Module 4: Integument and Somatosensation
Learning Objectives:
By the end of this module, students will be able to:
- List the functions of the integument.
- Identify the two primary layers of the skin.
- Differentiate the sub-layers of the epidermis.
- Differentiate the sub-layers of the dermis.
- Contrast thin skin and thick skin.
- Summarize the cells of the epidermis.
- List the function of the cells.
- Identify the structures derived from the epidermis.
- Describe the characteristics and function of the structures derived from the epidermis.
- List the sensory receptors of the skin.
- Subdivide the unencapsulated and encapsulated receptors.
- Differentiate the location and primary function of the sensory receptors of the skin.
- Categorize the receptors into the pathways the signals would travel through the spinal cord.
Terms to Know
|
Integument
|
Somatosensation
|
The skin and accessory structures perform a variety of essential functions, such as protecting the body from invasion by microorganisms, chemicals, and other environmental factors; preventing dehydration; acting as a sensory organ; modulating body temperature and electrolyte balance; and synthesizing vitamin D. The underlying hypodermis has important roles in storing fats, forming a “cushion” over underlying structures, and providing insulation from cold temperatures.
Integument Functions
- Protection
- Water regulation
- Temperature regulation
- Vitamin D synthesis
- Sensory perception
- Excretion by secretion (discussed in lecture)
- Storage (discussed in lecture)
- Non-verbal communication (discussed in lecture)
Protection and Water Regulation
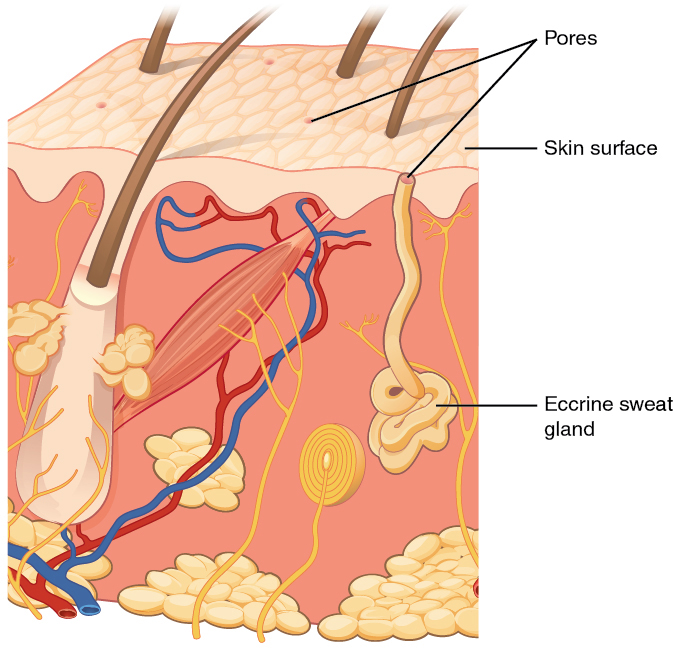
The skin protects the rest of the body from basic elements such as wind, water, and UV sunlight. It acts as a protective barrier against water loss due to layers of keratin and glycolipids in the stratum corneum. It also is the first line of defense against abrasive activity due to contact with grit, microbes, or harmful chemicals. Sweat excreted from sweat glands has antibiotic properties and deters microbes from over-colonizing the skin surface.
Temperature Regulation (Thermoregulation)
The integumentary system helps regulate body temperature through its tight association with the sympathetic nervous system. The sympathetic nervous system is continuously monitoring body temperature and initiating appropriate motor responses. Sweat glands secrete water, salt, and other substances to cool the body when it becomes warm. If the body becomes excessively warm due to high temperatures, vigorous activity, or a combination of the two, sweat glands will be stimulated by the sympathetic nervous system. When the sweat evaporates from the skin surface, the body is cooled as body heat is dissipated. In addition to sweating, arterioles in the dermis dilate so that excess heat carried by the blood can dissipate through the skin and into the surrounding environment.
Fun Fact – Sweat (-> you will not be assessed on this content)
The sympathetic nervous system stimulates sweat glands to produce upwards of 0.7 to 1.5 L of sweat per hour in an active person.
When body temperatures drop, the arterioles constrict to minimize heat loss, particularly in the ends of the digits and tip of the nose. Although the temperature of the skin drops, as a result, passive heat loss is prevented, and internal organs and structures remain warm. If the skin temperature drops too much (such as environmental temperatures below freezing), the conservation of body core heat can result in the skin actually freezing; a condition called frostbite.
Vitamin D Synthesis
The epidermal layer of human skin synthesizes vitamin D when exposed to UV radiation. In the presence of sunlight, a form of vitamin D3 is synthesized in the skin. Vitamin D is essential for the normal absorption of calcium and phosphorous, required for healthy bones. The absence of sun exposure can lead to a lack of vitamin D in the body, leading to a condition called rickets, a painful condition in children where the bones are misshapen due to a lack of calcium, causing bow leggedness. Elderly individuals who suffer from vitamin D deficiency can develop osteomalacia, a softening of the bones. In addition to its essential role in bone health, vitamin D is essential for general immunity against bacterial, viral, and fungal infections. Recent studies are also finding a link between insufficient vitamin D and cancer.
