Module 10: Autonomic Nervous System
Learning Objectives:
By the end of this class, students will be able to:
- Compare and contrast the somatic and autonomic nervous systems.
- Compare and contrast the parasympathetic and sympathetic divisions.
- Explain dual innervation by the parasympathetic and sympathetic divisions.
- Describe an autonomic plexus, including the fibers carried within a plexus.
- Describe the anatomy of the parasympathetic divisions.
- Describe the sympathetic chain and the rami connecting it to the spinal nerve.
- Describe the anatomy of the four pathways of the sympathetic division.
- Describe the effects of the parasympathetic and sympathetic divisions on organs and organ systems throughout the body.
- Explain referred pain.
Terms to Know
General
Autonomic Plexuses
Parasympathetic Division
|
Sympathetic Division
*Covered only in lecture, not in this text |
Somatic Vs. Autonomic Nervous System
*This content will be covered in the assignment, primarily as self-study. Portions will be briefly reviewed in lecture.
The nervous system can be divided into two functional parts: the somatic nervous system and the autonomic nervous system. The somatic nervous system causes voluntary contraction of skeletal muscles (though contraction can happen without conscious awareness, like breathing). This is the branch of the nervous system we were describing with the corticospinal tract and lower motor neurons in Unit 1. The autonomic nervous system controls involuntary contraction of cardiac and smooth muscle, as well as glandular tissue. You may remember from Unit 1 that lower motor neurons can only excite their effector. That means that, if the lower motor neuron is stimulated, it will cause the muscle to contract. In the autonomic nervous system, stimulation can either excite or inhibit the effector. That means it can cause muscle contraction or secretion from a gland, or it can prevent those actions from occurring.
There are a few key differences in the neurons and neuronal pathways between the somatic and autonomic nervous systems. The somatic nervous system has just one lower motor neuron traveling from the spinal cord to the effector muscle. Since there is only one neuron, there is no synapse between neurons, and thus, no ganglia. That lower motor neuron originates in the ventral (anterior) horn of the spinal cord. In the autonomic nervous system there are two neurons in the pathway from the spinal cord to the effector organ. The synapse between the two neurons occurs at a ganglion, or a collection of cell bodies. The neurons that originate in the spinal cord begin in the lateral horn. In the somatic nervous system, the lower motor neuron axons are highly myelinated, allowing for a very rapid signal transmission from the spinal cord to the effector. In the autonomic nervous system, the axons are either lightly myelinated (meaning a thin layer of myelin) or unmyelinated, resulting in a slower conduction speed.
Divisions of the Autonomic Nervous System
*This content will be covered in the assignment, primarily as self-study. Portions will be briefly reviewed in lecture.
The two divisions of the autonomic nervous system are the sympathetic division and the parasympathetic division.
- The sympathetic division is associated with the fight-or-flight response, preparing the body to respond to potentially dangerous situations. It is active in situations of fear or rage, for example, and it is also active when we exercise. Its pathways originate from the thoracic and first two lumbar levels of the spinal cord, and as a result, it is sometimes called the thoracolumbar division.
- The parasympathetic division is associated with rest and digest, conserving energy, replenishing energy stores, and conducting routine maintenance. Its pathways originate from the brainstem, traveling to effectors via cranial nerves, or from sacral levels S2-S4 in the spinal cord. This division is sometimes called the craniosacral division.
Most target effectors receive dual innervation, meaning they receive innervation from both the parasympathetic and sympathetic divisions. Whichever is most active at a given time will determine the activity of the effector at that time. For example, the heart receives connections from both the sympathetic and parasympathetic divisions. One causes heart rate to increase, whereas the other causes heart rate to decrease. The situation that we are in determines which division is most active (i.e. resting vs. a stressful situation).
In both divisions we have preganglionic and postganglionic neurons. The preganglionic neuron is the first neuron in the pathway running from the spinal cord to the ganglion to synapse with the second neuron. The postganglionic neuron is the second neuron in the pathway, running from the ganglion to the effector.
- In the sympathetic division, the ganglia tend to be relatively close to the spinal cord, located in either the sympathetic trunk (chain) or the prevertebral ganglia (more on those later). As a result, the sympathetic division has a short preganglionic axon and a long postganglionic axon.
