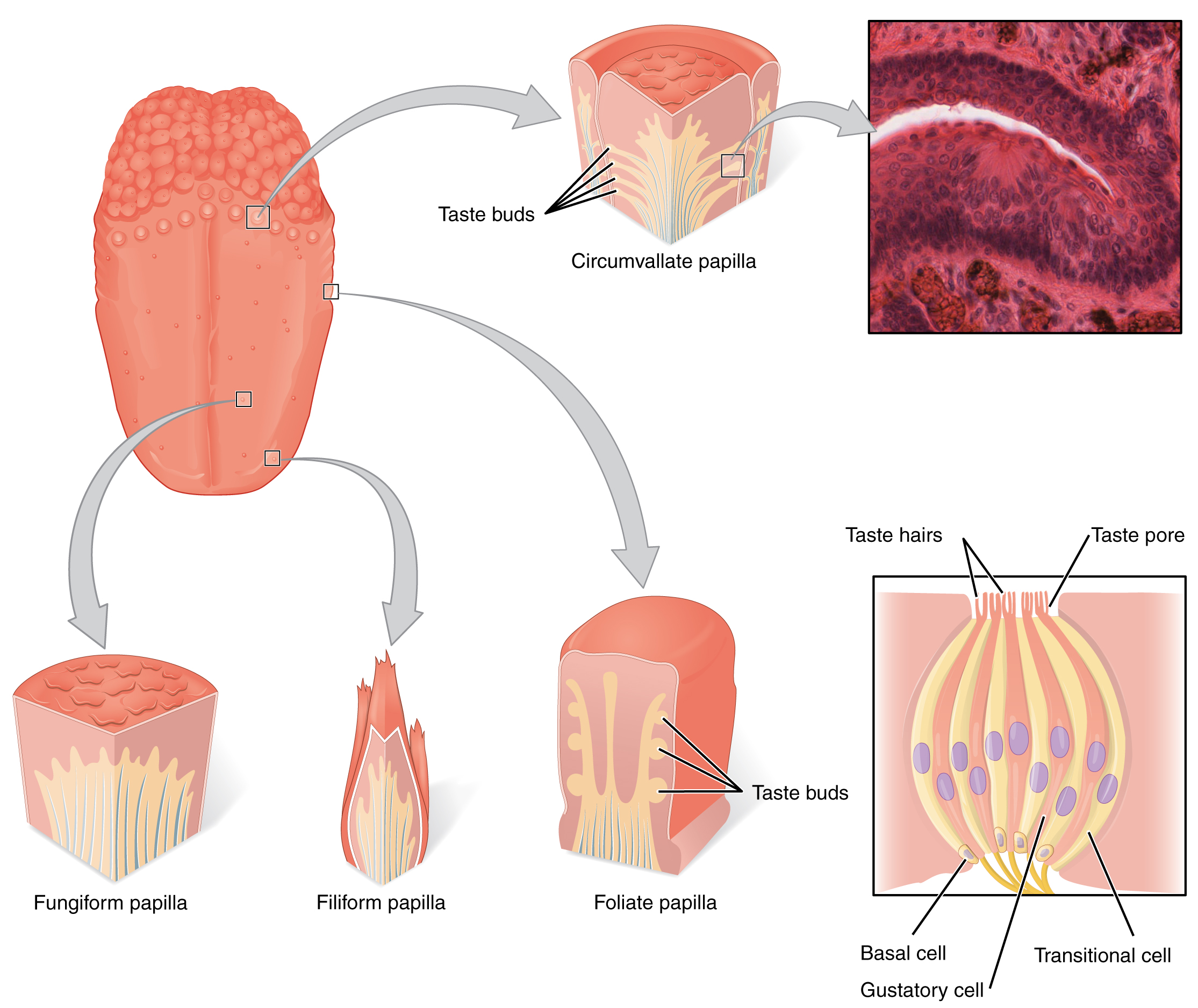
The top and sides of the tongue are studded with papillae, extensions of lamina propria of the mucosa, which are covered in stratified squamous epithelium. Mushroom-shaped fungiform papillae cover a large area of the tongue; they tend to be larger toward the rear of the tongue and smaller on the tip and sides. In contrast, filiform papillae are long and thin. Fungiform papillae contain taste buds, and filiform papillae have touch receptors that help the tongue move food around in the mouth. The filiform papillae create an abrasive surface that performs mechanically, much like a cat’s rough tongue used for grooming. Lingual glands in the tongue’s lamina propria secrete mucus and watery serous fluid that contains the enzyme lingual lipase, which plays a minor role in breaking down triglycerides but does not begin working until it is activated in the stomach. A fold of mucous membrane on the underside of the tongue, the lingual frenulum, tethers the tongue to the floor of the mouth.
