Module 3: Spinal Cord and Reflexes
Learning Objectives:
By the end of this class, students will be able to:
- Describe the anatomy of the spinal cord and identify its regional variations.
- Explain the functional pathways in the spinal cord.
- Predict the deficits associated with injury to specific regions of the spinal cord.
- Explain the different types of reflexes.
Terms to Know
|
Vertebral Column
Gross Anatomy
|
Pathways
Reflexes
*Covered only in lecture, not in this text |
Gross Anatomy of the Spinal Cord
This information is covered in the assignment and reviewed and built upon in lecture.
The spinal cord transmits information between the brain and the body (with the exception of most structures in the head and neck, which have information carried in cranial nerves, covered in unit 3). The spinal cord is located in the vertebral foramen at the center of the vertebral column. As a result the spinal cord is surrounded and protected by bone. The central canal is located in the center of the spinal cord and contains cerebrospinal fluid. The spinal cord is also surrounded by cerebrospinal fluid, which provides nourishment and protection, as well as connective tissue layers called the meninges that also provide additional protection.
Regions of the Spinal Cord
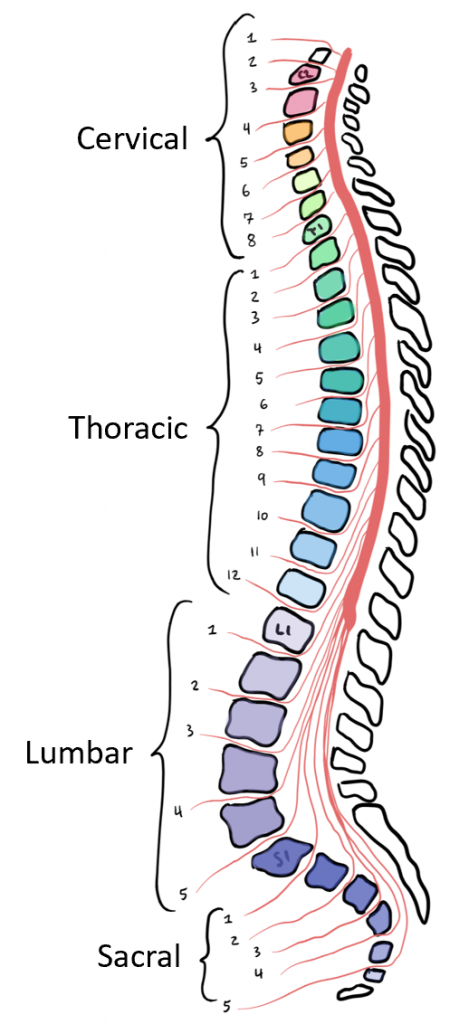
The length of the spinal cord is divided into regions that correspond to the regions of the vertebral column. Superiorly, immediately adjacent to the brain stem is the cervical region, followed by the thoracic, then the lumbar, and finally the sacral region.
There are two portions of the spinal cord that have a larger diameter in order to house more cell bodies for more neurons that will go out to innervate specific parts of the body. The cervical enlargement houses neurons that will innervate the muscles of the upper extremities, while the lumbar enlargement will innervate the muscles of the lower extremity. The cervical enlargement is particularly large because there is greater control over the fine musculature of the upper limbs, particularly of the fingers. The lumbar enlargement is not as significant in appearance because there is less fine motor control of the lower limbs.
The spinal cord is not the full length of the vertebral column because the spinal cord only grows until around age four, but the skeleton continues to grow years beyond that. As the vertebral column grows, the spinal nerves (discussed later) grow with it and result in a long bundle of nerves that resembles a horse’s tail and is named the cauda equina. The sacral spinal cord is at the level of the upper lumbar vertebral bones. The spinal nerves extend from their various levels to the proper level of exit from the vertebral column. The most inferior portion of the spinal cord is called the conus medularis, and it falls around the level of the first lumbar vertebrae.