- In the parasympathetic division, the ganglia are located either near or in the target organ. Terminal ganglia are located near the target organ, while intramural ganglia are located within the wall of the target organ. As a result, the parasympathetic division has a long preganglionic axon and short postganglionic axons in its pathways.
The short postganglionic axon in the parasympathetic system means that the parasympathetic system can only have a very local effect. The postganglionic neuron can’t travel far from the ganglion because it is so short. In the sympathetic system, two postganglionic neurons that synapsed in the ganglion with the same preganglionic neuron can travel to effector tissues that are further from each other, giving it a somewhat more widespread effect. In addition, the sympathetic division can cause the adrenal gland to secrete epinephrine and norepinephrine into the bloodstream, resulting in very widespread effects throughout the body. We will talk more about the adrenal gland later in this module.
Axons in the autonomic nervous system travel through plexuses to get to their destination. A plexus is essentially a web of intertwining axons and nerves traveling to their destination. Axons from both the parasympathetic division and sympathetic division travel in the same plexus, and all autonomic plexuses we will discuss have axons that carry information from both divisions. As a result of the axonal lengths in each division (sympathetic = long postganglionic axon, parasympathetic = long preganglionic axon), a plexus will contain preganglionic parasympathetic fibers and postganglionic sympathetic fibers. This is drawn out in lecture.
Neurotransmitters are signaling molecules released at synapses. We say very little about neurotransmitters in this course, as they are covered extensively in physiology. However I want you to know the following about the neurotransmitters used for signaling in the divisions of the autonomic nervous system:
- Parasympathetic division:
- Synapse between the preganglionic and postganglionic neurons = Acetylcholine
- Synapse between the postganglionic neuron and the effector = Acetylcholine
- Sympathetic division:
- Synapse between the preganglionic and postganglionic neurons = Acetylcholine