Sensory Perception
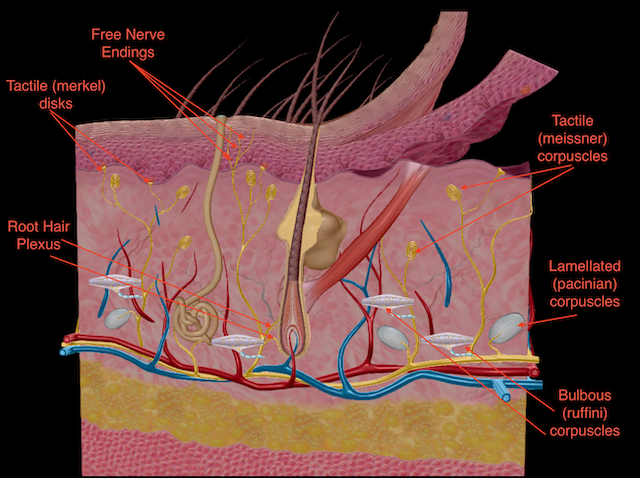
The skin acts as a sense organ because the epidermis, dermis, and hypodermis contain specialized sensory nerve structures that detect touch, surface temperature, and pain. These receptors are more concentrated on the tips of the fingers, which are most sensitive to touch, especially the tactile (Meissner) corpuscle, which responds to light touch, and the lamellated (Pacinian) corpuscle, which responds to deep pressure. Tactile (Merkel) discs, seen scattered in the stratum basale and superficial papillary layer of the dermis, are light-touch receptors, and bulbous (Ruffini) corpuscles found in the dermis and subcutaneous layers are sensitive to deep pressure and skin distortion. In addition to these specialized receptors, there are sensory nerves connected to each hair follicle (root hair plexus), pain and temperature receptors (free nerve endings) scattered throughout the skin, and motor nerves that innervate the arrector pili muscles and glands. This rich innervation helps us sense our environment and react accordingly.
Layers of Skin
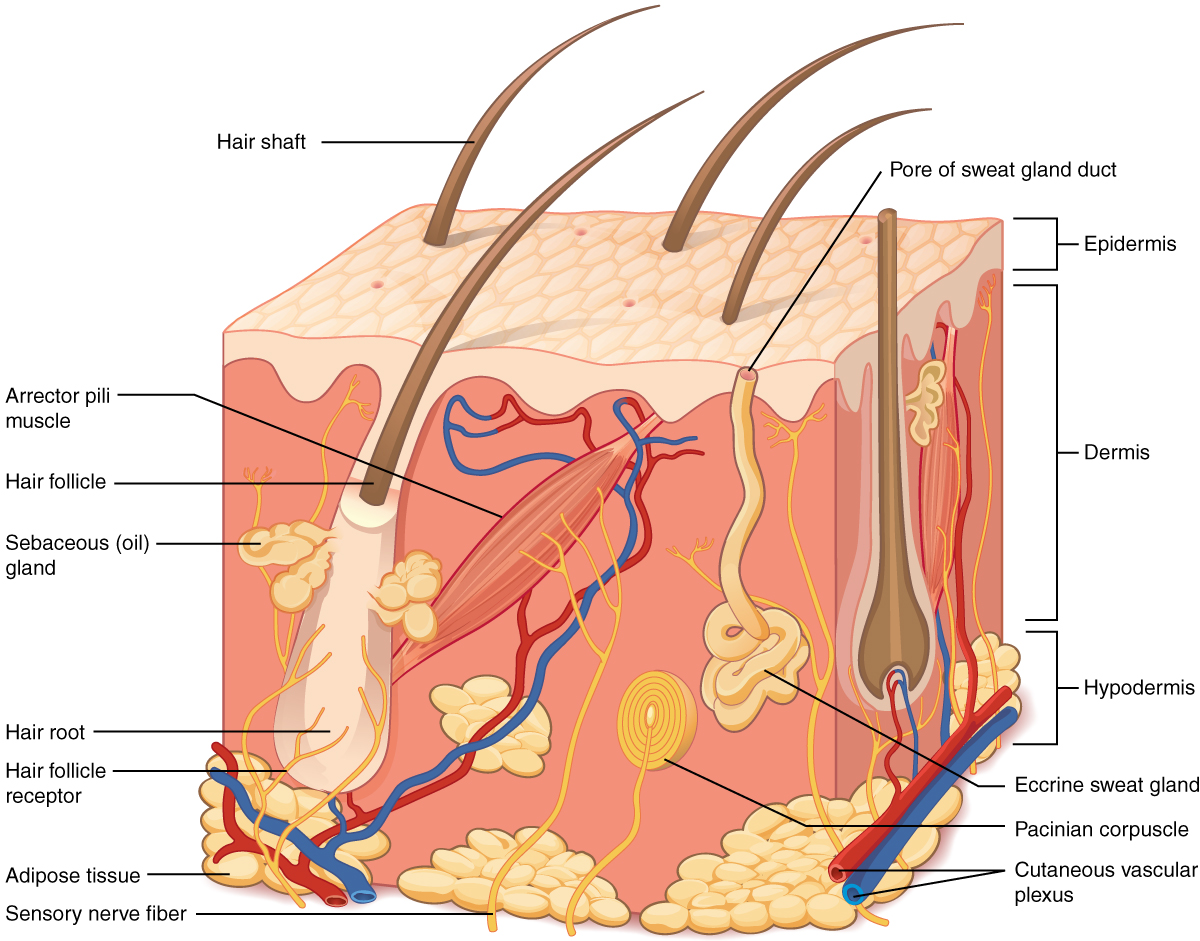
The skin is composed of two main layers: the epidermis, closely packed epithelial cells, and the dermis, made of dense, irregular connective tissue that houses blood vessels, hair follicles, sweat glands, and other structures. Beneath the dermis lies the hypodermis, composed mainly of loose connective and fatty tissues and is not considered a layer of the integument.
