Module 14: Digestive System I – Alimentary Tract
Learning Objectives:
By the end of this class, students will be able to:
- Describe the organ quadrant system and nine region system for dividing the abdominal cavity.
- Describe the peritoneum and mesenteries.
- Analyze and describe the functions of the digestive system.
- Explain the histology of the GI tract wall.
- Explain the anatomy of the esophagus and stomach.
- Describe the anatomy of the small intestines and large intestines.
Terms to Know
|
Abdominal Cavity Quadrants
Peritoneum
Development
Histological Organization
General
|
Esophagus
Stomach
Small Intestine
Large Intestine
Vasculature
*Covered only in lecture, not in this text |
Abdominal Regions and Quadrants
This will be covered in lecture.
To promote clear communication, such as about the location of a patient’s abdominal pain or a suspicious mass, health care providers divide up the cavity into either nine regions or four quadrants. You should know the names of the regions and quadrants as labeled in the image below. For the nine-region system, we will ask you about the name and the location of the regions, but we won’t ask you which organs are located specifically in which regions. For the quadrant system, we will ask you about the quadrant that an organ is primarily located in.
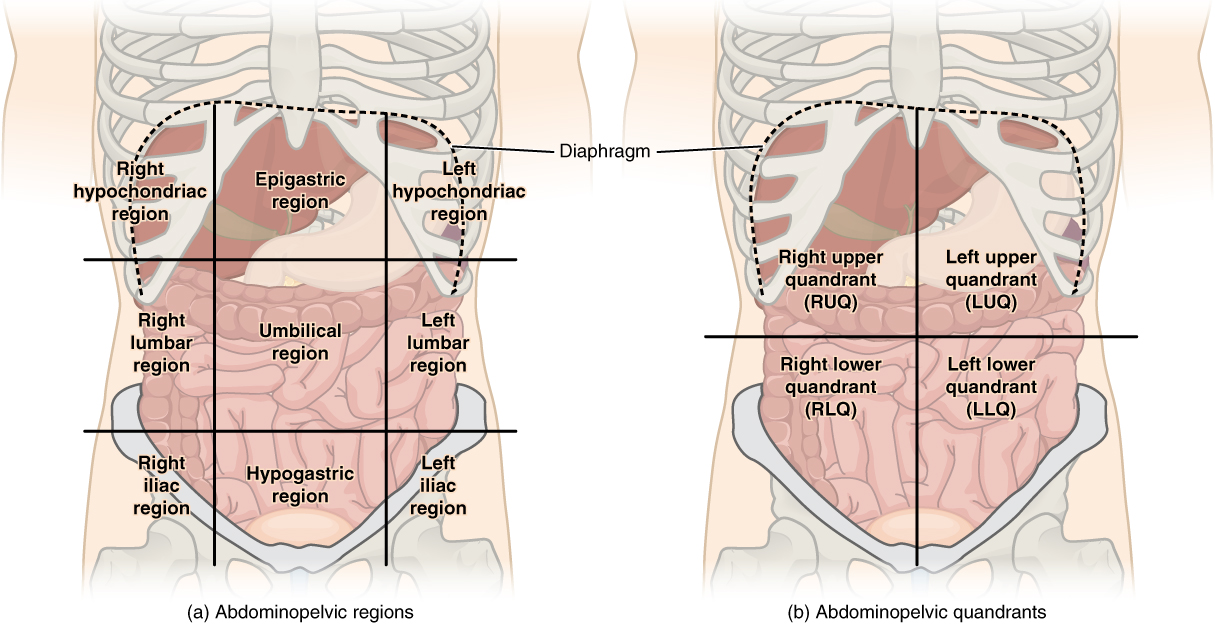
The more detailed regional approach subdivides the cavity with one horizontal line immediately inferior to the ribs and one immediately superior to the pelvis, and two vertical lines drawn as if dropped from the midpoint of each clavicle (collarbone). There are nine resulting regions. The simpler quadrants approach, which is more commonly used in medicine, subdivides the cavity with one horizontal and one vertical line that intersect at the patient’s umbilicus (navel).
The Peritoneum and Mesentery
This content is primarily covered in the reading and assignment as self-study. It will be only briefly reviewed in lecture.
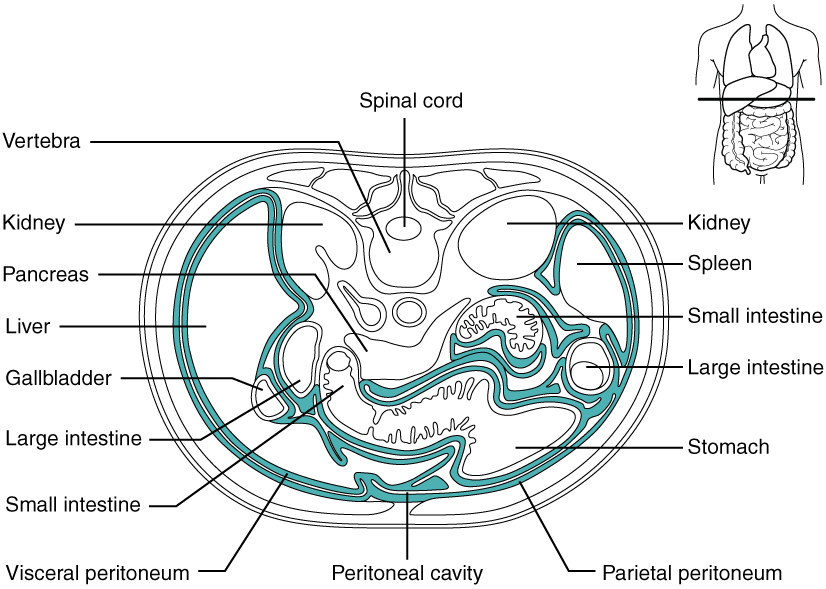
The digestive organs within the abdominopelvic cavity are held in place by the peritoneum, a broad membranous sac made up of simple squamous epithelial tissue surrounded by connective tissue. The peritoneum is similar to the pleura surrounding the lungs and the pericardium surrounding the heart. The parietal peritoneum is the outer layer that primarily lines the wall of the abdominopelvic cavities. The visceral peritoneum is the inner layer that lines most organs abdominopelvic cavity. The visceral and parietal peritoneum are continuous with each other, and they enclose the peritoneal cavity. The organs are surrounded by, but not within, the peritoneal cavity. The peritoneal cavity contains few milliliters of watery fluid and acts as a lubricant to reduce friction between the abdominal and pelvic organs and the body wall that could lead to inflammation of the organs. The visceral peritoneum includes multiple large folds that envelope various abdominal organs, holding them to the dorsal surface of the body wall. Within these folds are blood vessels, lymphatic vessels, and nerves that innervate the organs with which they are in contact, supplying their adjacent organs. The five major peritoneal folds are described in the table below.
| The Five Major Peritoneal Folds | |
|---|---|
| Fold | Description |
| Greater omentum | Apron-like pouch extending inferiorly between the body wall and the anterior surface of the small intestine |
| Falciform ligament | Anchors the liver to the anterior abdominal wall and inferior border of the diaphragm |
| Lesser omentum | Suspends the stomach from the inferior border of the liver |
| Mesentery Proper | Vertical band of tissue anterior to the lumbar vertebrae and anchoring most of the small intestine |
| Mesocolon | Attaches the large intestine (the transverse and sigmoid colon) to the posterior abdominal wall |
Not all organs are surrounded by peritoneum, and that has to do with how they develop. There are three categories of organs based on their relationship to the peritoneum:
- Intraperitoneal: These organs are surrounded by peritoneum in development and remain so in adulthood. Examples include the stomach and liver.