Tongue
Muscles That Move the Tongue
Although the tongue is obviously important for tasting food, it is also necessary for mastication, deglutition (swallowing), and speech. Because it is so moveable, the tongue facilitates complex speech patterns and sounds.
Muscles that Move the Tongue
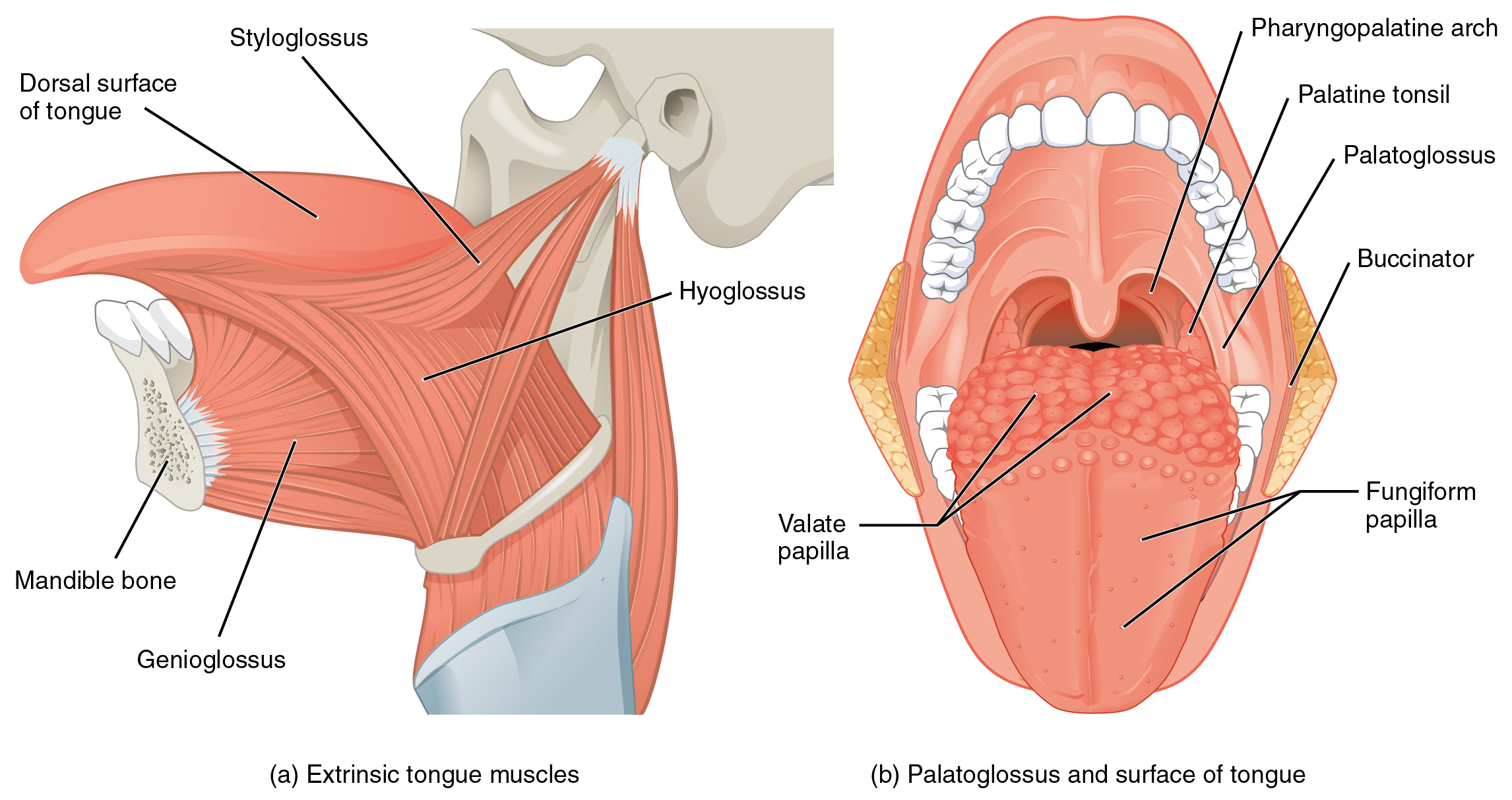
Tongue muscles can be extrinsic or intrinsic. Extrinsic tongue muscles insert into the tongue from outside origins, and the intrinsic tongue muscles insert into the tongue from origins within it. The extrinsic muscles move the whole tongue in different directions, whereas the intrinsic muscles allow the tongue to change its shape (such as curling the tongue in a loop or flattening it).