The Epidermis
The epidermis is epithelium composed of multiple layers of cells. The basal layer consists of cuboidal cells, whereas the outer layers are squamous, keratinized cells. It is made of four or five layers of epithelial cells, depending on its location in the body. It does not have any blood vessels within it (i.e., it is avascular). Skin that has four layers of cells is referred to as “thin skin.” These layers are the stratum basale, stratum spinosum, stratum granulosum, and stratum corneum from deep to superficial. Most of the skin can be classified as thin skin. “Thick skin” is found only on the palms of the hands and the soles of the feet. It has a fifth layer, called the stratum lucidum, located between the stratum corneum and the stratum granulosum.
The cells in all of the layers except the stratum basale are called keratinocytes. A keratinocyte is a cell that manufactures and stores the protein keratin. Keratin is an intracellular fibrous protein that gives hair, nails, and skin their hardness and water-resistant properties. The keratinocytes in the stratum corneum are dead and regularly slough away, being replaced by cells from the deeper layers.
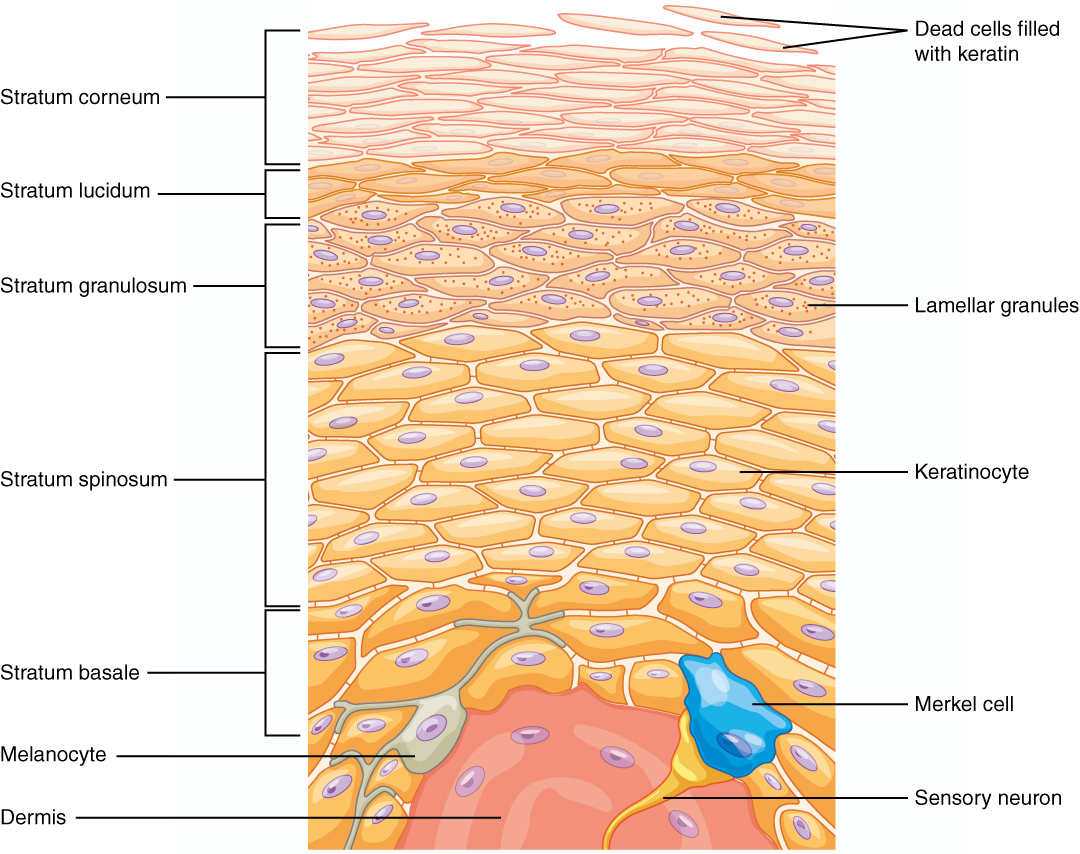
Stratum Basale
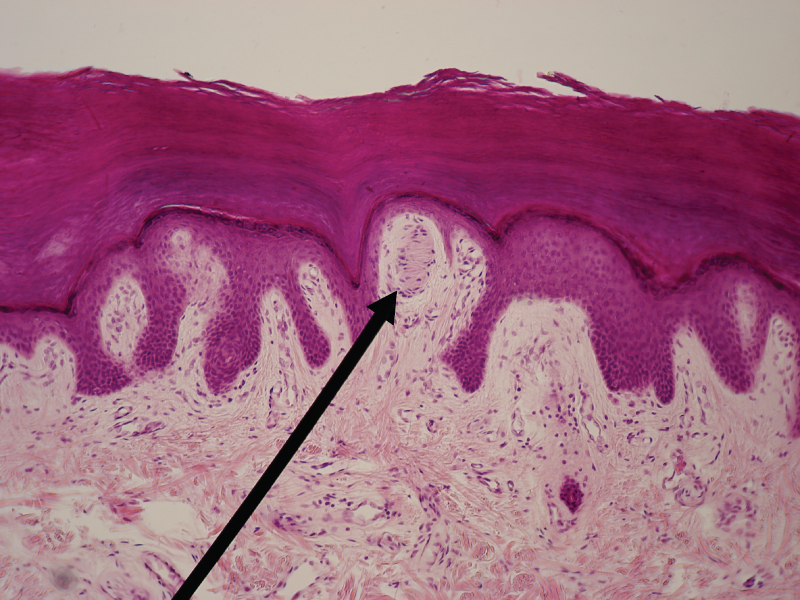
The stratum basale is the deepest epidermal layer and attaches the epidermis to the basal lamina, below which lie the layers of the dermis. The cells in the stratum basale bond to the dermis via intertwining collagen fibers referred to as the basement membrane. A finger-like projection or fold, known as the dermal papilla (plural = dermal papillae), is found in the superficial portion of the dermis. Dermal papillae increase the strength of the connection between the epidermis and dermis; the greater the folding, the stronger the connections.
