Module 17: Female Reproductive System
Learning Objectives:
By the end of this module, students will be able to:
- Describe the gross anatomy of the female reproductive organs.
- Explain the anatomy of the vagina and external female genitalia.
- Detail the anatomy of the mammary glands.
Terms to Know
|
Reproductive System – General
Female Reproductive System
|
Female Reproductive System (continued)
|
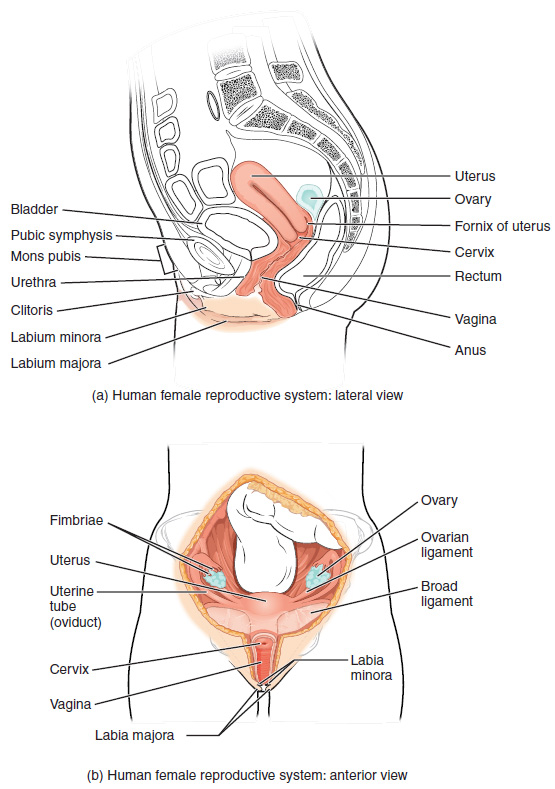
The female reproductive system functions to produce gametes and reproductive hormones, just like the male reproductive system; however, it also has the additional task of supporting the developing fetus and delivering it to the outside world. Unlike its male counterpart, the female reproductive system is located primarily inside the pelvic cavity. Recall that the ovaries are the female gonads. The gamete they produce is called an oocyte.
External Female Genitals
*This content will be covered in lecture.
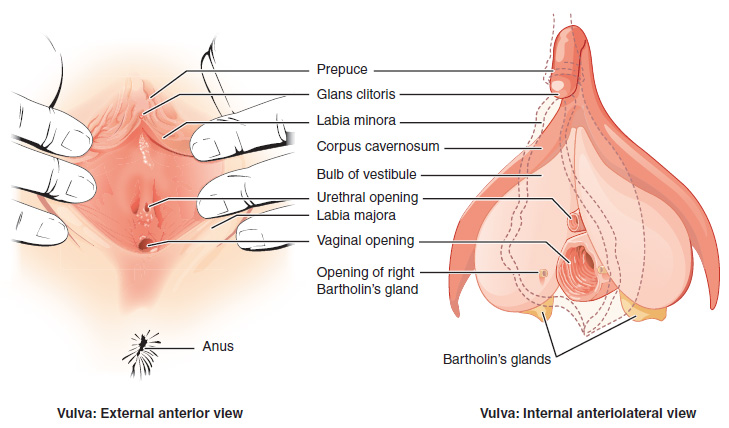
The external female reproductive structures are referred to collectively as the vulva. The mons pubis is a pad of fat that is located anteriorly, over the pubic bone. After puberty, it becomes covered in pubic hair. The labia majora (labia = “lips”; majora = “larger”) are folds of hair-covered skin that begin just posterior to the mons pubis. The thinner and more pigmented labia minora (labia = “lips”; minora = “smaller”) extend medially to the labia majora. Although they naturally vary in shape and size from woman to woman, the labia minora serves to protect the female urethra and the entrance to the female reproductive tract.