Internal Anatomy of the Spinal Cord
In the CNS, regions with many cell bodies and dendrites are referred to as gray matter, while regions composed primarily of myelinated axons are called white matter. White matter is white because axons are insulated by myelin, which is a lipid-rich (fatty) substance. Though it isn’t actually gray, gray matter may have that color ascribed to it because, next to the white matter, it is just darker. Gray matter and white matter can be seen with the unaided eye in the CNS.
Gray Matter: Horns
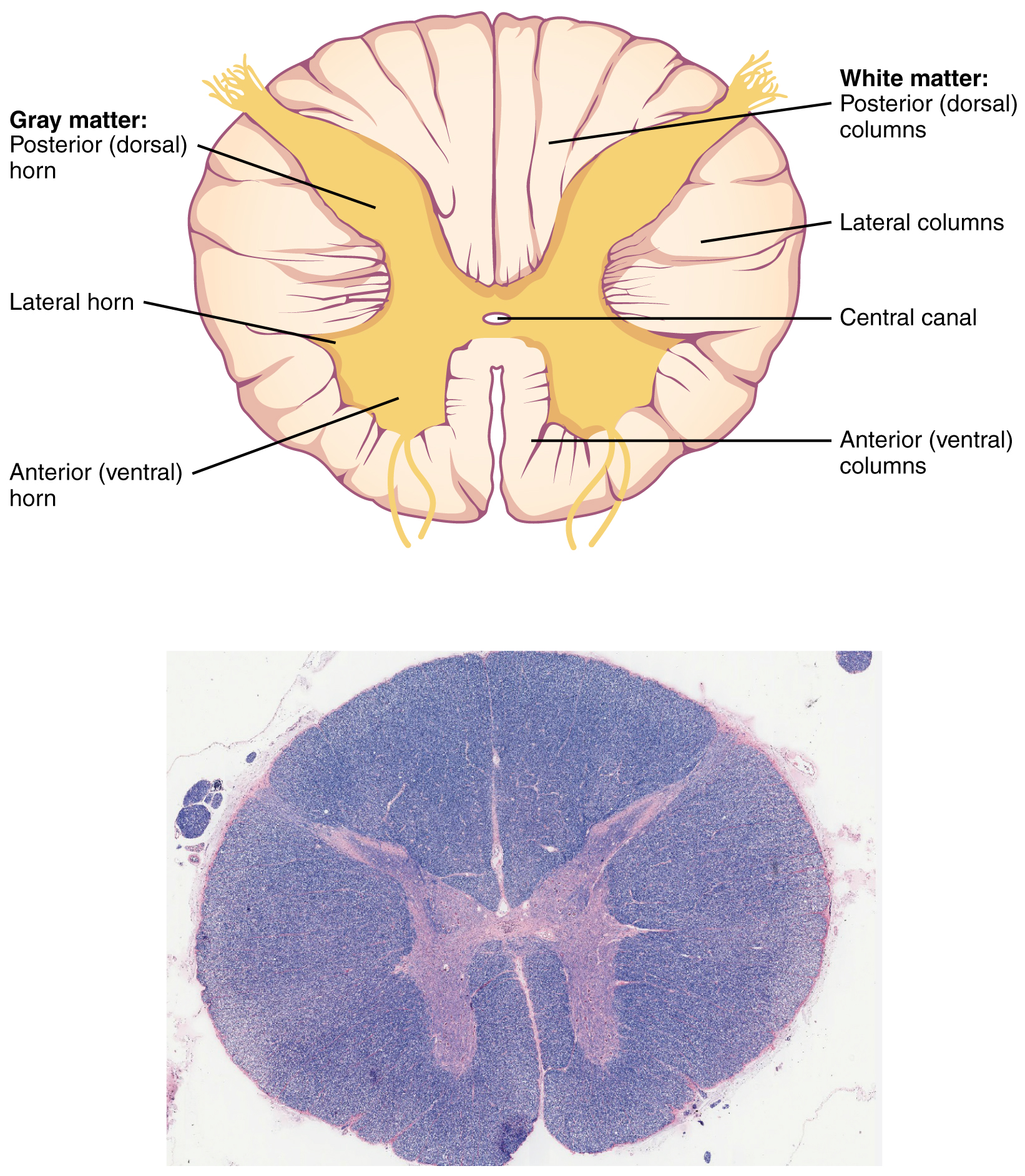
In cross-section, the gray matter of the spinal cord has a shape somewhat similar to a capital “H.” The gray matter is subdivided into regions that are referred to as horns. The dorsal or posterior horn is responsible for sensory processing. The ventral or anterior horn sends out motor signals to the skeletal muscles. Note that it is common to see the terms dorsal (dorsal = “back”) and ventral (ventral = “belly”) used interchangeably with posterior and anterior, particularly in reference to nerves and the structures of the spinal cord. You should be comfortable using both terms interchangeably. The lateral horn, which is only found in the thoracic region (and less prominent in the very upper lumbar region), is the central component of the sympathetic division of the autonomic nervous system (covered in unit 2).