The stratum basale is a single layer of cells primarily made of basal cells. A basal cell is a cuboidal-shaped stem cell that is a precursor of the keratinocytes of the epidermis. All of the keratinocytes are produced from this single layer of cells, which are constantly going through mitosis to produce new cells. As new cells are formed, the existing cells are pushed superficially away from the stratum basale. Two other cell types are found dispersed among the basal cells in the stratum basale. The first is a tactile (Merkel) cell responsible for stimulating sensory nerves that the brain perceives as touch. These cells are especially abundant on the surfaces of the hands and feet. The second is a melanocyte, a cell that produces the pigment melanin. Melanin gives hair and skin its color and helps protect the epidermis’ living cells from ultraviolet (UV) radiation damage.
Stratum Spinosum
As the name suggests, the stratum spinosum is spiny due to the protruding cell processes that join the cells via a structure called a desmosome. The desmosomes interlock with each other and strengthen the bond between the cells. The stratum spinosum is composed of eight to 10 layers of keratinocytes, formed as a result of cell division in the stratum basale. Interspersed among the keratinocytes of this layer are dendritic (Langerhans) cells, which function as macrophages by engulfing bacteria, foreign particles, and damaged cells that occur in this layer.
The keratinocytes in the stratum spinosum begin the synthesis of keratin and release a water-repelling glycolipid that helps prevent water loss from the body, making the skin relatively waterproof. As new keratinocytes are produced atop the stratum basale, the keratinocytes of the stratum spinosum are pushed into the stratum granulosum.
Stratum Granulosum
The stratum granulosum has a grainy appearance due to further changes to the keratinocytes as they are pushed from the stratum spinosum. The cells (three to five layers deep) become flattened in this layer. Their cell membranes thicken, and they generate large amounts of the proteins keratin, which is fibrous, and keratohyalin, which accumulates lamellar granules within the cells. These two proteins make up the bulk of the keratinocyte mass in the stratum granulosum and give the layer its grainy appearance. The nuclei and other cell organelles disintegrate as the cells die, leaving behind the keratin, keratohyalin, and cell membranes to form the stratum lucidum, the stratum corneum, and the accessory structures of hair and nails.
Stratum Lucidum
The stratum lucidum is a smooth, seemingly translucent layer of the epidermis located just above the stratum granulosum and below the stratum corneum. This thin layer of cells is found only in the thick skin of the palms, soles, and digits. The keratinocytes that compose the stratum lucidum are dead and flattened. These cells are densely packed, which gives these cells their transparent (i.e., lucid) appearance and provides a water barrier.
Stratum Corneum
The stratum corneum is the most superficial layer of the epidermis and is exposed to the outside environment. The increased keratinization of the cells in this layer gives it its name. There are usually 15 to 30 layers of dead cells in the stratum corneum. This dry, dead layer helps prevent the penetration of microbes and the dehydration of underlying tissues and provides mechanical protection against abrasion for the more delicate, underlying layers. Cells in this layer are shed periodically and are replaced by cells pushed up from the stratum granulosum (or stratum lucidum in the palms and soles of feet). The entire layer is replaced during a period of about 4 weeks.
Dermis
The dermis might be considered the “core” of the integumentary system (derma- = “skin”), as distinct from the epidermis (epi- = “upon” or “over”) and hypodermis (hypo- = “below”). It contains blood and lymph vessels, nerves, and other structures, such as hair follicles and sweat glands. The dermis comprises two layers of connective tissue that compose an interconnected mesh of elastin and collagenous fibers produced by fibroblasts.
Layers of the Dermis
This stained slide shows the two components of the dermis—the papillary layer and the reticular layer. Both are made of connective tissue with fibers of collagen extending from one to the other, making the border between the two somewhat indistinct. The dermal papillae extending into the epidermis belong to the papillary layer, whereas the dense collagen fiber bundles below belong to the reticular layer.
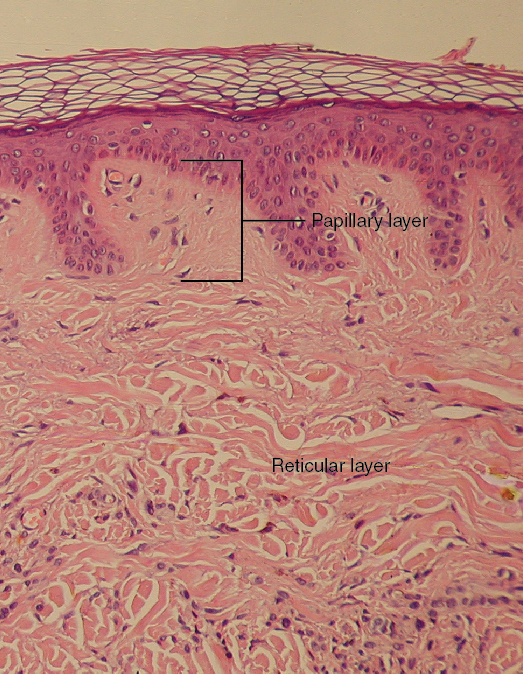
Papillary Layer
The papillary layer is made of loose, areolar connective tissue, which means the collagen and elastin fibers of this layer form a loose mesh. This superficial layer of the dermis projects into the stratum basale of the epidermis to form finger-like dermal papillae. Within the papillary layer are fibroblasts, a small number of fat cells (adipocytes), and an abundance of small blood vessels. Also, the papillary layer contains phagocytes, defensive cells that help fight bacteria or other infections that have breached the skin. This layer also contains lymphatic capillaries, nerve fibers, and touch receptors called the tactile (Meissner) corpuscles.