The extrinsic muscles all include the word root glossus (glossus = “tongue”), and the muscle names are derived from where the muscle originates. These muscles originate outside the tongue and insert into connective tissues within the tongue. The palatoglossus is responsible for elevating the posterior tongue, the hyoglossus pulls it down and back, the styloglossus pulls it up and back, and the genioglossus pulls it forward. Working in concert, these muscles perform three important digestive functions in the mouth: (1) position food for optimal chewing, (2) gather food into a bolus (rounded mass), and (3) position food so it can be swallowed.
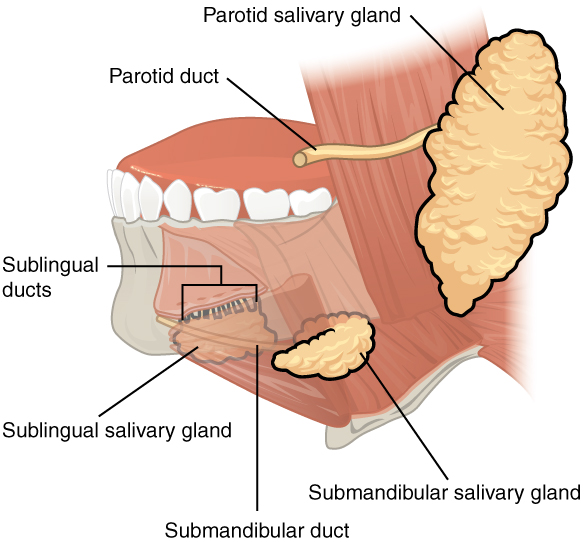
The Salivary Glands
Many small intrinsic salivary glands are housed within the mucous membranes of the mouth and tongue. These minor exocrine glands are constantly secreting saliva directly into the oral cavity or indirectly through ducts, even while you sleep. In fact, an average of 1 to 1.5 liters of saliva is secreted each day. Usually, just enough saliva is present to moisten the mouth and teeth. Secretion increases when you eat because saliva is essential to moisten food and initiate the chemical breakdown of carbohydrates. The labial glands also secrete small amounts of saliva in the lips. Also, the buccal glands in the cheeks, palatal glands in the palate, and lingual glands in the tongue help ensure that all areas of the mouth are supplied with adequate saliva.
The Major Salivary Glands
Outside the oral mucosa are three pairs of major salivary glands, which secrete the majority of saliva into ducts that open into the mouth:
- The submandibular glands, which are on the floor of the mouth, secrete saliva into the mouth through the submandibular ducts. The submandibular glands are innervated by CN VII (facial nerve).
- The sublingual glands, which lie below the tongue, use the lesser sublingual ducts to secrete saliva into the oral cavity. The sublingual glands are innervated by CN VII (facial nerve).
- The parotid glands lie between the skin and the masseter muscle, near the ears. They secrete saliva into the mouth through the parotid duct, which is located near the second upper molar tooth. The parotid glands are innervated by CN IX (glossopharyngeal nerve).
Salivary glands
Saliva Fun Facts – >(you will not be assessed on this content)
Saliva is essentially (98 to 99.5 percent) water. The remaining .5-2 percent is a complex mixture of ions, glycoproteins, enzymes, growth factors, and waste products. Perhaps the most important ingredient in saliva from the perspective of digestion is the enzyme salivary amylase, which initiates the breakdown of carbohydrates. Food does not spend enough time in the mouth to allow all the carbohydrates to break down, but salivary amylase continues acting until it is inactivated by stomach acids. Bicarbonate and phosphate ions function as chemical buffers, maintaining saliva at a pH between 6.35 and 6.85. Salivary mucus helps lubricate food, facilitating movement in the mouth, bolus formation, and swallowing. Saliva contains immunoglobulin A, which prevents microbes from penetrating the epithelium, and lysozyme, making saliva antimicrobial. Saliva also contains epidermal growth factor, which might have given rise to the adage “a mother’s kiss can heal a wound.”