The superior, anterior portions of the labia minora come together to encircle the clitoris (or glans clitoris), an organ that originates from the same cells as the glans penis and has abundant nerves that make it important in sexual sensation and orgasm. The hymen is a thin membrane that sometimes partially covers the entrance to the vagina. The vaginal opening is located between the opening of the urethra and the anus. It is flanked by outlets to the greater vestibular (Bartholin’s) glands.
Vagina
*This content is introduced in the pre-lecture assignment and will be elaborated on in lecture.
The vagina is a muscular canal (approximately 10 cm long) that serves as the entrance to the reproductive tract. It also serves as the exit from the uterus during menses and childbirth. The outer walls of the anterior and posterior vagina are formed into longitudinal columns, or ridges, and the superior portion of the vagina—called the fornix—meets the protruding uterine cervix. The walls of the vagina are lined with an outer, fibrous adventitia; a middle layer of smooth muscle; and an inner mucous membrane with transverse folds called rugae. Together, the middle and inner layers allow the expansion of the vagina to accommodate intercourse and childbirth. The greater vestibular glands and the lesser vestibular glands (located near the clitoris) secrete mucus, which keeps the vestibular area moist.
The vagina is home to a normal population of microorganisms that help to protect against infection by pathogenic bacteria, yeast, or other organisms that can enter the vagina. In a healthy woman, the most predominant type of vaginal bacteria is from the genus Lactobacillus. This family of beneficial bacterial flora secretes lactic acid, and thus protects the vagina by maintaining an acidic pH (below 4.5). Potential pathogens are less likely to survive in these acidic conditions. Lactic acid, in combination with other vaginal secretions, makes the vagina a self-cleansing organ.
Ovaries
*This content is introduced in the pre-lecture assignment and will be elaborated on in lecture.
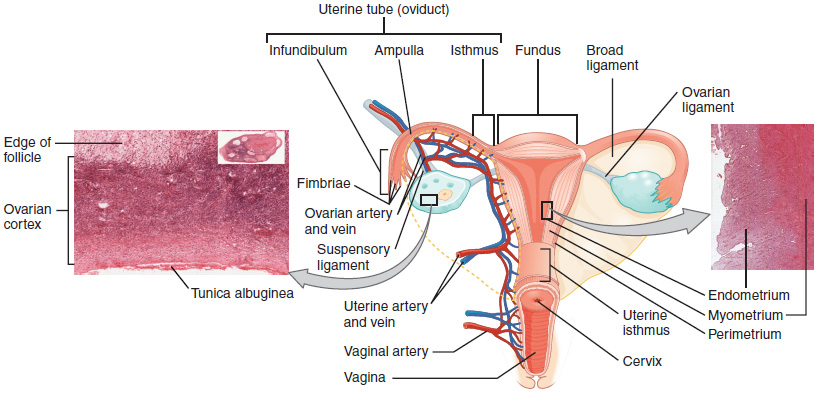
The ovaries are the female gonads. Paired ovals, they are each about 2 to 3 cm in length, about the size of an almond. The ovaries are located within the pelvic cavity and are supported by the mesovarium, an extension of the peritoneum that connects the ovaries to the broad ligament. Extending from the mesovarium itself is the suspensory ligament that contains the ovarian blood and lymph vessels. Finally, the ovary itself is attached to the uterus via the ovarian ligament.
The ovary comprises an outer covering of cuboidal epithelium called the ovarian surface epithelium that is superficial to a dense connective tissue covering called the tunica albuginea. Beneath the tunica albuginea is the cortex, or outer portion, of the organ. The cortex is composed of a tissue framework called the ovarian stroma that forms the bulk of the adult ovary. Oocytes develop within the outer layer of this stroma, each surrounded by supporting cells. This grouping of an oocyte and its supporting cells is called a follicle. Beneath the cortex lies the inner ovarian medulla, the site of blood vessels, lymph vessels, and the nerves of the ovary.
The Ovarian Cycle
*This content is self-study.
The ovarian cycle is a set of predictable changes in a female’s oocytes and ovarian follicles. During a woman’s reproductive years, it is a roughly 28-day cycle that can be correlated with but is not the same as, the menstrual cycle. The cycle includes two interrelated processes: oogenesis (the production of female gametes) and folliculogenesis (the growth and development of ovarian follicles).