- Retroperitoneal: The organs are against the posterior body wall and are not surrounded by peritoneum.
- Primarily retroperitoneal: These organs are never surrounded by peritoneum, not in development nor in adulthood. An example is the kidneys.
- Secondarily retroperitoneal: These organs are originally surrounded by peritoneum, but during development they are pushed out from the peritoneum and against the posterior body wall. Examples include the pancreas and duodenum.
Introduction to the digestive system
This content is primarily covered in the reading and assignment as self-study. It will be only briefly reviewed in lecture.
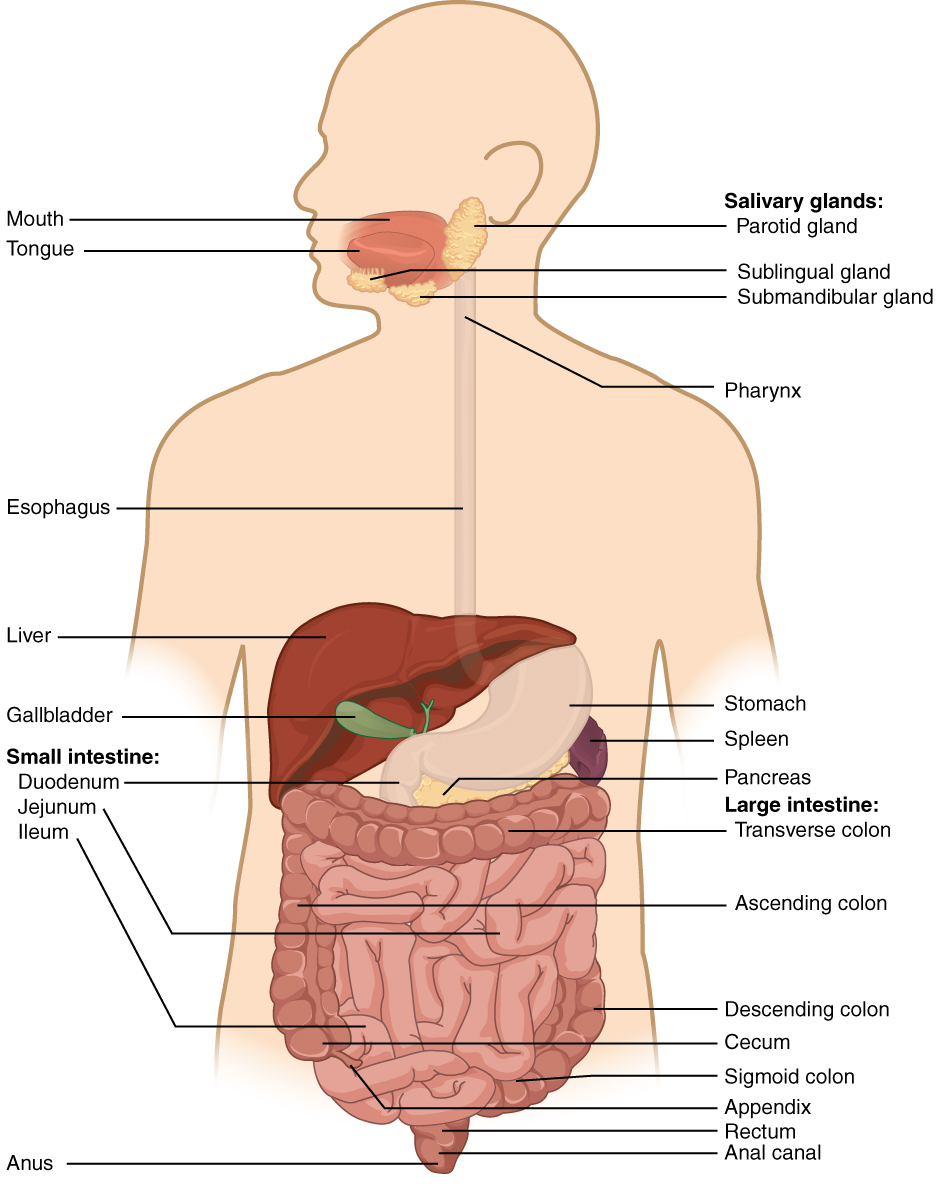
The digestive system consists of organs spanning the head and neck to the pelvic cavity. Food passes through some of these organs, where it is broken down, digested, and absorbed, then wastes are compacted and excreted. These organs are part of the alimentary canal, or digestive tract. Other organs assist with digestion by mechanically breaking down food or secreting chemicals that break down food through chemical digestion. The organs of the digestive system are listed here, though we will only talk about the organs located in the thorax, abdomen, and pelvis in this unit. Organs located in the head and neck will be covered in Unit 3.
- Alimentary canal organs: organs of the digestive tract that food substance passes through. It is a one-way tube about 25 feet in length.
- Oral cavity (covered in Unit 3)
- Pharynx (covered in Unit 3)
- Esophagus
- Stomach
- Small intestines
- Large intestines
- Accessory digestive organs: organs critical for the breakdown of food, but the food does not pass through them.
- Teeth (covered in Unit 3)
- Tongue (covered in Unit 3)
- Salivary glands (covered in Unit 3)
- Gallbladder
- Liver
- Pancreas
Histology of the Alimentary Canal
This content is primarily covered in the reading and assignment as self-study.
Throughout its length, the alimentary tract is composed of the same four tissue layers.
- Mucosa: a mucous membrane consisting of three layers:
- Epithelium: in direct contact with ingested food. Interspersed among its epithelial cells are goblet cells, which secrete mucus and fluid into the lumen. The type of epithelium differs by location, and we will discuss this in detail below and in lecture.
- Lamina propria: a layer of areolar connective tissue deep to the epithelium that contains blood and lymphatic vessels as well as mucosa-associated lymphatic tissue (MALT) to respond to foodborne bacteria and foreign matter in the alimentary canal.