Reticular Layer
Underlying the papillary layer is the much thicker reticular layer, composed of dense, irregular connective tissue. This layer is well vascularized and has a rich sensory and sympathetic nerve supply. The reticular layer appears reticulated (net-like) due to a tight meshwork of fibers. Elastin fibers provide some elasticity to the skin, enabling movement. Collagen fibers provide structure and tensile strength, with strands of collagen extending into both the papillary layer and the hypodermis. Also, collagen binds water to keep the skin hydrated.
Hypodermis
The hypodermis (also called the subcutaneous layer or superficial fascia) is directly below the dermis. It connects the skin to the underlying fascia (fibrous tissue) of the bones and muscles. It is not strictly a part of the skin, although the hypodermis and dermis border can be difficult to distinguish. The hypodermis consists of well-vascularized, loose, areolar connective tissue and adipose tissue, which functions as a mode of fat storage and provides insulation and cushioning for the integument.
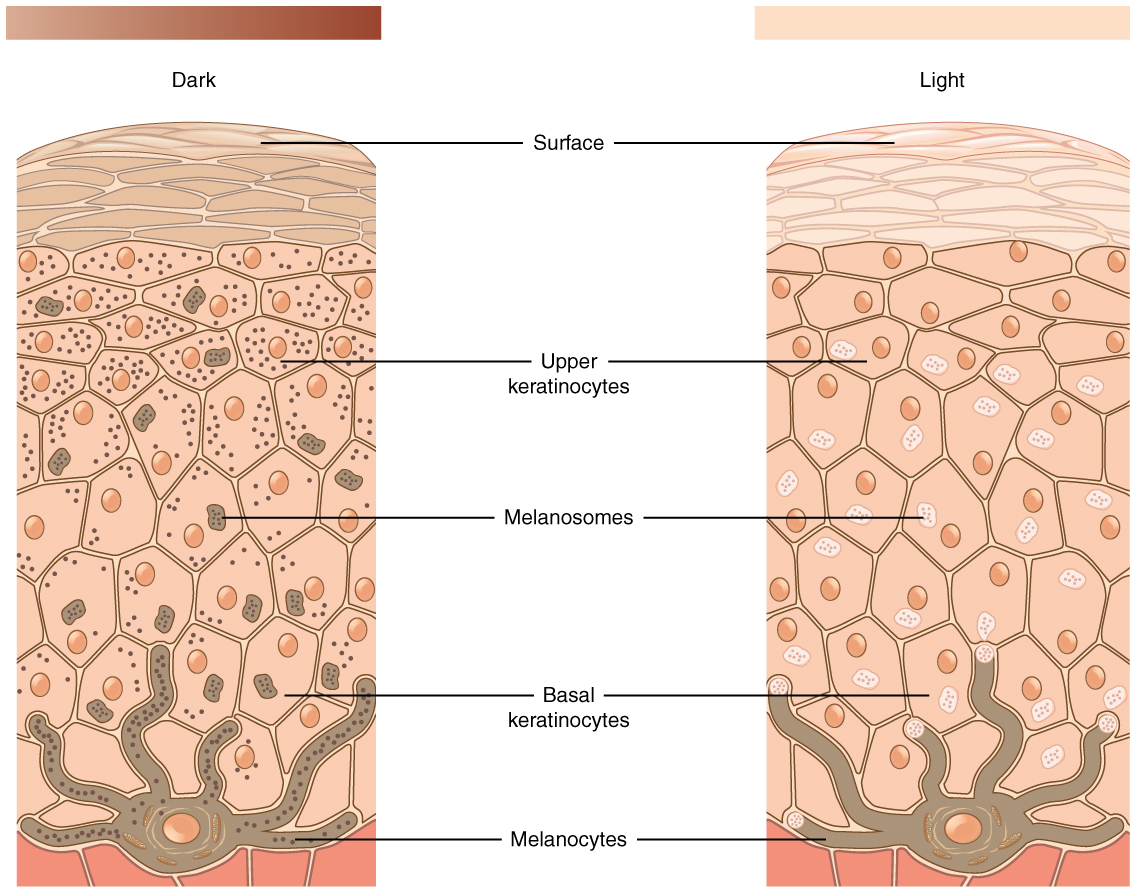
Pigmentation
The skin color is influenced by several pigments, including melanin, carotene, and hemoglobin. Recall that melanin is produced by cells called melanocytes, scattered throughout the epidermis’ stratum basale. The melanin is transferred into the keratinocytes via a cellular vesicle called a melanosome. The skin’s relative coloration depends on the amount of melanin produced by melanocytes in the stratum basale and taken up by keratinocytes.
Melanin – FYI (For Your Information -> you will not be assessed on this content)
Melanin occurs in two forms
- Eumelanin
-
- black and brown
- Pheomelanin
- red shades
Exposure to UV rays causes melanin to be manufactured at higher rates to protect the DNA of epidermal cells.