- Synapse between the postganglionic neuron and the effector = Norepinephrine
Parasympathetic Pathways
*This content will be covered in lecture.
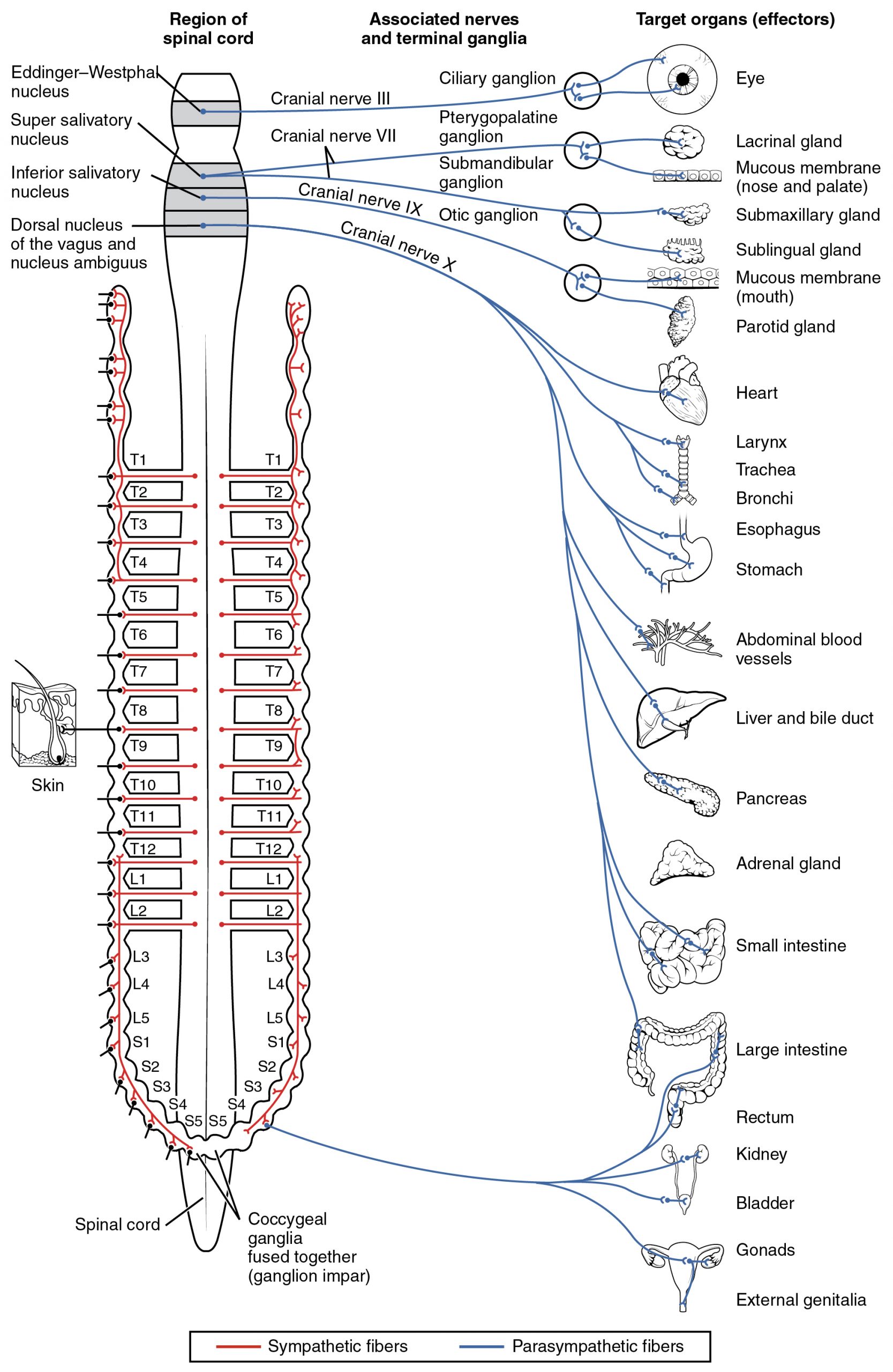
The parasympathetic division of the autonomic nervous system involves neurons that originate in the brainstem and the sacral spinal cord. Preganglionic fibers originating in the brainstem travel through cranial nerves. There are four cranial nerves in which parasympathetic fibers originate. Three of them only send fibers to the head and neck, and we will talk about those in Unit 3 (oculomotor, facial, and glossopharyngeal). The vagus nerve, cranial nerve X, carries parasympathetic fibers to organs of the thorax and abdomen, and we will talk about the vagus nerve extensively in this section. Preganglionic axons from the sacral region originate from the S2-S4 level of the spinal cord. They are called pelvic splanchnic nerves.
We will draw out and discuss the parasympathetic pathways in lecture. Here is a brief summary:
- Vagus Nerve: The vagus nerve provides parasympathetic innervation to the thoracic organs and most of the abdominal organs. Fibers branch along its path to join several different plexuses that travel to specific organs.
- Thorax
- Fibers in the esophageal plexus travel to portions of the esophagus
- Fibers in the cardiac plexus travel to the heart
- Fibers in the pulmonary plexus travel to the lungs and bronchi
- Abdomen
- Fibers in the celiac plexus travel to organs of the foregut (alimentary tract organs from the very inferior esophagus through the first two parts of the duodenum, also the liver, pancreas, and gallbladder)
- Fibers in the superior mesenteric plexus travel to the midgut organs (third part of the duodenum through the first two thirds of the transverse colon)
- Thorax
- Pelvic splanchnic nerves (S2-S4): These nerves supply the distal aspect of the alimentary (digestive) tract and pelvic organs.
- Fibers in the inferior mesenteric plexus travel to the hindgut organs (last two thirds of the transverse colon to the rectum)
- Fibers in the hypogastric plexus travel to pelvic organs, including the bladder and reproductive organs.
Sympathetic Division of the Autonomic Nervous System
*This content will be covered in lecture.