- Muscularis mucosa: a thin, smooth muscle layer that creates folds in the stomach and intestines, increasing the surface area for digestion and absorption.
- Submucosa: lies immediately beneath the mucosa. A broad layer of dense connective tissue, it connects the overlying mucosa to the underlying muscularis.
- Muscularis: made up of a double layer of smooth muscle in most locations: an inner circular layer and an outer longitudinal layer. The contractions of these layers promote mechanical digestion and move the food along the canal. The stomach is equipped for its churning function by the addition of a third layer, the oblique muscle.
- Serosa: superficial to the muscularis of alimentary canal organs in the abdominal cavity. It consists of a layer of visceral peritoneum overlying a layer of loose connective tissue. When an organ is retroperitoneal, the organ is surrounded by an adventitia rather than a serosa.
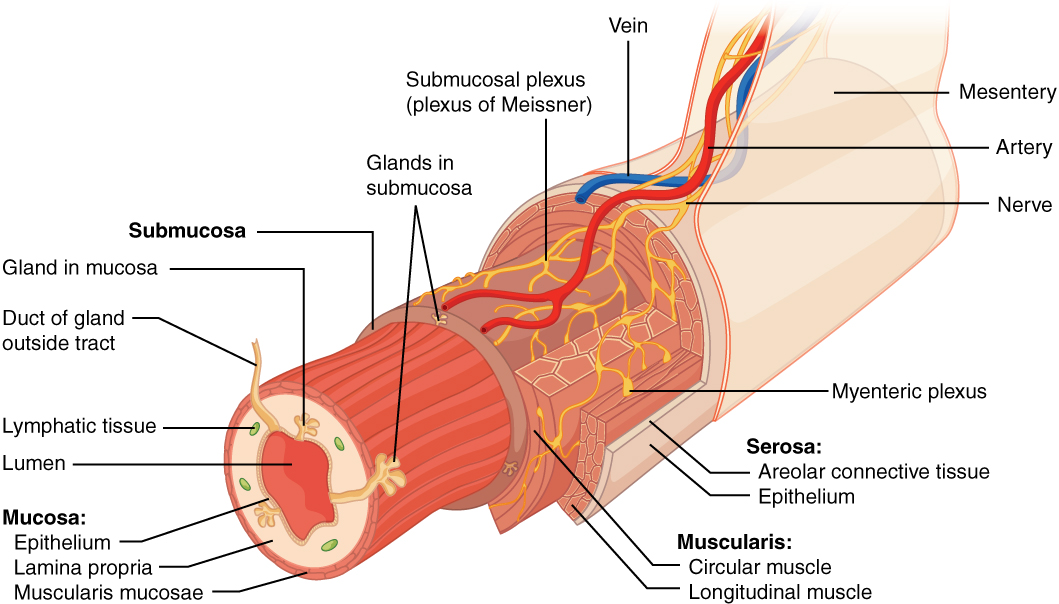
The walls of the alimentary canal contain a variety of sensors that help regulate digestive functions. Much of the alimentary canal receives local innervation from the enteric nervous system, which runs from the esophagus to the anus, and contains approximately 100 million motor, sensory, and interneurons. The myenteric plexus (plexus of Auerbach) lies in the muscularis layer of the alimentary canal, between the inner circular and outer longitudinal layers, and it is responsible for motility, especially the rhythm and force of the contractions of the muscularis. As food enters the different portions of the digestive tract, neurons of the enteric nervous system sense the presence of food and stretch in the walls of the organ. As a result, the myenteric plexus is stimulated, causing contraction in the muscularis layer.
Both the sympathetic and parasympathetic divisions of the autonomic nervous system also influence the digestive system organs. We will discuss specific autonomic innervation of these organs later in this module. In general, sympathetic activation (the fight-or-flight response) restricts the activity of enteric neurons, thereby decreasing GI secretion and motility. In contrast, parasympathetic activation (the rest-and-digest response) increases GI secretion and motility by stimulating neurons of the enteric nervous system.
Functions of the Digestive System
This content is primarily covered in the reading and assignment as self-study.
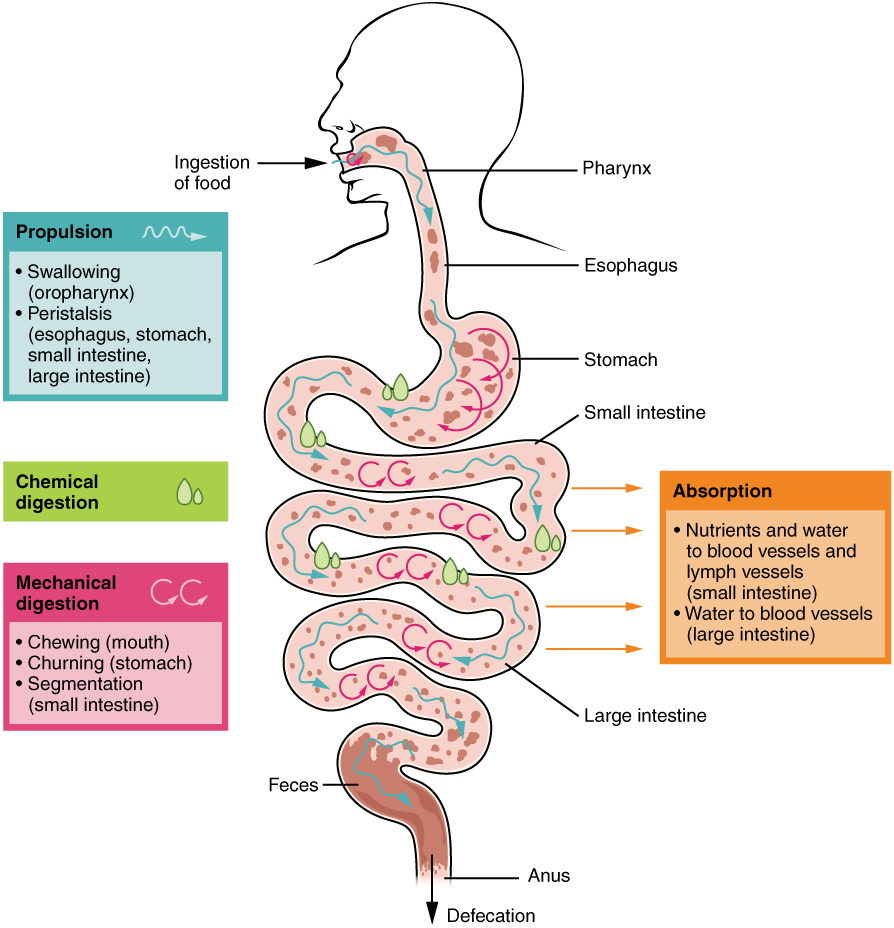
The digestive system has several functions:
- Ingestion: take in food and fluids through the oral cavity
- Propulsion: movement of food through the digestive tract, including swallowing and movement of food through the digestive tract via peristalsis
- Digestion: breaking down of foods in order to release their nutrients
- Mechanical digestion: makes the food smaller to increase both surface area and mobility, including chewing, churning in the stomach, and segmentation primarily in the small intestines
- Chemical digestion: digestive secretions break down complex food molecules into their chemical building blocks
- Secretion: production and delivery substances that lubricate and allow for smooth movement of food through the alimentary canal and substances involved in chemical digestion
- Absorption: take in nutrients and water from the food we digested and transporting them to the bloodstream where they are transported and put to use
- Compaction: remove water (dehydrate) and compact undigested materials (waste) for excretion
- Excretion: removing undigested food and waste produced in the digestive tract through the process of defecation