White Matter: Columns
Just as the gray matter is separated into horns, the white matter of the spinal cord is separated into columns. The columns extend along the entire length of the spinal cord as continuous bands of white matter. Between the two posterior horns of gray matter are the posterior columns. Roughly between the two anterior horns are the anterior columns. The white matter on either side of the spinal cord, between the posterior horn and the anterior horn, are the lateral columns.
Nerves Entering and Exiting the Spinal Cord
Emerging from the spinal cord bilaterally, dorsal and ventral rootlets merge to form dorsal and ventral roots at each spinal cord segment. The ventral roots contain only the axons of motor neurons carrying information away from the spinal cord to muscles and glands. The dorsal roots contain only the axons of sensory neurons carrying information to the CNS from the periphery. The dorsal root ganglion for each nerve is seen as an enlargement of the dorsal root near the spinal nerve, and it it contains the cell bodies for pseudounipolar sensory neurons.
The dorsal and ventral roots merge a short distance from the spinal cord to form the spinal nerve. As a result, all of the spinal nerves carry both sensory and motor axons. Each spinal nerve then branches into a dorsal ramus (plural: rami), which carries both sensory and motor information from or to the posterior trunk, and the ventral ramus, which carries both sensory and motor information from or to the extremities and anterior trunk.
There are 31 spinal nerves, named for the level of the spinal cord at which each one emerges.
- 8 pairs of cervical nerves designated C1 to C8
- 12 thoracic nerves designated T1 to T12
- 5 pairs of lumbar nerves designated L1 to L5
- 5 pairs of sacral nerves designated S1 to S5
- 1 pair of coccygeal nerves
The spinal nerves are numbered from the superior to inferior positions, and each emerges from the vertebral column through the intervertebral foramen at its level. The first nerve, C1, emerges between the first cervical vertebra and the occipital bone. C2 through C7 emerge superior to the vertebrae of the same number, but C8 emerges between the seventh cervical vertebra and the first thoracic vertebra. For the thoracic and lumbar nerves, each one emerges inferior to the vertebra of the same number. The sacral nerves emerge from the sacral foramina along the length of that unique vertebra.
Spinal Cord Pathways
This information will be covered in lecture.
In this section you will learn about the pathways that carry information through the spinal cord, either in from the periphery to the brain, or from the brain out to the periphery. We will only discuss these pathways through the spinal cord, meaning that we will not follow them all the way to or from their structures in the brain. That information can be found on additional pathway slides posted on canvas in gray text, but you will not be asked about it in this unit. You will learn about the structures of the brainstem, cerebellum, and cerebrum in Unit 3. Sensory and motor information going to or from the head and neck follow different pathways, and we will discuss those more in Unit 3.