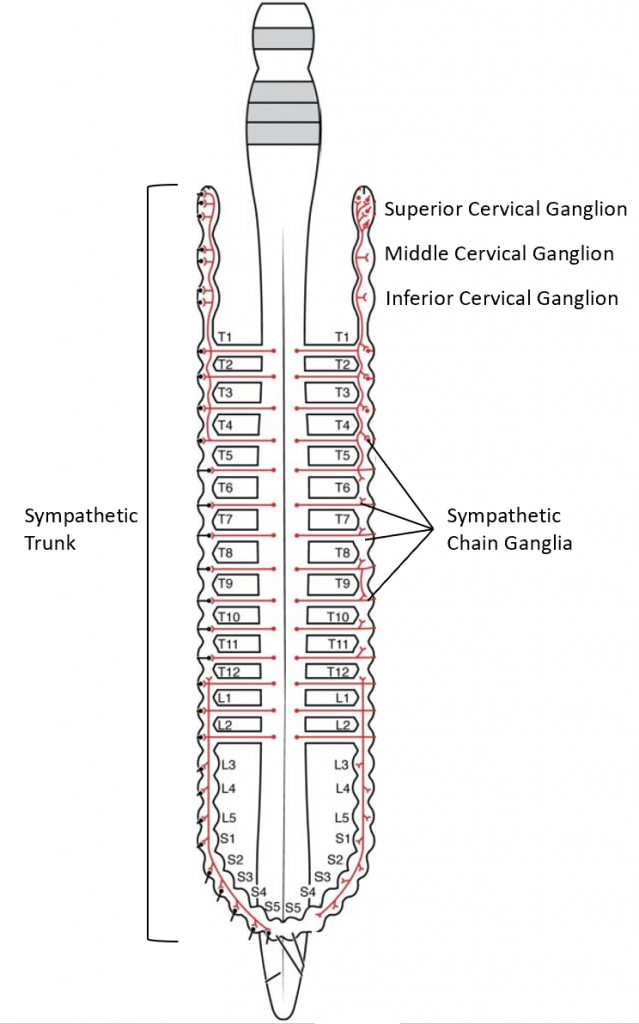
The sympathetic division of the autonomic nervous system involves neurons that originate from the lateral horns of the thoracic and first two lumbar segments of the spinal cord. The majority of ganglia of the sympathetic system belong to a network of sympathetic chain ganglia, located in the sympathetic chain (trunk) that runs alongside the vertebral column. The ganglia appear as swellings along the chain that are connected by groups of axons. The chain is longer than the origin in the thoracic and upper lumbar regions. Three ganglia extend superiorly past the T1 level. They are called the superior, middle, and inferior cervical ganglia. As you can see in the image, they extend alongside the cervical region of the spinal cord, but they are not originating from the cervical region. Instead, the fibers originate in the upper thoracic regions and ascend in the chain to the cervical ganglia. Similarly, the chain extends inferiorly to the sacral levels, and that information originates in the lower thoracic and upper lumbar levels before descending to the sacral levels. Prevertebral ganglia are situated anterior to the vertebral column and receive inputs from splanchnic nerves. They are associated with controlling organs in the abdominal cavity. The three prevertebral ganglia are the celiac ganglion, the superior mesenteric ganglion, and the inferior mesenteric ganglion.
The sympathetic pathways all start the same way. The cell body of the preganglionic neuron is located in the lateral horn of the spinal cord. The preganglionic axon leaves the spinal cord through the ventral root and enters the spinal nerve. From there, the axon leaves the spinal nerve and travels through a branch called the white rami communicantes to reach the sympathetic chain. The white rami communicantes still contains preganglionic axons, and preganglionic axons are myelinated. Mylin is a lipid-based material, and that gives these axons a lighter white-ish appearance. That’s why it is called the white rami communicantes. You can also think of “rami communicantes” as a collection of axons communicating between the spinal nerve and the sympathetic chain.
From there, the pathways differ. Some fibers ascend or descend in the chain, and those are the fibers that appear to be “connecting” the ganglia to form the sympathetic chain. Some axons simply leave the chain after traveling through the white rami communicantes. Some preganglionic axons synapse in the chain ganglia. In just one pathway, after synapsing in the chain ganglia, the postganglionic axons travel back to the spinal nerve through the gray rami communicantes. This is simply a second communication route from the sympathetic chain to the spinal nerve, but in this case it is composed of postganglionic axons, which are unmyelinated. Thus, it is called the gray rami communicantes. Remember that the white rami communicantes travels away from the spinal nerve to the sympathetic chain, while the gray rami communicantes travels from the sympathetic chain back to the spinal nerve. (This is drawn out in lecture.)
There are four sympathetic pathways. We will draw them out and discuss them in lecture. This section will only provide a brief summary:
- Spinal nerve pathway: This pathway follows the path described above, including returning to the spinal nerve via the gray rami communicantes. It is the only pathway that involves the gray rami communicantes! No other pathway has a need to go back to the spinal nerve. This pathway uses the spinal nerve and its branches to get out to its targets in the skin. It innervates the arrector pili muscles, allowing our hair to “stand up,” our sweat glands to increase sweating for heat dissipation, and the blood vessels in our skin, causing vasodilation to cool blood at the surface of the body (heat dissipation).