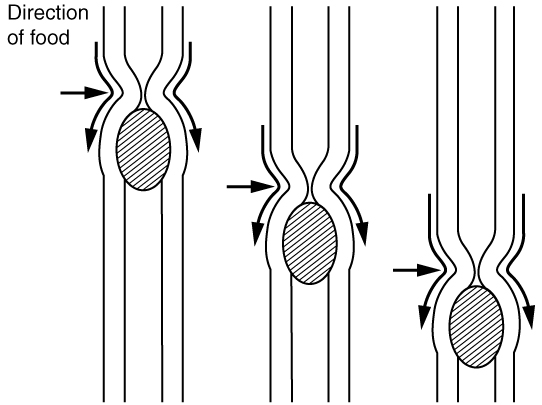
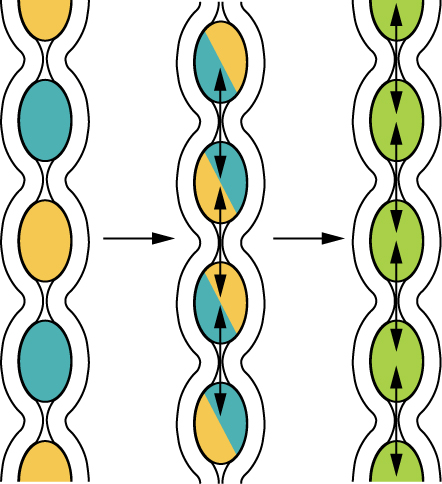
Peristalsis is the sequential, alternating waves of contraction and relaxation of alimentary wall smooth muscles, which act to propel food along the digestive tract. Peristalsis is so powerful that foods and liquids you swallow move along the digestive tract even against gravity.
Segmentation is different than peristalsis, though it does involve localized contractions of circular muscle of the muscularis layer of the alimentary canal. Instead of propelling food substances forward, segmentation is a form of mechanical digestion. These contractions isolate small sections of the intestine, moving their contents back and forth while continuously subdividing, breaking up, and mixing the contents. By moving food back and forth in the intestinal lumen, segmentation mixes food with digestive juices and facilitates absorption.
The following table provides an overview of the specific functions of the organs of the alimentary canal. These organs will be covered in the following sections.
| Functions of the Digestive Organs | |
|---|---|
| Organ | Functions |
| Esophagus |
|
| Stomach |
|
| Small intestine |
|
| Large intestine |
|
The Esophagus
This content will be covered in lecture.
The esophagus is a muscular tube that connects the pharynx to the stomach. It is approximately 25.4 cm (10 in) in length, located posterior to the trachea, and remains in a collapsed form when not engaged in swallowing. It runs a mainly straight route through the mediastinum of the thorax. To enter the abdomen, the esophagus penetrates the diaphragm through an opening called the esophageal hiatus.
The esophagus is liked by non-keratinized, stratified squamous epithelium. This epithelium protects against erosion from food particles. The muscularis layer changes according to location: In the upper third of the esophagus, the muscularis is skeletal muscle. In the middle third, it is both skeletal and smooth muscle. In the lower third, it is smooth muscle. The esophageal walls also contain glands that function to protect it. Esophageal glands proper are most concentrated in the superior portion of the esophagus. They secrete mucous to lubricate the esophagus to help food move easily towards the stomach. Esophageal cardiac glands, located in the inferior portion of the esophagus, secrete a basic substance to help counter against acidic contents that may reflux into the lower esophagus from the stomach.
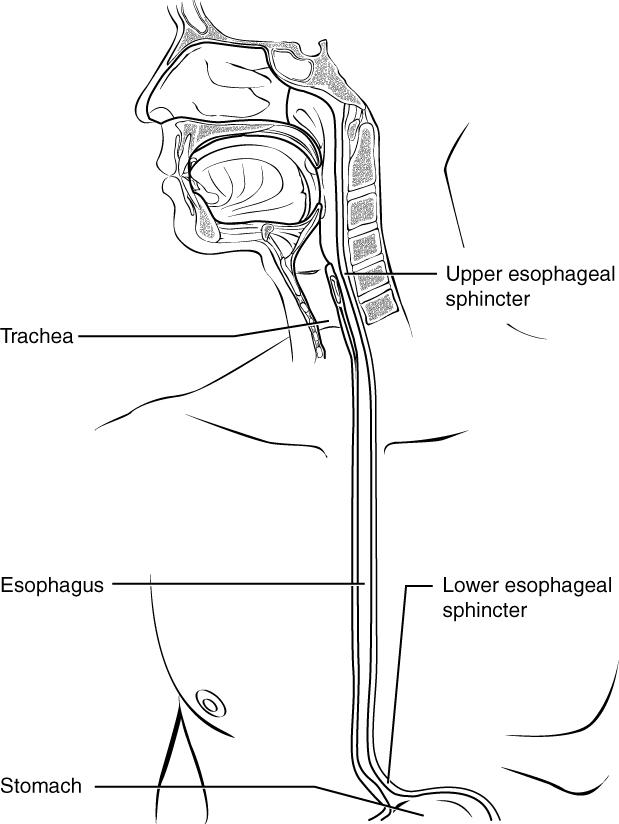
The superior (upper) esophageal sphincter controls the movement of food from the pharynx into the esophagus. Rhythmic waves of peristalsis, which begin in the upper esophagus, propel the bolus of food toward the stomach. Food passes from the esophagus into the stomach at the inferior (lower) esophageal sphincter (also called the gastroesophageal or cardiac sphincter). Recall that sphincters are muscles that surround tubes and serve as valves, closing the tube when the sphincters contract and opening it when they relax. The lower esophageal sphincter relaxes to let food pass into the stomach, and then contracts to prevent stomach acids from backing up into the esophagus. Surrounding this sphincter is the muscular diaphragm, which helps close off the sphincter when no food is being swallowed. When the lower esophageal sphincter does not completely close, the stomach’s contents can reflux (that is, back up into the esophagus), causing heartburn or gastroesophageal reflux disease (GERD).