Ascending pathways of nervous system fibers in these columns carry sensory information up to the brain, whereas descending pathways carry motor commands from the brain. The posterior columns are composed of axons of ascending tracts. The anterior and lateral columns are composed of many different groups of axons of both ascending and descending tracts. Most pathways of the spinal cord decussate at some point, meaning they cross to the contralateral side from where they originated. That means that the right side of the brain is processing incoming or outgoing information from the left side of the body, and the left side of the brain is processing incoming or outgoing information for the right side of the body.
Sensory Pathways
A sensory pathway that carries peripheral sensations to the brain is referred to as an ascending pathway. Different types of somatic sensory information each follow specific pathways through the CNS.
Note that we will use the terms first order neuron, second order neuron, and third order neuron with sensory pathways. That simply means the first neuron in the pathway, the second neuron in the pathway, and the third neuron in the pathway.
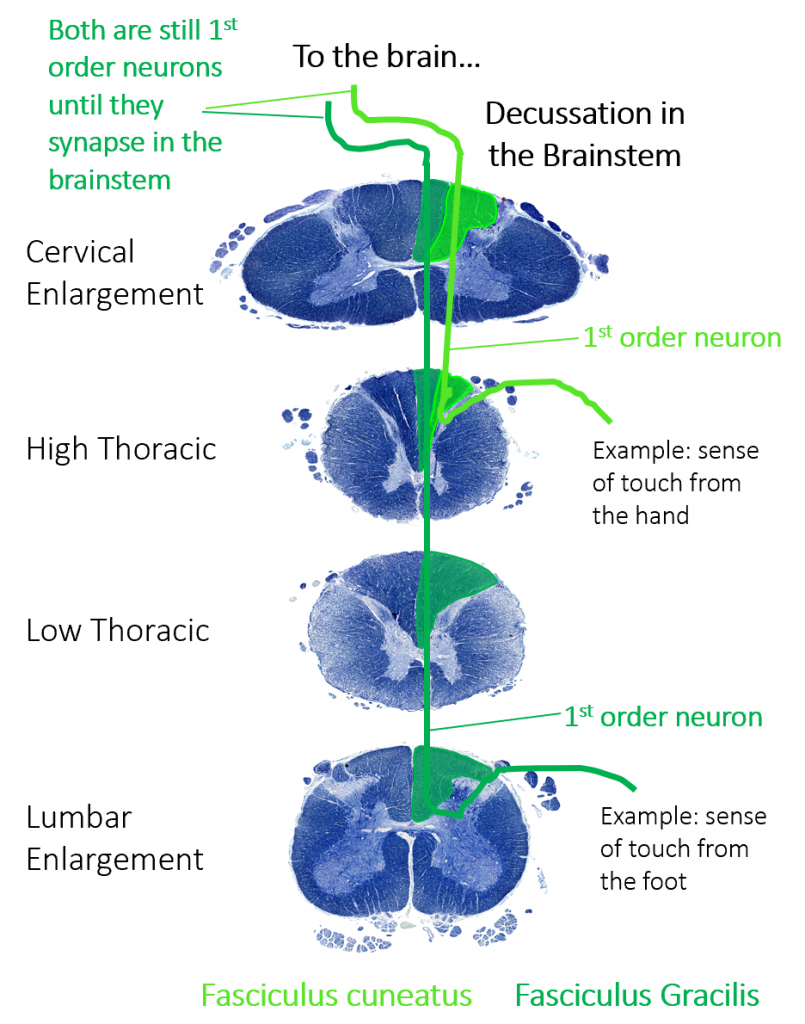
Dorsal Column-Medial Lemniscus (DCML) Pathway
The dorsal column-medial lemniscus (DCML) pathway carries information about fine, discriminative touch and light pressure. It begins with the sensory axon carrying information from receptors in the periphery through the spinal nerve and dorsal root. The first order neuron in this pathway has a cell body in the dorsal root ganglion. The axons of the first order neuron enter the dorsal column of white matter in the spinal cord. (The dorsal column is separated into two component tracts, the fasciculus gracilis that contains axons from the legs and lower body, and the fasciculus cuneatus that contains axons from the upper body and arms. However, we will not ask you about this on the exam.)