Each of the major salivary glands secretes a unique formulation of saliva according to its cellular makeup. For example, the parotid glands secrete a watery solution that contains salivary amylase. The submandibular glands have cells similar to those of the parotid glands, as well as mucus-secreting cells. Therefore, saliva secreted by the submandibular glands also contains amylase but in a liquid thickened with mucus. The sublingual glands contain mostly mucous cells, and they secrete the thickest saliva with the least amount of salivary amylase.
Mumps – FYI (For Your Information -> you will not be assessed on this content)
In about one-third of men who are past puberty, mumps also causes testicular inflammation, typically affecting only one testis and rarely resulting in sterility. With the increasing use and effectiveness of mumps vaccines, the incidence of mumps has decreased dramatically. According to the U.S. Centers for Disease Control and Prevention (CDC), the number of mumps cases dropped from more than 150,000 in 1968 to fewer than 1700 in 1993 to 11 reported cases in 2011.
Regulation of Salivation
The autonomic nervous system regulates salivation (the secretion of saliva). In the absence of food, parasympathetic stimulation keeps saliva flowing at just the right level for comfort as you speak, swallow, sleep, and generally go about life. Over-salivation can occur, for example, if you are stimulated by the smell of food, but that food is not available for you to eat. Drooling is an extreme instance of the overproduction of saliva. During times of stress, such as before speaking in public, sympathetic stimulation takes over, reducing salivation and producing the symptom of dry mouth often associated with anxiety. When you are dehydrated, salivation is reduced, causing the mouth to feel dry and prompting you to take action to quench your thirst.
Salivation can be stimulated by the sight, smell, and taste of food. It can even be stimulated by thinking about food. You might notice whether reading about food and salivation right now has had any effect on your production of saliva.
How does the salivation process work while you are eating? The food contains chemicals that stimulate taste receptors on the tongue, which send impulses to the superior and inferior salivatory nuclei in the brain stem. These two nuclei then send back parasympathetic impulses through fibers in the glossopharyngeal and facial nerves, stimulating salivation. Even after you swallow food, salivation is increased to cleanse the mouth and water down and neutralize any irritating chemical remnants, such as that hot sauce in your burrito. Most saliva is swallowed along with food and is reabsorbed so that fluid is not lost.
The Teeth
The teeth are organs similar to bones that you use to tear, grind, and otherwise mechanically break down food.
Types of Teeth
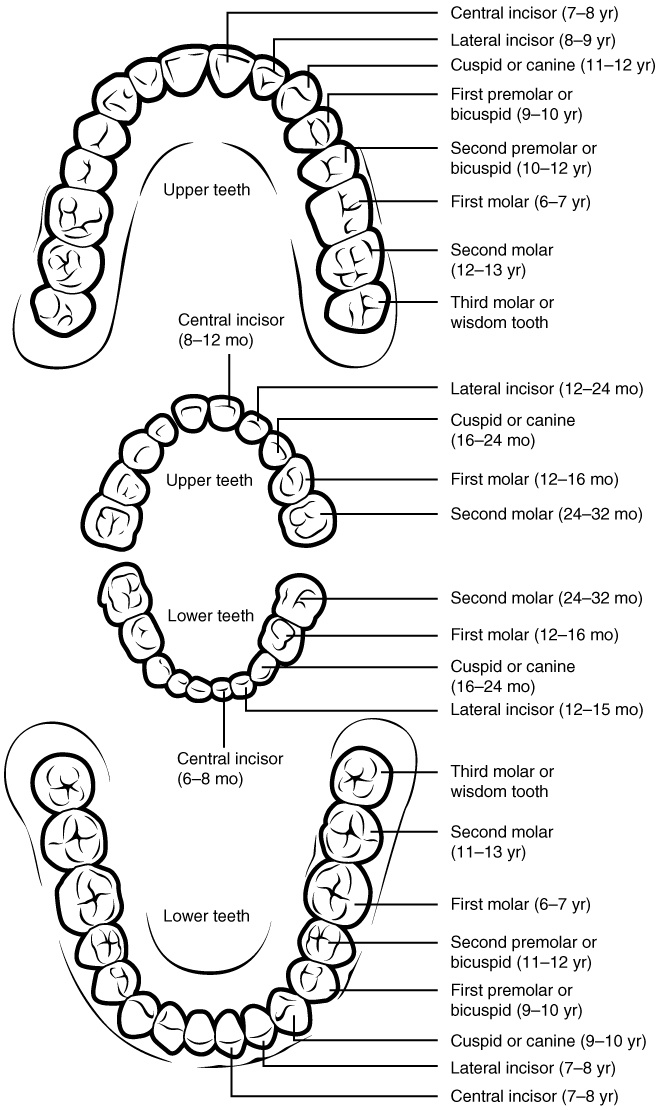
During the course of your lifetime, you have two sets of teeth (one set of teeth is a dentition). Your 20 deciduous teeth, or baby teeth, first begin to appear at about 6 months of age. Between approximately ages 6 and 12, these teeth are replaced by 32 permanent teeth. Moving from the center of the mouth toward the side, these are as follows:
- The eight incisors, four top, and four bottom, are the sharp front teeth you use for biting into food.