Stomach
This content will be covered in lecture.
 The stomach is an expansion of the alimentary canal that lies immediately inferior to the esophagus. It links the esophagus to the first part of the small intestine (the duodenum). In addition to its chemical and mechanical digestion functions, the stomach serves as a temporary holding chamber, keeping food and allowing only small amounts into the small intestine at a time. The bolus of food is mixed together with digestive juices in the stomach until together they form chyme, which is released into the small intestine. Little absorption occurs in the stomach, with the exception of the negligible amount of alcohol and certain medications. The contents of the stomach are completely emptied into the duodenum within 2 to 4 hours after you eat a meal. However, note that this is still a fraction of the 24 to 72 hours that full digestion typically takes from start to finish.
The stomach is an expansion of the alimentary canal that lies immediately inferior to the esophagus. It links the esophagus to the first part of the small intestine (the duodenum). In addition to its chemical and mechanical digestion functions, the stomach serves as a temporary holding chamber, keeping food and allowing only small amounts into the small intestine at a time. The bolus of food is mixed together with digestive juices in the stomach until together they form chyme, which is released into the small intestine. Little absorption occurs in the stomach, with the exception of the negligible amount of alcohol and certain medications. The contents of the stomach are completely emptied into the duodenum within 2 to 4 hours after you eat a meal. However, note that this is still a fraction of the 24 to 72 hours that full digestion typically takes from start to finish.
Structure
There are four main regions in the stomach:
- Cardia (or cardiac region): area where the esophagus connects to the stomach and through which food passes into the stomach.
- Fundus: dome-shaped superior portion of the stomach located just inferior to the diaphragm.
- Body: the main, large part of the stomach.
- Pylorus: funnel-shaped region that connects the body of the stomach to the duodenum. The smooth muscle pyloric sphincter is located at this latter point of connection and controls stomach emptying into the duodenum. The small intestines can only process a small amount of chyme at a time, so it’s passage into the duodenum is highly regulated.
The lateral surface of the stomach is called the greater curvature, while the medial border is the lesser curvature. The inner walls contain folds called rugae (gastric folds).
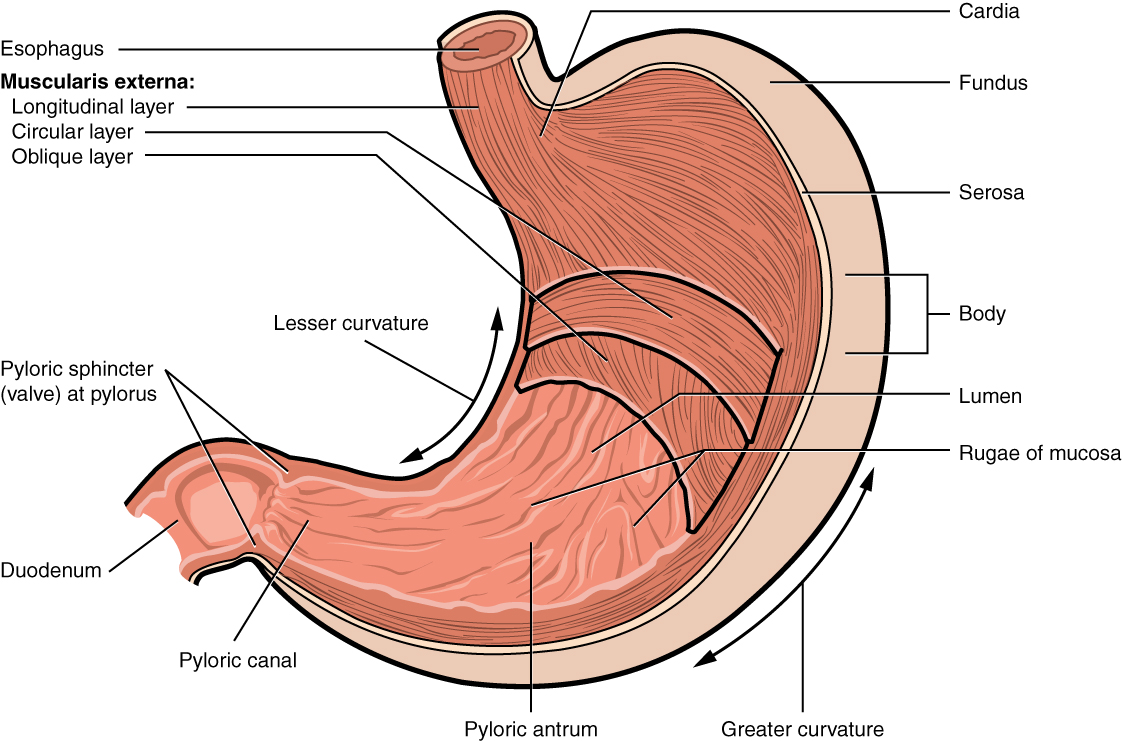
In addition to the typical circular and longitudinal smooth muscle layers, the muscularis has an inner oblique smooth muscle layer. As a result, in addition to moving food through the canal, the stomach can vigorously churn food, mechanically breaking it down into smaller particles.
Epithelium and Cells of the Stomach
The stomach is lined by simple columnar epithelium. A vast number of gastric pits dot the surface of the epithelium and mark the entry to each gastric gland, which secretes a complex digestive fluid referred to as gastric juice.
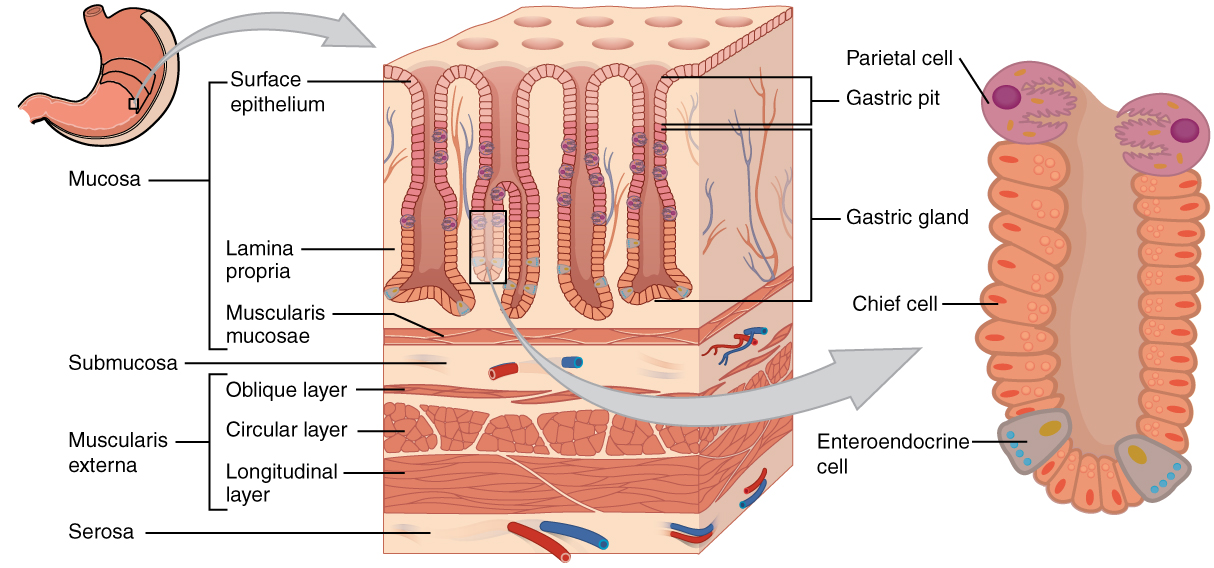
There are five types of cells in the stomach epithelium, including the cells lining the lumen and the cells of the gastric pits:
- Surface mucus cells: line the lumen of the stomach and secrete a protective coat of alkaline mucus to protect the epithelium against the acidic substances in the stomach. This mucus forms a physical barrier, and its bicarbonate ions neutralize acid.