Oogenesis – FYI (For Your Information -> you will not be assessed on this content)
Gametogenesis in females is called oogenesis. The process begins with the ovarian stem cells or oogonia. Oogonia are formed during fetal development, and divide via mitosis, much like spermatogonia in the testis. Unlike spermatogonia, however, oogonia form primary oocytes in the fetal ovary prior to birth. These primary oocytes are then arrested in this stage of meiosis I, only to resume it years later, beginning at puberty and continuing until the woman is near menopause (the cessation of a woman’s reproductive functions). The number of primary oocytes present in the ovaries declines from one to two million in an infant, to approximately 400,000 at puberty, to zero by the end of menopause.
The initiation of ovulation—the release of an oocyte from the ovary—marks the transition from puberty into reproductive maturity for women. From then on, throughout a woman’s reproductive years, ovulation occurs approximately once every 28 days. Just prior to ovulation, a surge of luteinizing hormone triggers the resumption of meiosis in a primary oocyte. This initiates the transition from primary to secondary oocyte.
The Uterine Tubes
*This content is introduced in the pre-lecture assignment and will be elaborated on in lecture.
The uterine tubes (also called fallopian tubes or oviducts) serve as the conduit of the oocyte from the ovary to the uterus. Each of the two uterine tubes is close to, but not directly connected to, the ovary and divided into sections. The wide, distal infundibulum flares out with slender, finger-like projections called fimbriae. The middle region of the tube, called the ampulla, is where fertilization often occurs. The isthmus is the narrow medial end of each uterine tube that connects to the uterus at the uterine part of the uterine tube. The uterine tubes also have three layers: an outer serosa, a middle smooth muscle layer, and an inner mucosal layer. In addition to its mucus-secreting cells, the inner mucosa contains ciliated cells that beat in the direction of the uterus, producing a current that will be critical to move the oocyte.
Following ovulation, the secondary oocyte surrounded by a few granulosa cells is released into the peritoneal cavity. The nearby uterine tube, either left or right, receives the oocyte. Unlike sperm, oocytes lack flagella, and therefore cannot move on their own. So how do they travel into the uterine tube and toward the uterus? High concentrations of estrogen that occur around the time of ovulation induce contractions of the smooth muscle along the length of the uterine tube. These contractions occur every 4 to 8 seconds, and the result is a coordinated movement that sweeps the surface of the ovary and the pelvic cavity. Current flowing toward the uterus is generated by coordinated beating of the cilia that line the outside and lumen of the length of the uterine tube. These cilia beat more strongly in response to the high estrogen concentrations that occur around the time of ovulation. As a result of these mechanisms, the oocyte–granulosa cell complex is pulled into the interior of the tube. Once inside, the muscular contractions and beating cilia move the oocyte slowly toward the uterus. When fertilization does occur, sperm typically meet the egg while it is still moving through the ampulla.
The open-ended structure of the uterine tubes can have significant health consequences if bacteria or other contagions enter through the vagina and move through the uterus, into the tubes, and then into the pelvic cavity. If this is left unchecked, a bacterial infection (sepsis) could quickly become life-threatening. Sepsis is also associated with sexually transmitted bacterial infections, especially gonorrhea and chlamydia. These increase a woman’s risk for pelvic inflammatory disease (PID), infection of the uterine tubes or other reproductive organs. Even when resolved, PID can leave scar tissue in the tubes, leading to infertility.
The Uterus and Cervix
*This content is introduced in the pre-lecture assignment and will be elaborated on in lecture.
The uterus is the muscular organ that nourishes and supports the growing embryo. Its average size is approximately 5 cm wide by 7 cm long (approximately 2 in by 3 in) when a female is not pregnant. It has four sections. The portion of the uterus superior to the opening of the uterine tubes is called the fundus. The middle section of the uterus is called the body of the uterus. The narrowing portion prior to the cervix is called the isthmus. The cervix is the narrow inferior portion of the uterus that projects into the vagina. The cervix has three regions. The internal os (os = “opening”) is the deepest (closest to the isthmus of the uterus) region of the cervix. The external os is the region closest to the vagina and the cervical canal is the region between the internal and external openings. The cervix produces mucus secretions that become thin and stringy under the influence of high systemic plasma estrogen concentrations, and these secretions can facilitate sperm movement through the reproductive tract.