- The four cuspids (or canines) flank the incisors and have a pointed edge (cusp) to tear up food. These fang-like teeth are superb for piercing tough or fleshy foods.
- Posterior to the cuspids are the eight premolars (or bicuspids), which have an overall flatter shape with two rounded cusps useful for mashing foods.
- The most posterior and largest are the 12 molars, which have several pointed cusps used to crush food, so it is ready for swallowing. The third members of each set of three molars, top and bottom, are commonly referred to as the wisdom teeth because their eruption is commonly delayed until early adulthood. It is not uncommon for wisdom teeth to fail to erupt; that is, they remain impacted. In these cases, the teeth are typically removed by orthodontic surgery.
Permanent and Deciduous Teeth
Anatomy of a Tooth
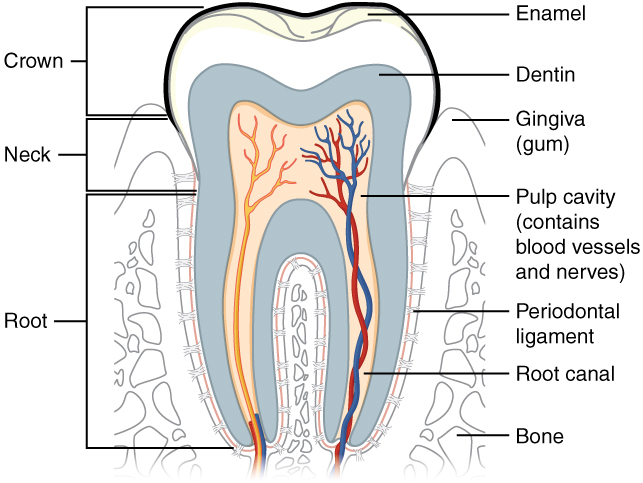
The teeth are secured in the alveolar processes (sockets) of the maxilla and the mandible. Gingivae (commonly called the gums) are soft tissues that line the alveolar processes and surround the necks of the teeth. Teeth are also held in their sockets by a connective tissue called the periodontal ligament.
The two main parts of a tooth are the crown, the portion projecting above the gum line, and the root embedded within the maxilla and mandible. Both parts contain an inner pulp cavity, containing loose connective tissue through which nerves and blood vessels run. The region of the pulp cavity that runs through the root of the tooth is called the root canal. Surrounding the pulp cavity is dentin, a bone-like tissue. In the root of each tooth, the dentin is covered by an even harder bone-like layer called cementum. In the crown of each tooth, the dentin is covered by an outer layer of enamel, the hardest substance in the body.
Although enamel protects the underlying dentin and pulp cavity, it is still nonetheless susceptible to mechanical and chemical erosion, or what is known as tooth decay. The most common form, dental caries (cavities), develops when colonies of bacteria feeding on sugars in the mouth release acids that cause soft tissue inflammation and degradation of the calcium crystals of the enamel.
The Structure of the Tooth
| Digestive Functions of the Mouth | ||
|---|---|---|
| Structure | Action | Outcome |
| Lips and cheeks | Confine food between teeth |
|
| Salivary glands | Secrete saliva |
|
| Tongue’s extrinsic muscles | Move tongue sideways and in and out |
|
| Tongue’s intrinsic muscles | Change tongue shape |
|
| Taste buds | Sense food in mouth and sense taste |
|
| Lingual glands | Secrete lingual lipase |
|
| Teeth | Shred and crush food |
|
Muscles That Move the Lower Jaw
In anatomical terminology, chewing is called mastication. The temporomandibular joint connects the temporal bone and mandible in a synovial joint. The muscles of mastication create the movement of the temporomandibular joint. Muscles involved in chewing must exert enough pressure to bite through and then chew food before swallowing. The masseter muscle is the main muscle used for chewing because it elevates the mandible (lower jaw) to close the mouth. It is assisted by the temporalis muscle, which retracts the mandible. You can feel the temporalis move by putting your fingers to your temple as you chew. Although the masseter and temporalis are responsible for elevating and closing the jaw to break food into digestible pieces, the medial pterygoid and lateral pterygoid muscles assist in chewing and moving food within the mouth.