The axons of the first order neuron in the dorsal column ascend all they way to the brainstem before synapsing there, making these very long neurons. The second order neuron then decussates, or crosses the midline in the brainstem and ascend to other brain structures. (They synapse with the third order neuron in the thalamus before reaching their destination in the primary somatosensory cortex of the parietal lobe. This is simply finishing the pathway for you, but you will not be asked about this on the exam.)
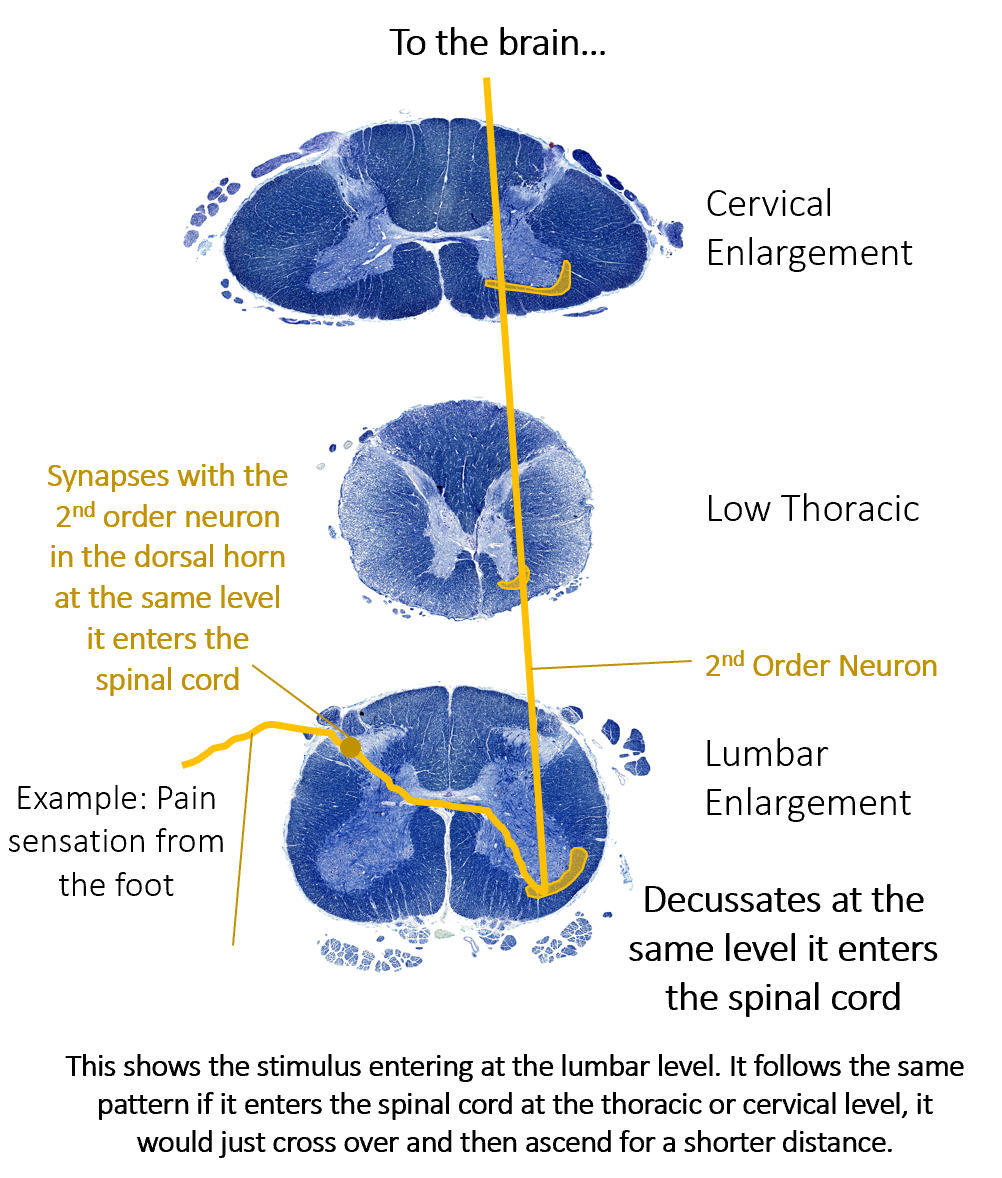
Anterolateral System
The anterolateral system (sometimes abbreviated ALS, though this is not related to the disease ALS) is sometimes called the spinothalamic tract, as two spinothalamic tracts primarily compose the anterolateral system. However, they follow the same path, so we will refer to them together as one pathway, the anterolateral system, in this course. The anterolateral system carries sensory information about pain, temperature, and crude touch.