Several ligaments maintain the position of the uterus within the abdominopelvic cavity. The broad ligament is a fold of the peritoneum that serves as a primary support for the uterus, extending laterally from both sides of the uterus and attaching it to the pelvic wall. The round ligament attaches to the uterus near the uterine tubes and extends to the labia majora. Finally, the uterosacral ligament stabilizes the uterus posteriorly by its connection from the cervix to the pelvic wall.
The wall of the uterus is made up of three layers. The most superficial layer is the serous membrane, or perimetrium, which consists of epithelial tissue that covers the exterior portion of the uterus. The middle layer, or myometrium, is a thick layer of smooth muscle responsible for uterine contractions. Most of the uterus is myometrial tissue, and the muscle fibers run horizontally, vertically, and diagonally, allowing the powerful contractions that occur during labor and the less powerful contractions (or cramps) that help to expel menstrual blood during a woman’s period. Anteriorly directed myometrial contractions also occur near the time of ovulation and are thought to possibly facilitate the transport of sperm through the female reproductive tract.
The innermost layer of the uterus is called the endometrium. The endometrium contains a connective tissue lining, the lamina propria, which is covered by epithelial tissue that lines the lumen. Structurally, the endometrium consists of two layers: the stratum basalis and the stratum functionalis (the basal and functional layers). The stratum basalis layer is part of the lamina propria and is adjacent to the myometrium; this layer does not shed during menses. In contrast, the thicker stratum functionalis layer contains the glandular portion of the lamina propria and the endothelial tissue that lines the uterine lumen. It is the stratum functionalis that grows and thickens in response to increased levels of estrogen and progesterone. In the luteal phase of the menstrual cycle, special branches off of the uterine artery called spiral arteries supply the thickened stratum functionalis. This inner functional layer provides the proper site of implantation for the fertilized egg, and—should fertilization not occur—it is only the stratum functionalis layer of the endometrium that sheds during menstruation.
The Breasts
*This content is introduced in the pre-lecture assignment and will be elaborated on in lecture.
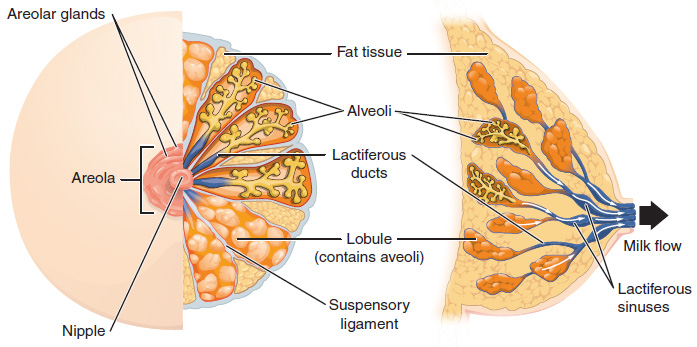
Whereas the breasts are located far from the other female reproductive organs, they are considered accessory organs of the female reproductive system. The function of the breasts is to supply milk to an infant in a process called lactation. The external features of the breast include a nipple surrounded by a pigmented areola, whose coloration may deepen during pregnancy. The areola is typically circular and can vary in size from 25 to 100 mm in diameter. The areolar region is characterized by small, raised areolar glands that secrete lubricating fluid during lactation to protect the nipple from chafing. When a baby nurses, or draws milk from the breast, the entire areolar region is taken into the mouth.