- Parietal cells: located in the gastric glands, which secrete both hydrochloric acid and intrinsic factor. Hydrochloric acid is responsible for the high acidity (pH 1.5 to 3.5) of the stomach contents and is needed to activate the protein-digesting enzyme, pepsin. The acidity also kills much of the bacteria you ingest with food and helps to denature proteins, making them more available for enzymatic digestion. Intrinsic factor is a glycoprotein necessary for the absorption of vitamin B12 in the small intestine.
- Chief cells: located in the gastric glands are chief cells, which secrete pepsinogen, the inactive proenzyme form of pepsin. HCl is necessary for the conversion of pepsinogen to pepsin which is involved in the digestion of proteins.
- Mucous neck cells: located in the gastric pit, and secrete thin, acidic mucus that surrounds to bolus of food in the stomach.
- Enteroendocrine cells: located in the gastric glands, and they secrete gastrin into the interstitial fluid deep to the epithelial cells. When food enters the stomach, gastrin stimulates the other cells above to produce and secrete their substances.
The Small Intestine
This content will be covered in lecture.
 Chyme released from the stomach enters the small intestine, which is smaller in diameter than the large intestine.
Chyme released from the stomach enters the small intestine, which is smaller in diameter than the large intestine.
The small intestine is subdivided into three regions.
- Duodenum: shortest region of the small intestine. It begins at the pyloric sphincter, and it bends posteriorly behind the peritoneum, becoming retroperitoneal, and then makes a C-shaped curve around the head of the pancreas before ascending anteriorly again to return to the peritoneal cavity and join the jejunum. The duodenum can therefore be subdivided into four segments: the superior, descending, horizontal, and ascending duodenum. The transition between the second and third parts is the transition from the foregut to the midgut. The hepatopancreatic ampulla and duodenal papilla is located at this transition point (more on that in Module 15).
-
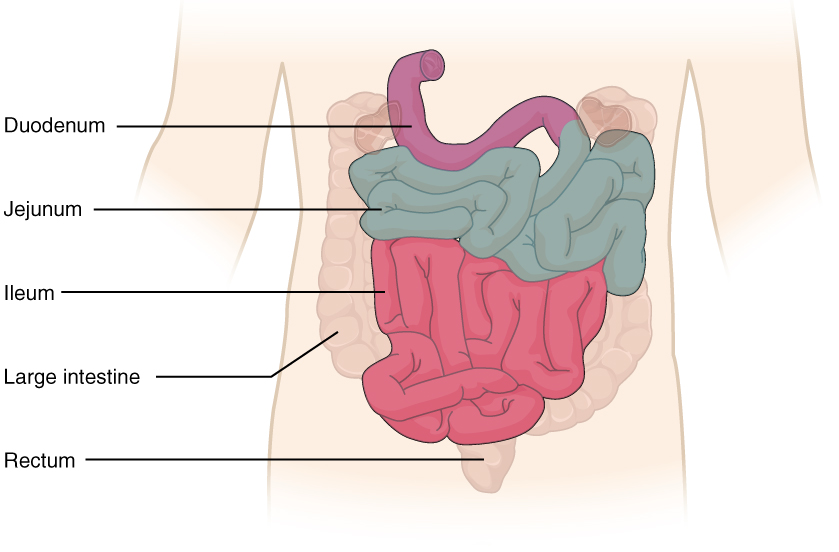
Small Intestine:The three regions of the small intestine are the duodenum, jejunum, and ileum. Jejunum: runs from the duodenum to the ileum. No clear demarcation exists between the jejunum and the final segment of the small intestine, the ileum.
-
Ileum: the longest part of the small intestine. It joins the cecum, the first portion of the large intestine, at the ileocecal valve (or sphincter).
The movement of intestinal smooth muscles includes both segmentation and peristalsis. If you could see into the small intestine when it was going through segmentation, it would look as if the contents were being shoved incrementally back and forth, as the rings of smooth muscle repeatedly contract and then relax. Segmentation in the small intestine does not force chyme through the tract. Instead, it combines the chyme with digestive juices and pushes food particles against the mucosa to be absorbed. When most of the chyme has been absorbed, the small intestinal wall becomes less distended. At this point, the localized segmentation process is replaced by peristaltic movements.
The digestion of proteins and carbohydrates, which partially occurs in the stomach, is completed in the small intestine with the aid of intestinal and pancreatic juices. Lipids arrive in the intestine largely undigested, so much of the focus here is on lipid digestion, which is facilitated by bile and the enzyme pancreatic lipase.
The small intestine is where practically all absorption occurs. In addition to its length, the folds and projections of the lining of the small intestine work to give it an enormous surface area (100x that of your skin!). This large surface area is necessary for complex processes of digestion and absorption that occur within it.
Three features increase the surface area of the small intestine more than 600-fold, substantially increasing the surface area for absorption:
- Circular folds (plica circulare): deep ridges and projections in the mucosa and submucosa. They cause the chyme to spiral through the small intestine, slowing its and providing the time and surface area needed for nutrients to be fully absorbed.
- Villi: Within the circular folds are small hair-like vascularized projections called villi that increase the surface area of the epithelium tremendously. Epithelium, primarily composed of absorptive cells, covers the villi. Each villus contains a capillary bed composed of one arteriole and one venule, as well as a lymphatic capillary called a lacteal. The breakdown products of carbohydrates and proteins (sugars and amino acids) can enter the bloodstream directly, but lipid breakdown products are absorbed by the lacteals and transported to the bloodstream via the lymphatic system.