- Melanin synthesis peaks ~ 10 days after the initial sun exposure. Thus why pale-skinned individuals are more likely to suffer sunburns.
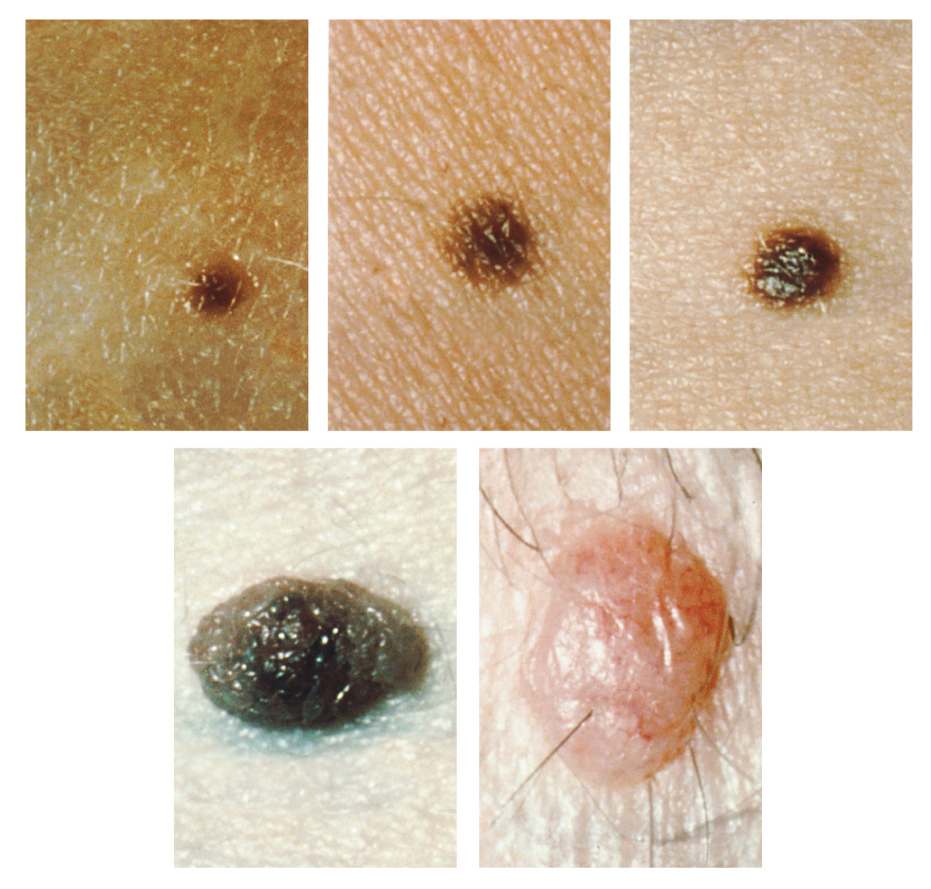
Melanosomes are temporary structures that are eventually destroyed by fusion with lysosomes; this fact, along with melanin-filled keratinocytes in the stratum corneum sloughing off, makes tanning impermanent. Too much sun exposure can eventually lead to wrinkling due to the destruction of the skin’s cellular structure, and in severe cases, can cause sufficient DNA damage to result in skin cancer. When there is an irregular accumulation of melanocytes in the skin, freckles appear. Moles are larger masses of melanocytes, and although most are benign, they should be monitored for changes that might indicate the presence of cancer (see ABCDE of skin cancer PSA in the lecture videos).
Moles
Accessory Structures
Accessory structures of the skin include hair, nails, sweat glands, and sebaceous glands. These structures embryologically originate from the epidermis and can extend down through the dermis into the hypodermis.
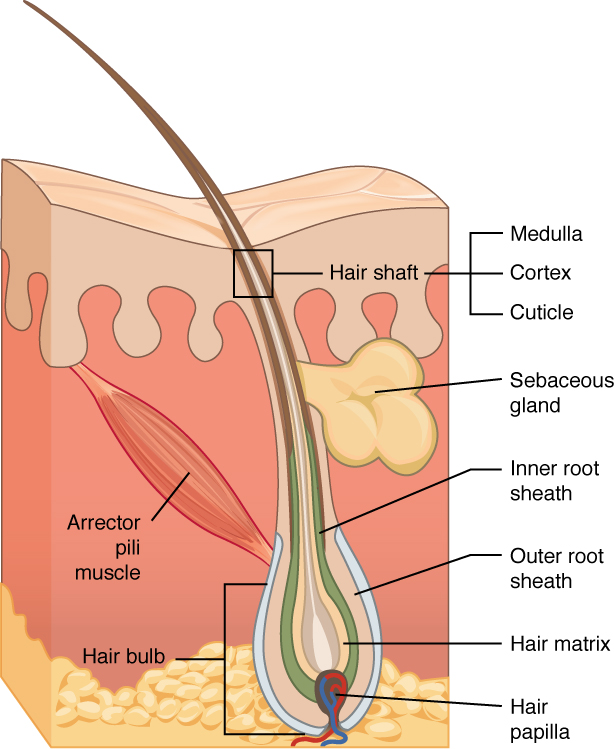
Hair
Hair is a keratinous filament growing out of the epidermis. It is primarily made of dead, keratinized cells. Strands of hair originate in an epidermal penetration of the dermis called the hair follicle. The hair shaft is the part of the hair not anchored to the follicle, and much of this is exposed at the skin’s surface. The rest of the hair, which is anchored in the follicle, lies below the surface of the skin and is referred to as the hair root. The hair root ends deep in the dermis at the hair bulb and includes a layer of mitotically active basal cells called the hair matrix. The hair bulb surrounds the hair papilla, which is made of connective tissue and contains blood capillaries and nerve endings from the dermis.