Muscles That Move the Lower Jaw
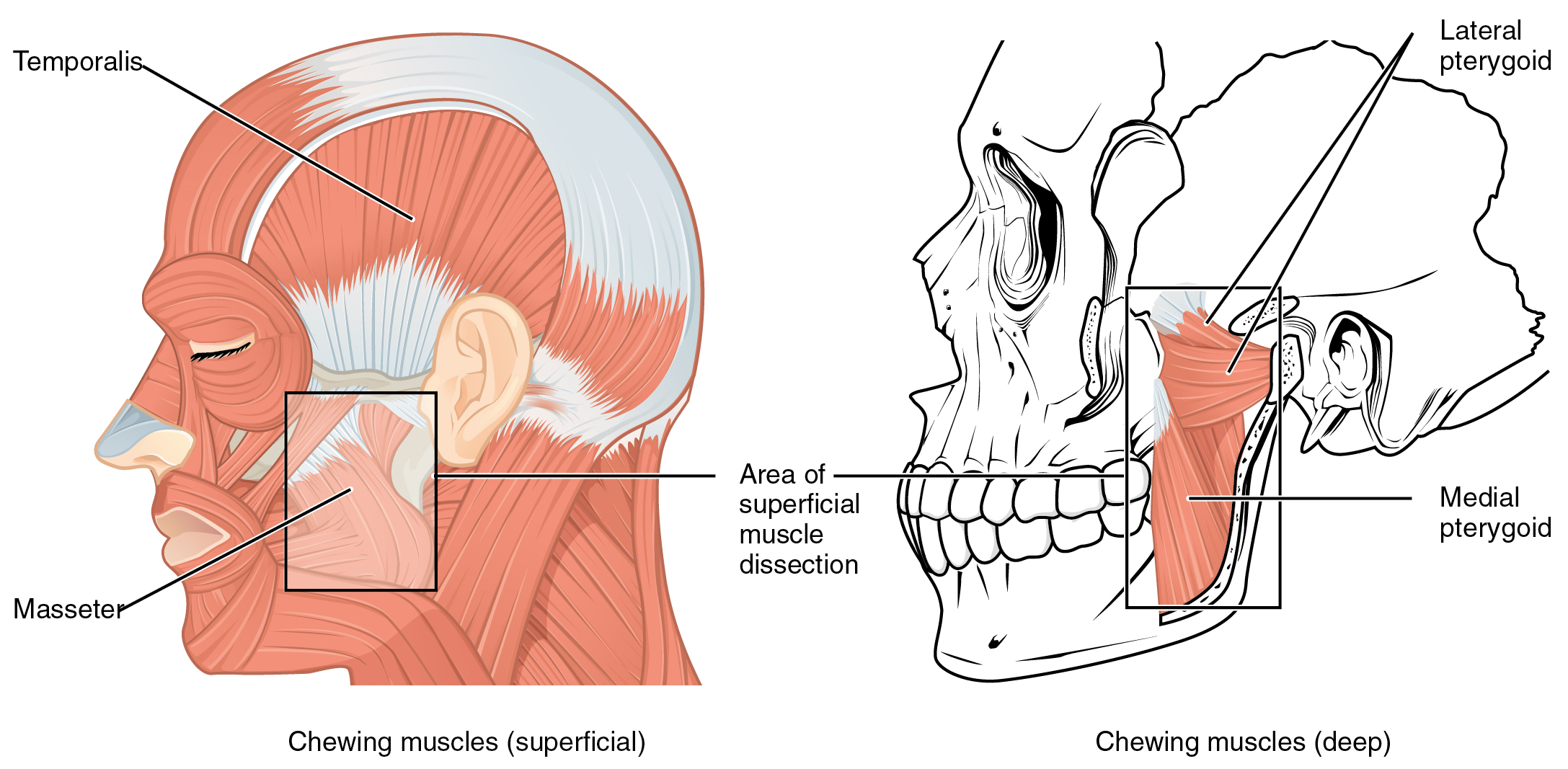
| Muscles of the Lower Jaw | |||||
|---|---|---|---|---|---|
| Movement | Target | Target motion direction | Prime mover | Origin | Insertion |
| Closes mouth; aids chewing | Mandible | Superior (elevates) | Masseter | Maxilla arch; zygomatic arch (for masseter) | Mandible |
| Closes mouth; pulls lower jaw in under upper jaw | Mandible | Superior (elevates); posterior (retracts) | Temporalis | Temporal bone | Mandible |
| Opens mouth; pushes lower jaw out under upper jaw; moves lower jaw side-to-side | Mandible | Inferior (depresses); posterior (protracts); lateral (abducts); medial (adducts) | Lateral pterygoid | Pterygoid process of sphenoid bone | Mandible |
| Closes mouth; pushes lower jaw out under upper jaw; moves lower jaw side-to-side | Mandible | Superior (elevates); posterior (protracts); lateral (abducts); medial (adducts) | Medial pterygoid | Sphenoid bone; maxilla | Mandible; temporo-mandibular joint |
Nerves of the tongue
The tongue allows us to manipulate food, push food/liquid (bolus) back towards the oropharynx to begin the swallowing process, and produce sound using the intrinsic and extrinsic muscles. The tongue also provides information about touch and taste. The special sense of taste is also known as gustation.
Motor Innervation
The hypoglossal nerve (CN XII) provides motor innervation to all of the intrinsic and extrinsic muscles of the tongue except for the palatoglossus muscle, which is innervated by the vagus nerve (CN X). Lesions of the hypoglossal nerve cause the tongue’s deviation to the ipsilateral (i.e., damaged) side. For example, when attempting to protrude (stick out) the tongue, a person with a lesion to the right hypoglossal nerve would protrude their tongue, but it would deviate to the right side of their oral cavity.
General Sensation
General sensation to the anterior two-thirds of the tongue is by innervation from a branch of the trigeminal nerve (CN V). General sensation to the posterior one-third of the tongue is by innervation from the glossopharyngeal nerve (CN IX).
Taste (Special Sense)