- Postganglionic sympathetic pathway: After entering the sympathetic chain from thoracic levels T1-T5, these fibers ascend to the middle and inferior cervical ganglia where they synapse. From there they simply exit the sympathetic chain and travel to the following plexuses:
- Fibers in the esophageal plexus travel to portions of the esophagus
- Fibers in the cardiac plexus travel to the heart
- Fibers in the pulmonary plexus travel to the lungs and bronchi
- Splanchnic nerve pathway: Fibers in this pathway originate from the T5-L2 levels. They leave the sympathetic chain in splanchnic nerves that travel to prevertebral ganglia:
- The greater splanchnic nerve (T5-T9) travels to the celiac ganglion. Postganglionic fibers join the celiac plexus and travel to organs of the foregut (alimentary tract organs from the very inferior esophagus through the first two parts of the duodenum, also the liver, pancreas, and gallbladder).
- The lesser splanchnic nerve (T10-T11) travels to the superior mesenteric ganglion. Postganglionic fibers join the superior mesenteric plexus and travel to the midgut organs (third part of the duodenum through the first two thirds of the transverse colon).
- The least splanchnic nerve (T12) sends fibers either to the superior mesenteric ganglion or the inferior mesenteric ganglion. This varies from source to source, so we won’t ask you to decide between the two. Just know that it could go to either of these locations.
- The lumbar splanchnic nerves (L1-L2) travel to the inferior mesenteric ganglion. Postganglionic fibers join the inferior mesenteric plexus and travel to the hindgut organs (last two thirds of the transverse colon to the rectum).
- Sacral splanchnic nerves emerge from the sacral extension of the sympathetic chain. Unlike the other splanchnic nerves, they have their synapse in the sacral sympathetic chain ganglia, and the splanchnic nerves that emerge are postganglionic. They join the hypogastric plexus to innervate pelvic organs.
- Adrenal medulla pathway: This is the only pathway that does not have a ganglion. Instead the axons that originate in the spinal cord travel to the adrenal medulla, the interior portion of the adrenal gland. The adrenal medulla releases the hormone norepinephrine into the bloodstream, using the blood rather than the postganglionic neurons to communicate with target structures.
Adrenal Medulla
The adrenal glands are wedges of glandular and neuroendocrine tissue located directly superior to the kidneys The adrenal glands have a rich blood supply and experience one of the highest rates of blood flow in the body, which makes sense given that they are endocrine glands. The adrenal gland consists of an outer cortex and an inner medulla. The cortex itself is made of glandular tissue divided into three zones: the zona glomerulosa, the zona fasciculata, and the zona reticularis. Each region secretes its own set of hormones. We will not ask you to know the specific hormones secreted by the adrenal cortex in this class, but they are important for the regulation of the long-term stress response, blood pressure and blood volume, nutrient uptake and storage, fluid and electrolyte balance, and inflammation. The adrenal medulla is neuroendocrine tissue that secretes epinephrine and norepinephrine in response to sympathetic stimulation.
Visceral Sensory Information
*This content will be reviewed in lecture.
Technically the autonomic nervous system encompasses motor responses, but it responds to visceral sensory input. Senses associated with the viscera are unconscious. For example, there are specific receptors that sense if there is enough oxygen in your blood, but you do not have a conscious perception of your oxygen levels. If it is too low, that sensory input will eventually cause an increase in your respiratory rate. Though visceral senses are not primarily a part of conscious perception, those sensations sometimes make it to conscious awareness. If a visceral sense is strong enough, it will be perceived. If you swallow a large bolus of food, for instance, you will probably feel the lump of that food as it pushes through your esophagus. As another example, if you inhale especially cold air, you can feel it as it enters your larynx and trachea.