Fun Fact – Hair (-> you will not be assessed on this content)
Just as the basal layer of the epidermis forms the layers of epidermis that get pushed to the surface as the dead skin on the surface sheds, the basal cells of the hair bulb divide and push cells outward in the hair root and shaft as the hair grows. The medulla forms the central core of the hair, which is surrounded by the cortex, a layer of compressed, keratinized cells covered by an outer layer of very hard, keratinized cells known as the cuticle. Hair growth begins with the production of keratinocytes by the basal cells of the hair bulb. As new cells are deposited at the hair bulb, the hair shaft is pushed through the follicle toward the surface. Keratinization is completed as the cells are pushed to the skin surface to form the shaft of hair that is externally visible. The external hair is completely dead and composed entirely of keratin. For this reason, our hair does not have sensation. Furthermore, you can cut your hair or shave without damaging the hair structure because the cut is superficial.
Hair serves a variety of functions, including protection, sensory input, thermoregulation, and communication. For example, the hair on the head protects the skull from the sun. The hair in the nose and ears and around the eyes (eyelashes) defends the body by trapping and excluding dust particles that may contain allergens and microbes. Hair of the eyebrows prevents sweat and other particles from dripping into and bothering the eyes. Hair also has a sensory function due to sensory innervation by a hair root plexus surrounding each hair follicle’s base. Hair is extremely sensitive to air movement or other environmental disturbances, much more so than the skin surface. This feature is also useful for detecting the presence of insects or other potentially damaging substances on the skin surface. Each hair root is connected to a smooth muscle called the arrector pili that contracts in response to nerve signals from the sympathetic nervous system, making the external hair shaft “stand up.”
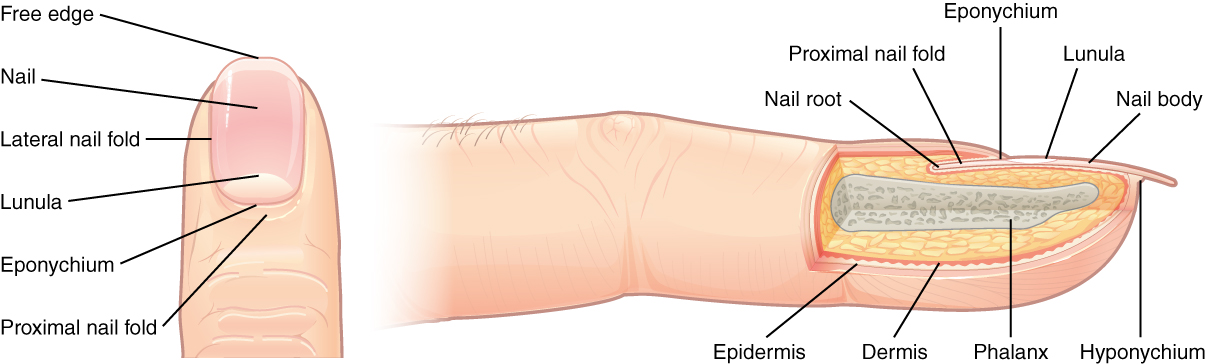
Nails
The nail bed is a specialized structure of the epidermis found at the tips of our fingers and toes. The nail body is formed on the nail bed and protects the tips of our fingers and toes as they are the farthest extremities and the parts of the body that experience the maximum mechanical stress. Also, the nail body forms a back-support for picking up small objects with the fingers. The nail body is composed of densely packed dead keratinocytes. The epidermis in this part of the body has evolved a specialized structure upon which nails can form. The nail body forms at the nail root, which has a matrix of proliferating cells from the stratum basale that enables the nail to grow continuously. The lateral nail fold overlaps the nail on the sides, helping to anchor the nail body. The nail fold that meets the proximal end of the nail body forms the nail cuticle, also called the eponychium. The nail bed is rich in blood vessels, making it appear pink, except at the base, where a thick layer of epithelium over the nail matrix forms a crescent-shaped region called the lunula (the “little moon”). The area beneath the nail’s free edge, furthest from the cuticle, is called the hyponychium. It consists of a thickened layer of stratum corneum.
Sweat Glands
When the body becomes warm, sweat glands produce sweat to cool the body. There are two types of sweat glands, each secreting slightly different products.
An eccrine sweat gland is a type of gland that produces a hypotonic sweat for thermoregulation. These glands are found all over the skin’s surface but are especially abundant on the palms of the hand, the soles of the feet, and the forehead. They are coiled glands lying deep in the dermis, with the duct rising to a pore on the skin surface, where the sweat is released. This type of sweat, released by exocytosis, is hypotonic and composed mostly of water, with some salt, antibodies, traces of metabolic waste, and dermicidin, an antimicrobial peptide. Eccrine glands are a primary component of thermoregulation in humans and thus help to maintain homeostasis.
An apocrine sweat gland is usually associated with hair follicles in densely hairy areas, such as armpits and genital regions. Apocrine sweat glands are larger than eccrine sweat glands and lie deeper in the dermis, sometimes even reaching the hypodermis, with the duct normally emptying into the hair follicle. In addition to water and salts, apocrine sweat includes organic compounds that make the sweat thicker and subject to bacterial decomposition and subsequent smell. The release of this sweat is under both nervous and hormonal control and plays a role in the poorly understood human pheromone response.