Taste to the anterior two-thirds of the tongue is achieved through innervation from a branch of the facial nerve (CN VII). On the other hand, taste to the posterior one-third of the tongue is accomplished through innervation from the glossopharyngeal nerve (CN IX). Taste perception is also performed by both the epiglottis and the tongue’s epiglottic region, which receives taste and general sensation from innervation from a branch of the vagus nerve (CN X).
Gustation (Taste)
Only a few recognized submodalities exist within the sense of taste or gustation. Until recently, only four tastes were recognized: sweet, salty, sour, and bitter. Research at the turn of the 20th century led to recognizing the fifth taste, umami, during the mid-1980s. Umami is a Japanese word that means “delicious taste” and is often translated to mean savory. Very recent research has suggested that there may also be a sixth taste for fats or lipids.
Gustation is the special sense associated with the tongue. The tongue’s surface, along with the rest of the oral cavity, is lined by a stratified squamous epithelium. Raised bumps called papillae (singular = papilla) contain the structures for gustatory transduction. There are four types of papillae based on their appearance: (circum)vallate, foliate, filiform, and fungiform. Within the structure of the papillae are taste buds that contain specialized gustatory receptor cells for the transduction of taste stimuli. These receptor cells are sensitive to the chemicals contained within foods ingested, and they release neurotransmitters based on the amount of the chemical in the food. Neurotransmitters from the gustatory cells can activate sensory neurons in the facial, glossopharyngeal, and vagus cranial nerves.
The Tongue
Taste FYI – For Your Information (-> you will not be assessed on this content)
Salty taste is simply the perception of sodium ions (Na+) in the saliva. When you eat something salty, the salt crystals dissociate into the component ions Na+ and Cl–, which dissolve into the saliva in your mouth. The Na+ concentration becomes high outside the gustatory cells, creating a strong concentration gradient that drives the diffusion of the ion into the cells. The entry of Na+ into these cells results in the depolarization of the cell membrane and the generation of a receptor potential.