Like the DCML, the anterolateral system begins with neurons that travel through the spinal nerve and dorsal root, with a cell body in the dorsal root ganglion. These neurons extend their axons to the dorsal horn, where they synapse with the second neuron in their respective pathway. Axons from these second neurons then decussate within the spinal cord at (or near) the level that they enter. From there they ascend to the brain. (Like the DCML pathway, the second order neuron synapses in the thalamus, and the third order neuron then projects to one of two areas in the cerebral cortex. You will not be asked about that on the exam.)
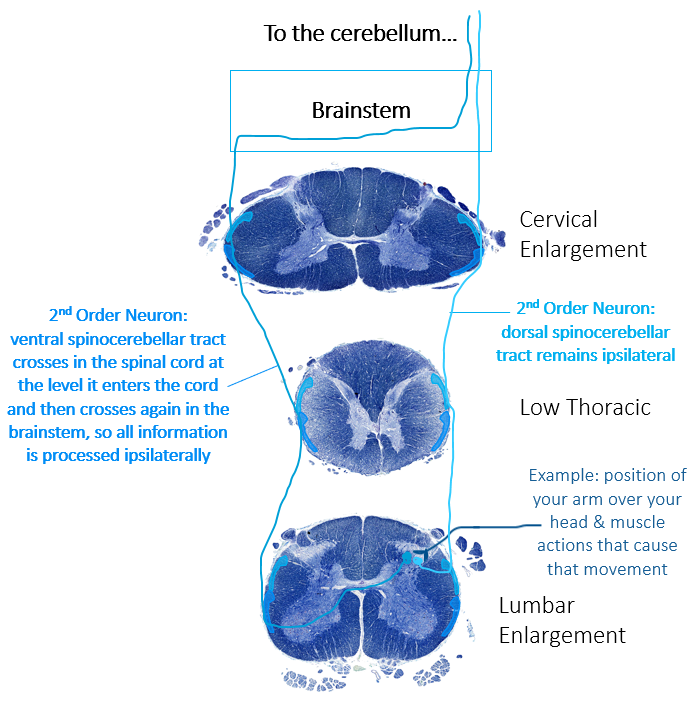
Spinocerebellar Pathway
The spinocerebellar pathway senses proprioceptive information. It is divided into dorsal and ventral portions, with the dorsal carrying information about the action of individual muscles and the ventral portion carrying information about the position of the limb as a whole. The first order neuron begins like the other sensory pathways, with an axon entering the spinal nerve, then the dorsal root, with a cell body in the dorsal root ganglion. It then enters the posterior horn and synapses there. From there, all we want you to know is that a portion of this pathway stays ipsilateral for its entire path, while the other portion of the pathway decussates at the level it enters the spinal cord and then crosses back over to the side it originated from in the brainstem. As a result all information that travels in the spinocerebellar pathway is ultimately processed in the ipsilateral cerebellum, the target for this pathway.