- Microvilli: Small cylindrical apical surface extensions of the epithelial cells lining the villi. There are an estimated 200 million microvilli per square millimeter of small intestine, greatly expanding the surface area of the plasma membrane and thus greatly enhancing absorption.
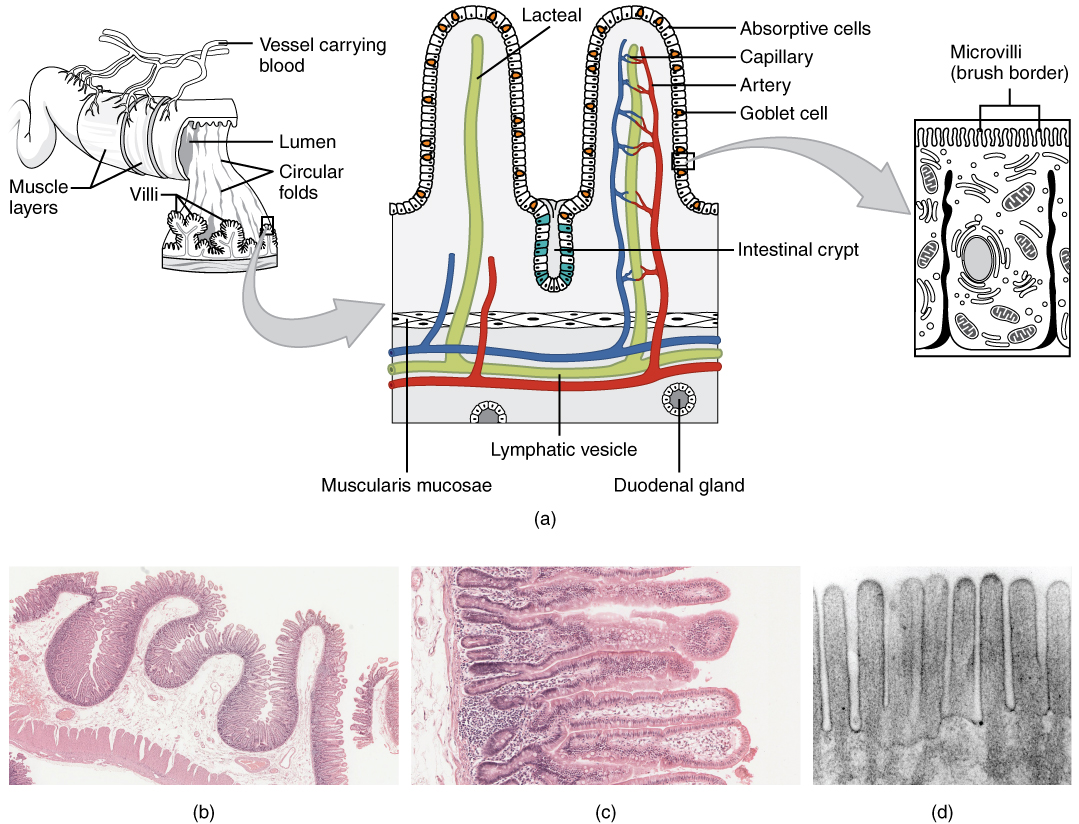
The lamina propria of the small intestine mucosa contains mucosa-associated lymphatic tissue (MALT), typically referred to as Peyer’s patches in certain regions. They serve to keep bacteria from entering the bloodstream.
The Large Intestine
This content will be covered in lecture.
The large intestine is the terminal part of the alimentary canal. The primary functions of this organ are to finish absorption of water, form feces, and eliminate feces from the body. The residue of chyme that enters the large intestine contains few nutrients except water, which is reabsorbed as the residue lingers in the large intestine, typically for 12 to 24 hours.
The large intestine runs from the appendix to the anus and frames the small intestine on three sides. Despite its being about one-half as long as the small intestine, it is called large because it is more than twice the diameter of the small intestine. The large intestine is subdivided into four main regions:
- Cecum: The first part of the large intestine is the cecum, a sac-like structure that is suspended inferior to the ileocecal valve. The ileocecal valve controls the flow of chyme from the ilium of the small intestine to the cecum of the large intestine.
- The appendix (or vermiform appendix) is a winding tube that attaches to the cecum. It contains lymphoid tissue, suggesting an immunologic function
-
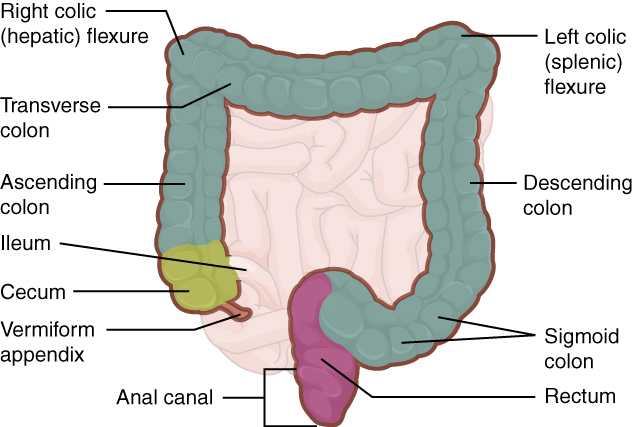
Large Intestine: The large intestine includes the cecum, colon, and rectum. Ascending colon: ascends on the right side of the abdomen.
- Right colic flexure (hepatic flexure): at the inferior surface of the liver, the colon bends to form the transverse colon
- Transverse colon: travels across the abdomen from right to left. The region defined as hindgut begins with the last third of the transverse colon and continues on.
- Left colic flexure (splenic flexure): where the colon angles sharply immediately inferior to the spleen.
- Descending colon: runs inferiorly along the left side of the posterior abdominal wall.
- Sigmoid colon: inferior to the descending colon in the lower left quadrant. It is s-shaped and extends medially to the midline.
- Rectum: in the pelvis, extending anterior to the sacrum and coccyx. It follows the curved contour of the sacrum and has three lateral bends that create a trio of internal transverse folds called the rectal valves. These valves help separate the feces from gas to prevent the simultaneous passage of feces and gas.
- Anal canal: located in the perineum, completely outside of the abdominopelvic cavity. It opens to the exterior of the body at the anus. The anal canal includes two sphincters. The internal anal sphincter is made of smooth muscle, and its contractions are involuntary. The external anal sphincter is made of skeletal muscle, which is under voluntary control. Except when defecating, both usually remain closed.
- The stratified squamous epithelial mucosa of the anal canal connects to the skin on the outside of the anus. This mucosa varies considerably from that of the rest of the colon to accommodate the high level of abrasion as feces pass through.