Sour taste is the perception of H+ concentration. Just as with sodium ions in salty flavors, these hydrogen ions enter the cell and trigger depolarization. Sour flavors are, essentially, the perception of acids in our food. Increasing hydrogen ion concentrations in the saliva (lowering saliva pH) triggers progressively stronger graded potentials in the gustatory cells. For example, orange juice—which contains citric acid—will taste sour because it has a pH value of approximately 3. Of course, it is often sweetened so that the sour taste is masked.
The first two tastes (salty and sour) are triggered by the cations Na+ and H+. The other tastes result from food molecules binding to a G protein-coupled receptor. A G protein signal transduction system ultimately leads to depolarization of the gustatory cell. The sweet taste is the sensitivity of gustatory cells to the presence of glucose dissolved in the saliva. Other monosaccharides such as fructose or artificial sweeteners such as aspartame (NutraSweet™), saccharine, or sucralose (Splenda™) also activate the sweet receptors. The affinity for each of these molecules varies, and some will taste sweeter than glucose because they bind to the G protein–coupled receptor differently.
Bitter taste is similar to sweet in that food molecules bind to G protein–coupled receptors. However, there are several different ways this can happen because there is a large diversity of bitter-tasting molecules. Some bitter molecules depolarize gustatory cells, whereas others hyperpolarize gustatory cells. Likewise, some bitter molecules increase G protein activation within the gustatory cells, whereas other bitter molecules decrease G protein activation. The specific response depends on which molecule is binding to the receptor.
One major group of bitter-tasting molecules are alkaloids. Alkaloids are nitrogen-containing molecules commonly found in bitter-tasting plant products, such as coffee, hops (in beer), tannins (in wine), tea, and aspirin. By containing toxic alkaloids, the plant is less susceptible to microbe infection and less attractive to herbivores.
Therefore, the function of bitter taste may primarily be related to stimulating the gag reflex to avoid ingesting poisons. Because of this, many bitter foods that are normally ingested are often combined with a sweet component to make them more palatable (cream and sugar in coffee, for example). The highest concentration of bitter receptors appears to be in the posterior tongue, where a gag reflex could still spit out poisonous food.
The taste known as umami is often referred to as the savory taste. Like sweet and bitter, it is based on the activation of G protein-coupled receptors by a specific molecule. The molecule that activates this receptor is the amino acid L-glutamate. Therefore, the umami flavor is often perceived while eating protein-rich foods. Not surprisingly, dishes that contain meat are often described as savory.
Once the gustatory cells are activated by the taste molecules, they release neurotransmitters onto the dendrites of sensory neurons. These neurons are part of the facial and glossopharyngeal cranial nerves and a component within the vagus nerve dedicated to the gag reflex. The facial nerve connects to taste buds in the anterior two thirds of the tongue. The glossopharyngeal nerve connects to taste buds in the posterior third of the tongue. The vagus nerve connects to taste buds in the extreme posterior of the tongue.
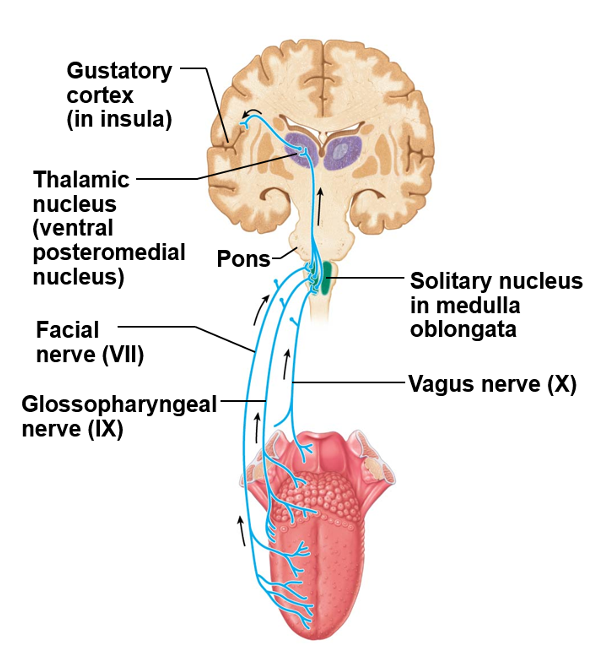
The sensory pathway for gustation travels along the facial and glossopharyngeal cranial nerves and synapses with neurons of the solitary nucleus in the brain stem. Axons from the solitary nucleus then project to the ventral posterior nucleus of the thalamus. Finally, axons from the ventral posterior nucleus project to the gustatory cortex of the cerebral cortex, where taste is processed and consciously perceived.