Breast milk is produced by the mammary glands, which are modified sweat glands. Groups of milk-secreting cells in clusters called alveoli produce milk. The alveoli secrete milk into lactiferous ducts which extend to a lactiferous sinus before secreting through pores in the nipples. The clusters can change in size depending on the amount of milk in the alveolar lumen. Once the milk is made in the alveoli, stimulated myoepithelial cells that surround the alveoli contract to push the milk to the lactiferous sinuses. From here, the baby can draw milk through the nipple by suckling. The lobes themselves are surrounded by fat tissue, which determines the size of the breast; breast size differs between individuals and does not affect the amount of milk produced. Supporting the breasts are multiple bands of connective tissue called suspensory ligaments that connect the breast tissue to the dermis of the overlying skin.
During the normal hormonal fluctuations in the menstrual cycle, breast tissue responds to changing levels of estrogen and progesterone, which can lead to swelling and breast tenderness in some individuals, especially during the secretory phase. If pregnancy occurs, the increase in hormones leads to further development of the mammary tissue and enlargement of the breasts.
Aging and the Female Reproductive System – FYI (For Your Information -> you will not be assessed on this content)
The earliest changes occur during the menopausal transition, often referred to as peri-menopause, when a women’s cycle becomes irregular but does not stop entirely. Although the levels of estrogen are still nearly the same as before the transition, the level of progesterone produced by the corpus luteum is reduced. This decline in progesterone can lead to abnormal growth, or hyperplasia, of the endometrium. This condition is a concern because it increases the risk of developing endometrial cancer. Two harmless conditions that can develop during the transition are uterine fibroids, which are benign masses of cells, and irregular bleeding. As estrogen levels change, other symptoms that occur are hot flashes and night sweats, trouble sleeping, vaginal dryness, mood swings, difficulty focusing, and thinning of hair on the head along with the growth of more hair on the face. Depending on the individual, these symptoms can be entirely absent, moderate, or severe.
After menopause, lower amounts of estrogens can lead to other changes. Cardiovascular disease becomes as prevalent in women as in men, possibly because estrogen reduces the amount of cholesterol in the blood vessels. When estrogen is lacking, many women find that they suddenly have problems with high cholesterol and the cardiovascular issues that accompany it. Osteoporosis is another problem because bone density decreases rapidly in the first years after menopause. The reduction in bone density leads to a higher incidence of fractures.
Hormone therapy (HT), which employs medication (synthetic estrogens and progestins) to increase estrogen and progestin levels, can alleviate some of the symptoms of menopause. In 2002, the Women’s Health Initiative began a study to observe women for the long-term outcomes of hormone replacement therapy over 8.5 years. However, the study was prematurely terminated after 5.2 years because of evidence of a higher than normal risk of breast cancer in patients taking estrogen-only HT. The potential positive effects on cardiovascular disease were also not realized in the estrogen-only patients. The results of other hormone replacement studies over the last 50 years, including a 2012 study that followed over 1,000 menopausal women for 10 years, have shown cardiovascular benefits from estrogen and no increased risk for cancer. Some researchers believe that the age group tested in the 2002 trial may have been too old to benefit from the therapy, thus skewing the results. In the meantime, intense debate and study of the benefits and risks of replacement therapy is ongoing. Current guidelines approve HT for the reduction of hot flashes or flushes, but this treatment is generally only considered when women first start showing signs of menopausal changes, if used in the lowest dose possible for the shortest time possible (5 years or less), and it is suggested that women on HT have regular pelvic and breast exams.
Sexual Differentiation
*This content will be covered in lecture.