Descending Pathways
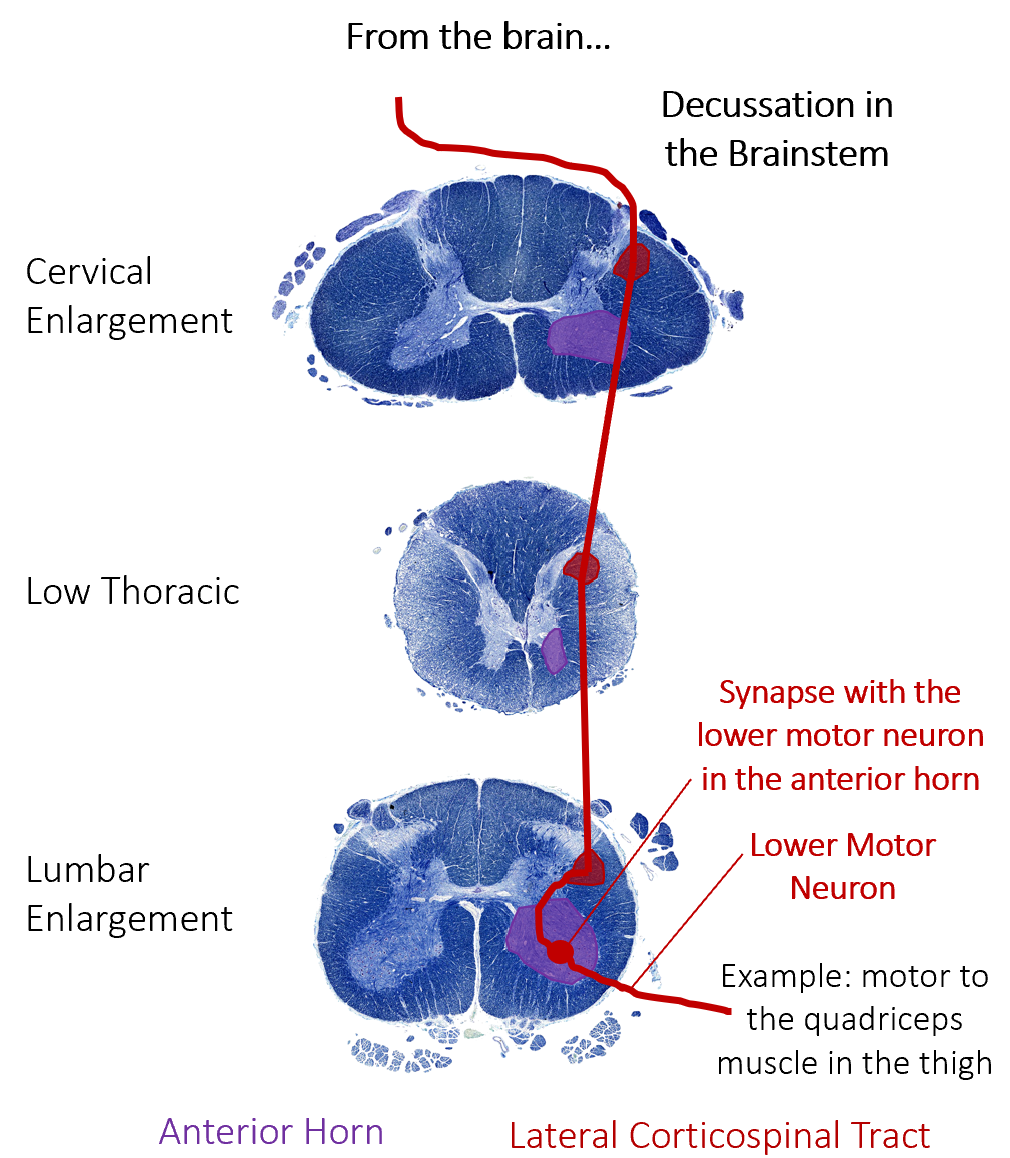
The motor output from the cortex descends into the brain stem and to the spinal cord to control the voluntary movements through motor neurons. In the descending pathways we have an upper motor neuron and a lower motor neuron.