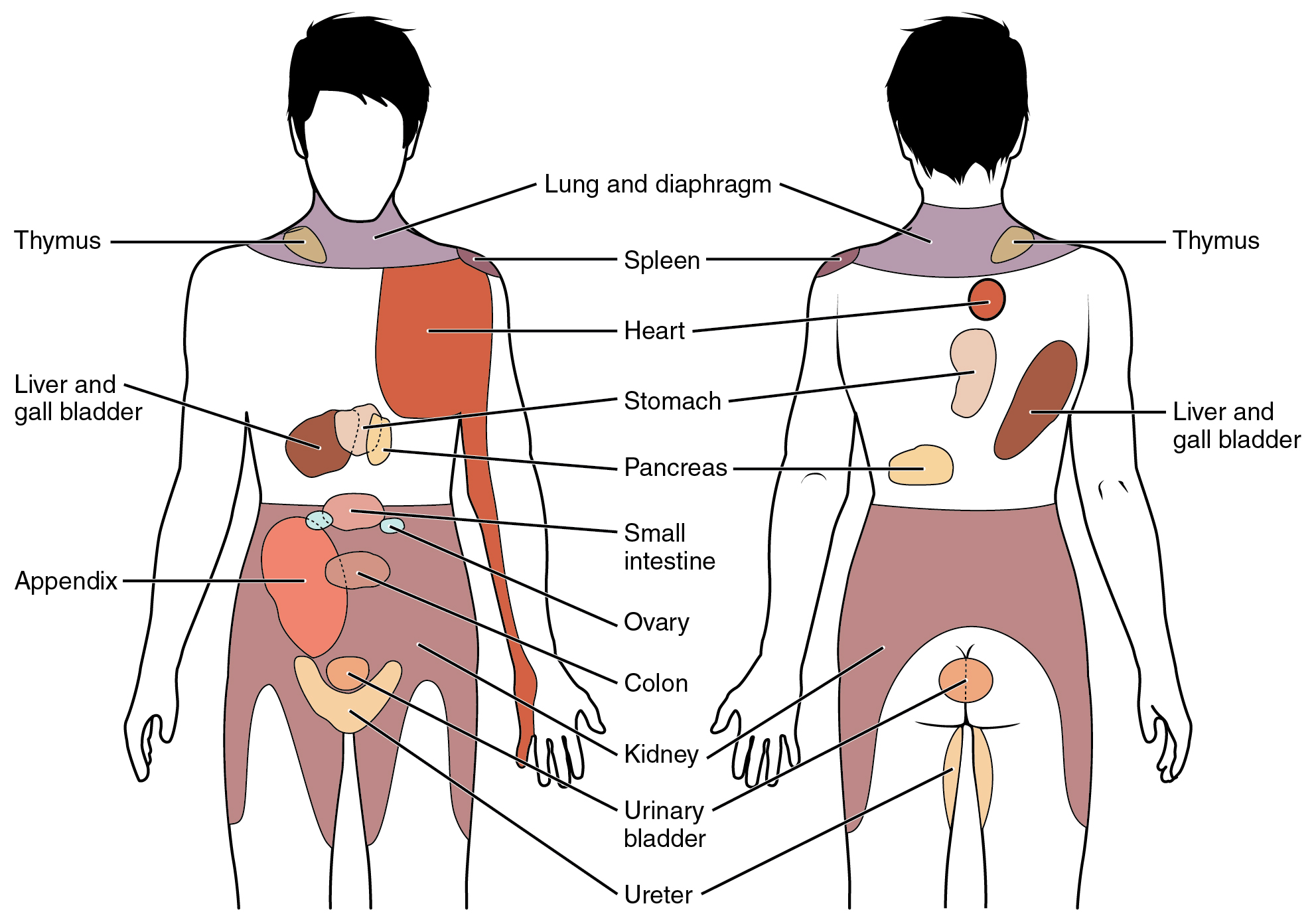
When particularly strong visceral sensations rise to the level of conscious perception, the sensations are often felt in unexpected places. For example, strong visceral sensations of the heart will be felt as pain in the left shoulder and left arm. This irregular pattern of projection of conscious perception of visceral sensations is called referred pain. Depending on the organ system affected, the referred pain will project to different areas of the body. The location of referred pain is not random. The most broadly accepted theory for this phenomenon is that the visceral sensory fibers enter at the same level of the spinal cord as the somatosensory fibers of the referred pain location. The visceral sensory fibers from the area of the heart would enter the spinal cord at the same level as the spinal nerves from the shoulder and arm, so the brain misinterprets the sensations from the heart region as being from the shoulder and arm regions.