Sebaceous Glands
A sebaceous gland is a type of oil gland found all over the body and helps to lubricate and waterproof the skin and hair. Most sebaceous glands are associated with hair follicles. They generate and excrete sebum, a mixture of lipids, onto the skin surface, thereby naturally lubricating the dry and dead layer of keratinized cells of the stratum corneum, keeping it pliable. The fatty acids of sebum also have antibacterial properties and prevent water loss from the skin in low-humidity environments. The secretion of sebum is stimulated by hormones, many of which do not become active until puberty. Thus, sebaceous glands are relatively inactive during childhood.
Aging and the Integumentary System
All systems in the body accumulate subtle and some not-so-subtle changes as a person ages. Among these changes are reductions in cell division, metabolic activity, blood circulation, hormonal levels, and muscle strength. In the skin, these changes are reflected in decreased mitosis in the stratum basale, leading to a thinner epidermis. The dermis, which is responsible for the skin’s elasticity and resilience, exhibits a reduced ability to regenerate, leading to slower wound healing. With its fat stores, the hypodermis loses structure due to the reduction and redistribution of fat, which in turn contributes to the thinning and sagging of skin.
The accessory structures also have lowered activity, generating thinner hair and nails, and reduced sebum and sweat. A reduced sweating ability can cause some elderly to be intolerant to extreme heat. Other cells in the skin, such as melanocytes and dendritic cells, also become less active, leading to a paler skin tone and lowered immunity. Wrinkling of the skin occurs due to the breakdown of its structure, resulting from decreased collagen and elastin production in the dermis, weakening of muscles lying under the skin, and the skin’s inability to retain adequate moisture.
Somatosensation (Touch)
Somatosensation is considered a general sense, as opposed to the special senses discussed in this section. Somatosensation is the group of sensory modalities that are associated with touch, proprioception, and interoception. These modalities include pressure, vibration, light touch, tickle, itch, temperature, pain, proprioception, and kinesthesia. This means that its receptors are not associated with a specialized organ, but are instead spread throughout the body in a variety of organs. Many of the somatosensory receptors are located in the skin, but receptors are also found in muscles, tendons, joint capsules, ligaments, and the walls of visceral organs.
Two types of somatosensory signals that are transduced by free nerve endings are pain and temperature. These two modalities use thermoreceptors and nociceptors to transduce temperature and pain stimuli, respectively. Temperature receptors are stimulated when local temperatures differ from body temperature. Some thermoreceptors are sensitive to just cold and others to just heat. Nociception is the sensation of potentially damaging stimuli. Mechanical, chemical, or thermal stimuli beyond a set threshold will elicit painful sensations. Stressed or damaged tissues release chemicals that activate receptor proteins in the nociceptors. Free nerve endings are found in the papillary layer of the dermis and the deep epidermis.
If you drag your finger across a textured surface, the skin of your finger will vibrate, providing information about light touch. Light touch is sensed by mechanoreceptors called tactile (Merkel) cells and tactile (Meissner) corpuscles. Tactile (Merkel) cells are located in the stratum basale of the epidermis. Tactile cells make up part of the tactile (Merkel) disc that exists at the epidermal-dermal junction. Tactile (Meissner) corpuscles are located in the dermis. Deep pressure and high-frequency vibration is transduced by lamellated (Pacinian) corpuscles, which are receptors with encapsulated endings found deep in the dermis, or subcutaneous tissue. Hair follicles are also wrapped in a plexus of nerve endings known as the root hair plexus. These nerve endings detect the movement of hair at the surface of the skin, such as when an insect may be walking along the skin. Stretching of the skin and deep, continuous pressure is transduced by stretch receptors known as bulbous (Ruffini) corpuscles. Other somatosensory receptors are found in the joints and muscles. Stretch receptors monitor the stretching of tendons, muscles, and the components of joints.
| Mechanoreceptors of Somatosensation | |||
|---|---|---|---|
| Name | Historical (eponymous) name | Location(s) | Stimuli |
| Free nerve endings | * | Deep epidermis and the papillary layer of dermis, cornea, tongue, joint capsules, visceral organs | Pain, temperature, mechanical deformation |
| Tactile discs | Merkel’s discs | Tactile cell = epidermis, Tactile disc = Epidermal–dermal junction, mucosal membranes | Light touch (Low-frequency vibration (5–15 Hz)) |
| Bulbous corpuscle | Ruffini’s corpuscle | Dermis, joint capsules | Continuous deep pressure, skin distortion |
| Tactile corpuscle | Meissner’s corpuscle | Papillary dermis, especially in the fingertips and lips | Light touch (Low-frequency vibrations below 50 Hz) |
| Lamellated corpuscle | Pacinian corpuscle | Deep dermis, subcutaneous tissue | Deep pressure, high-frequency vibration (around 250 Hz) |
| Root hair plexus | * | Wrapped around hair follicles in the dermis | Movement of hair (light touch) |
| Muscle spindle | * | In line with skeletal muscle fibers | Muscle contraction and stretch |
| Golgi tendon organ | * | In line with tendons | Stretch of tendons |
Unencapsulated Tactile Receptors
Unencapuslated tactile receptors are not wrapped in myelin or a modified myelin sheath. These include:
- Free Nerve Endings
- Tactile (Merkel) discs
- Root Hair Plexus
Encapsulated Tactile Receptors
Encapsulated tactile receptors are wrapped in a modified myelin sheath. These receptors include:
- Tactile (Meissner) corpuscles
- Lamellated (Pacinian) corpuscles
- Bulbous (Ruffini) corpuscles