- Upper Motor Neurons: These neurons originate in the brain and descend through the spinal cord until they reach the level that the pathway will exit the spinal cord. At that point they enter the anterior (ventral) horn and synapse with the lower motor neuron. The upper motor neuron can either excite or inhibit the lower motor neuron, meaning it can cause the lower motor neuron to send a signal to the muscle to contract or it can prevent the lower motor neuron from sending that signal.
- Lower Motor Neurons: The lower motor neurons originate in the anterior (ventral) horn of the spinal cord. The axon travels through the ventral root to join the spinal nerve on its way out to a skeletal muscle. The axon is relatively long because it needs to reach muscles in the periphery of the body. Some axons are a meter in length, such as the lumbar motor neurons that innervate muscles in the feet. The axons will also branch to innervate multiple muscle fibers forming a motor unit, as discussed in Module 2. If a lower motor neuron is excited by an upper motor neuron, the muscle will contract. (The lower motor neuron cannot inhibit the muscle.)
Corticospinal Tract
Axons of the corticospinal tract are largely contralateral, meaning that they cross the midline of the brain stem or spinal cord and synapse on the opposite side of the body. Therefore, the right motor cortex of the cerebrum controls muscles on the left side of the body, and vice versa.
The corticospinal tract descends from the cortex through the deep white matter of the brain. It then passes through the brainstem where the vast majority of fibers decussate. (We will only focus on the decussating fibers in this class.)
The motor neuron that causes contraction of the big toe, for example, is located in the sacral spinal cord. The axon that has to reach all the way to the belly of that muscle may be a meter in length. The neuronal cell body that maintains that long fiber must be quite large, possibly several hundred micrometers in diameter, making it one of the largest cells in the body.
Reflexes
This section will provide a brief introduction to reflexes, as this content is covered thoroughly in the slides and lecture.
Simple somatic reflexes do not include the higher centers discussed for conscious or voluntary aspects of movement. However, we do become consciously aware that a reflex occurred, even though we don’t need our higher centers to cause the reflex.
Reflexes involve a receptor in the periphery, a sensory neuron that carries the information to the spinal cord, integration in the spinal cord (which sometimes involves an interneuron), a motor neuron to carry the response to the effector (a muscle for somatic reflexes), and the effector itself. Reflexes can be monosynaptic, meaning just one synapse in the pathway, or polysynaptic, meaning more than one synapse in the pathway.
We will discuss a few different types of reflexes:
- Monosynaptic stretch reflex: In this reflex, when a skeletal muscle is stretched, a muscle spindle receptor is activated. The axon from this receptor structure will cause direct contraction of the muscle. A common example of this reflex is the knee jerk that is elicited by a rubber hammer struck against the patellar ligament in a physical exam.
- Golgi tendon reflex: In this reflex, lower motor neurons are inhibited in response to too much tension on a muscle, as sensed by a Golgi tendon organ. This prevents excessive tension, such as trying to lift too much weight, in order to protect the muscle and tendon.
- Polysynaptic withdrawal reflex: When you touch a hot stove, you pull your hand away. Sensory receptors in the skin sense extreme temperature and the early signs of tissue damage. This signal travels along the sensory fiber from the skin, through the dorsal root to the posterior horn, where it synapses on an interneuron. The interneuron then signals a ventral horn motor neuron, which innervates the muscles needed to pull your hand away from the stove. It also inhibits the muscles that would oppose that movement and activates muscles involved in balancing posture while the arm is forcefully withdrawn. This is one example of a polysynaptic withdrawal reflex, but it would occur with any reflexive response to pain or extreme temperatures, such as stepping on something sharp.