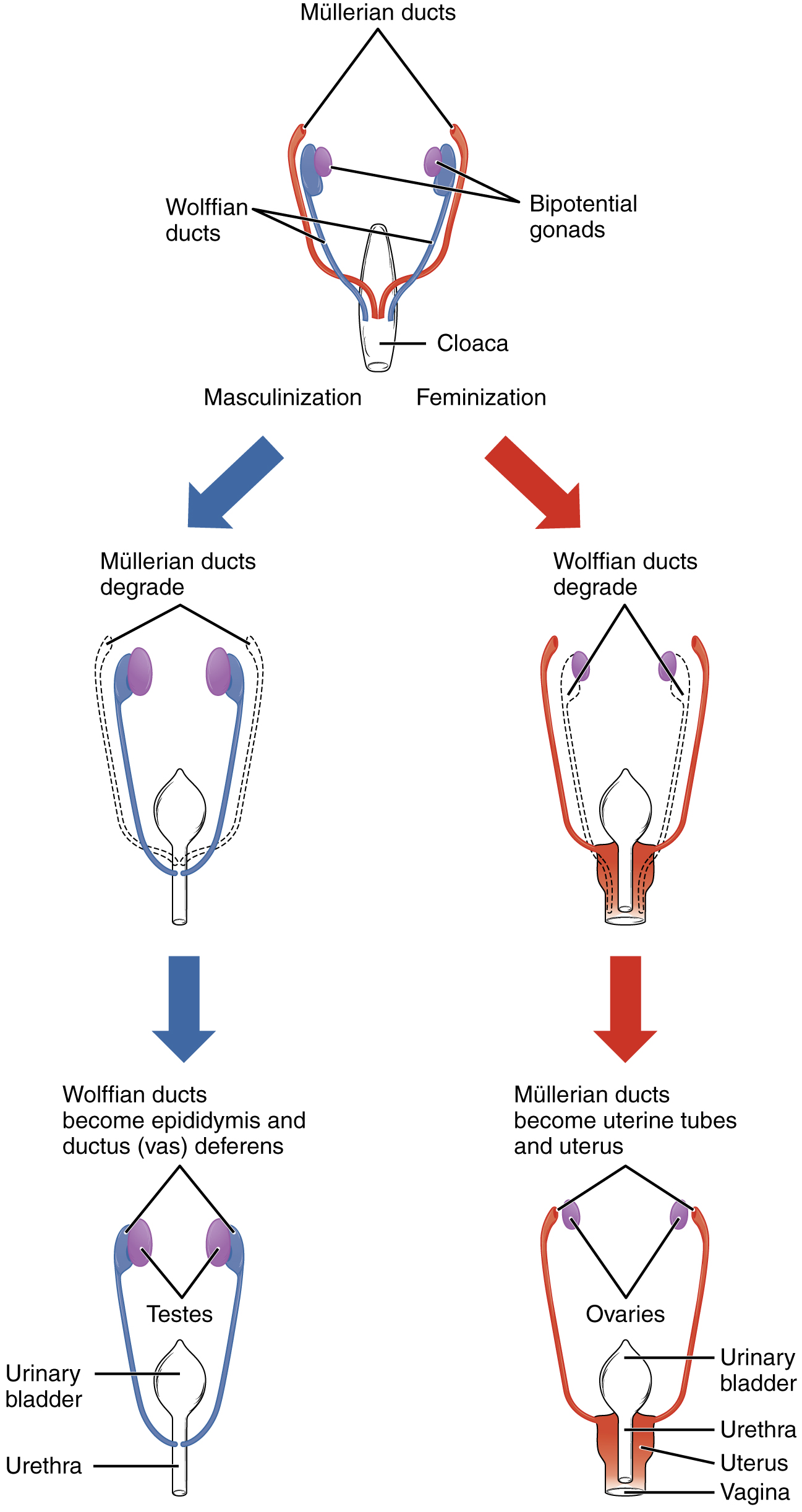
Sexual differentiation does not begin until the fetal period, during weeks 9–12. Embryonic males and females, though genetically distinguishable, are morphologically identical. Bipotential gonads, or gonads that can develop into male or female sexual organs, are connected to a central cavity called the cloaca via Müllerian ducts and Wolffian ducts. (The cloaca is an extension of the primitive gut.) Several events lead to sexual differentiation during this period.
During male fetal development, the bipotential gonads become the testes and associated epididymis. The Müllerian ducts degenerate. The Wolffian ducts become the vas deferens, and the cloaca becomes the urethra and rectum.
During female fetal development, the bipotential gonads develop into ovaries. The Wolffian ducts degenerate. The Müllerian ducts become the uterine tubes and uterus, and the cloaca divides and develops into a vagina, a urethra, and a rectum.