- The anal canal’s mucous membrane is organized into longitudinal folds, each called an anal column. Depressions between the anal columns, each called an anal sinus, secrete mucus that facilitates defecation. The pectinate line is a horizontal, jagged band that runs circumferentially just below the level of the anal sinuses, and represents the junction between the hindgut and external skin. The mucosa above this line is innervated by visceral sensory fibers, and the lower region is innervated by somatic sensory fibers.
Unlike the small intestines, there are no circular folds or villi in the large intestines. Other than in the anal canal, the mucosa of the colon is simple columnar epithelium made mostly of colonocytes (absorptive cells) and goblet cells. These goblet cells secrete mucus that eases the movement of feces and protects the intestine from the effects of the acids and gases produced by enteric bacteria. The enterocytes absorb water and salts as well as vitamins produced by your intestinal bacteria.
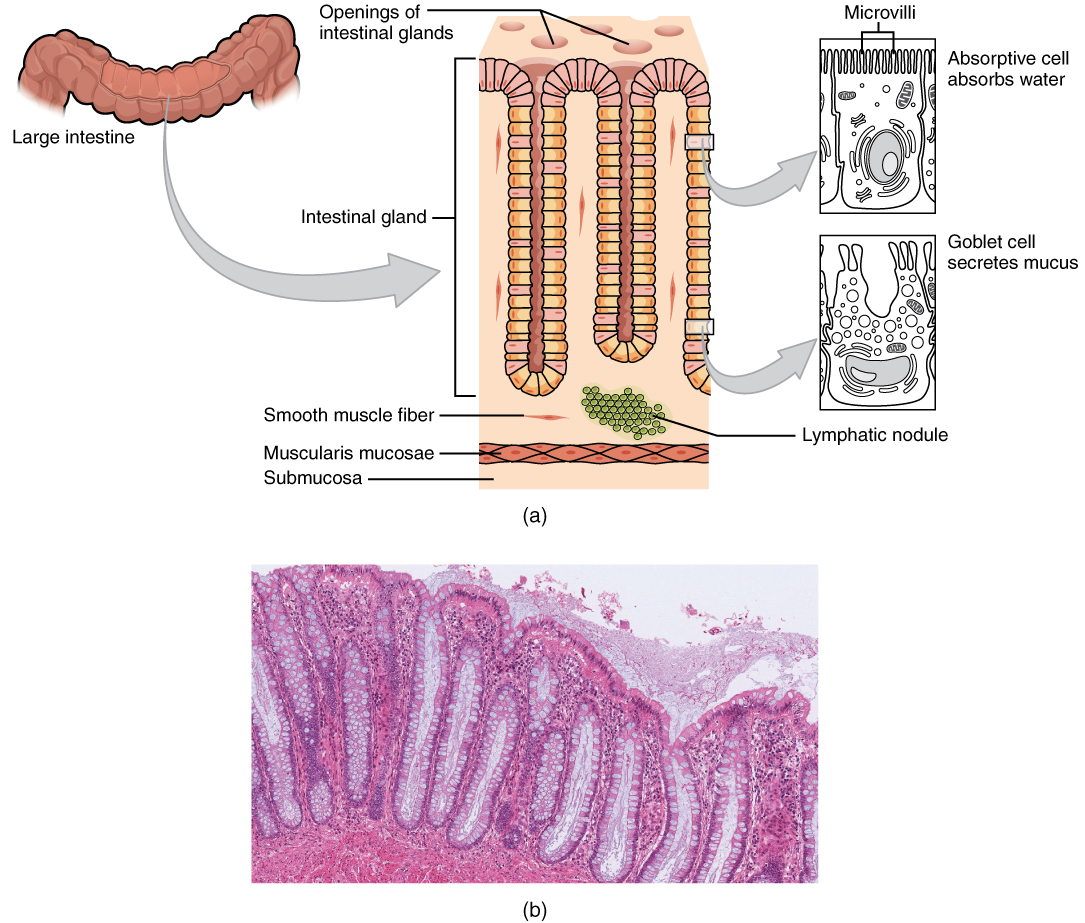
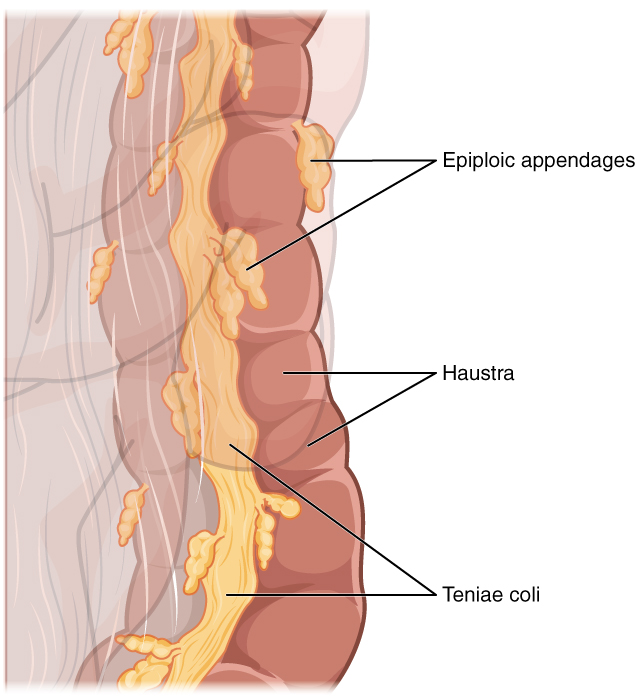
Three features are unique to the large intestine
- Teniae coli: three bands of smooth muscle that make up the longitudinal muscle layer of the muscularis of the large intestine.
- Haustra: pouches created by tonic contractions of the teniae coli
- Omental appendices (epiploic appendages): fat-filled sacs of visceral peritoneum. The purpose of these is unknown.
Absorption, Feces Formation, and Defecation
The large intestine absorbs most of the remaining water to convert the liquid chyme residue into semisolid feces (“stool”). Feces are eliminated through contractions of the rectal muscles.
The process of defecation begins when mass movements force feces from the colon into the rectum, stretching the rectal wall and provoking the defecation reflex, which eliminates feces from the rectum. This parasympathetic reflex is mediated by the spinal cord. It contracts the sigmoid colon and rectum, relaxes the internal anal sphincter, and initially contracts the external anal sphincter. The presence of feces in the anal canal sends a signal to the brain, which gives you the choice of voluntarily opening the external anal sphincter (defecating) or keeping it temporarily closed. If you decide to delay defecation, it takes a few seconds for the reflex contractions to stop and the rectal walls to relax. The next mass movement will trigger additional defecation reflexes until you defecate.
If defecation is delayed for an extended time, additional water is absorbed, making the feces firmer and potentially leading to constipation. On the other hand, if the waste matter moves too quickly through the intestines, not enough water is absorbed, and diarrhea can result.

