Module 26: Pharynx and Larynx | Nasal Cavity and Smell
Learning Objectives:
By the end of this class, students will be able to:
- Compare and contrast the functions of the regions of the pharynx.
- Explain the action of swallowing using the palatal muscles, laryngeal elevators, and pharyngeal constrictors.
- Describe the anatomy and functions of the larynx.
- Identify and describe the function of the vocal folds, vestibular folds, and glottis.
- Describe how the cartilages of the larynx move to produce sound with air movement through the larynx.
- Describe the anatomy of the nasal cavity.
- Describe the structure and function of the paranasal sinuses.
- Identify and describe the structure, location, and innervation pathway of olfactory receptors.
Terms to Know
|
Pharynx
Larynx
|
Nasal Cavity and Related Structures
Olfaction
|
The Pharynx
The pharynx is involved in both digestion and respiration. It receives food and air from the mouth, and air from the nasal cavities. When food enters the pharynx, involuntary muscle contractions close off the air passageways.
A short tube of skeletal muscle lined with a mucous membrane, the pharynx runs from the posterior oral and nasal cavities to the opening of the esophagus and larynx. It has three subdivisions. The most superior, the nasopharynx, is involved only in breathing and speech. The other two subdivisions, the oropharynx and the laryngopharynx are used for both breathing and digestion. The oropharynx begins inferior to the nasopharynx and is continuous below with the laryngopharynx. The inferior border of the laryngopharynx connects to the esophagus, whereas the anterior portion connects to the larynx, allowing air to flow into the bronchial tree.
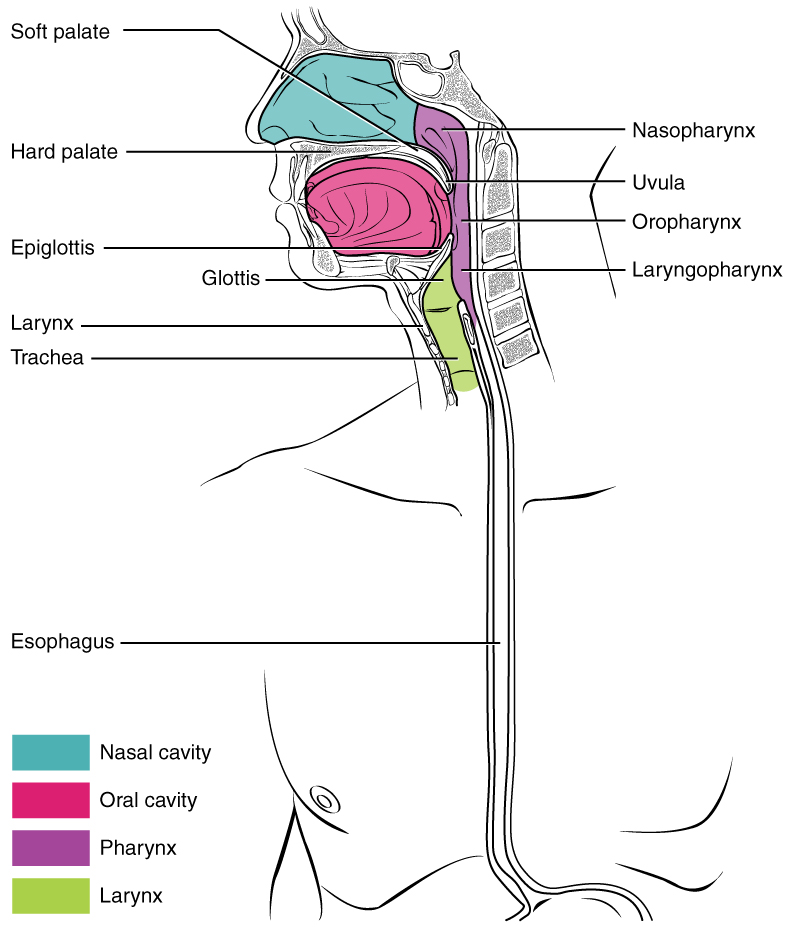
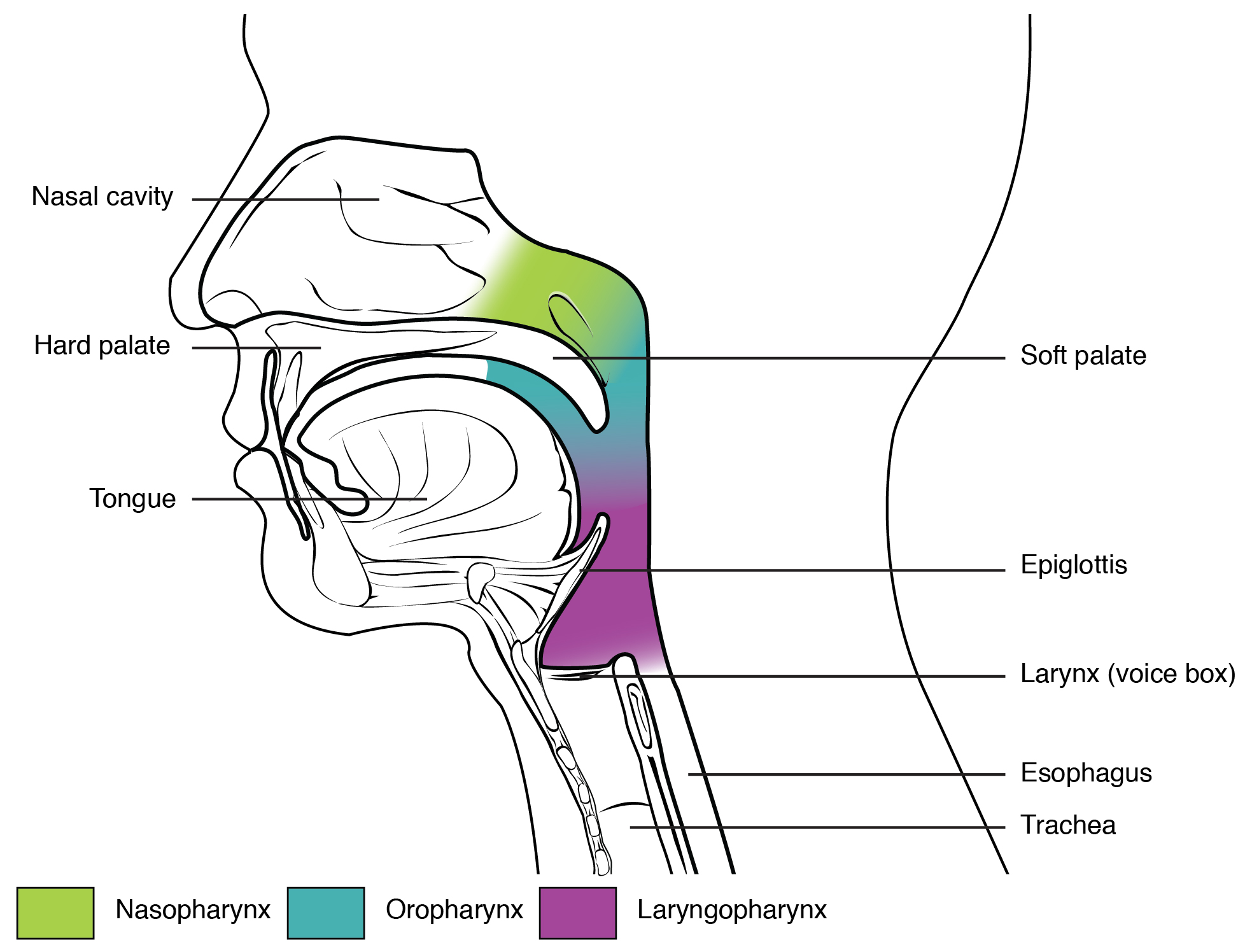
The Nasopharynx
The nasopharynx is flanked by the conchae of the nasal cavity, and it serves only as an airway. At the top of the nasopharynx are the pharyngeal tonsils. The pharyngeal tonsils, also known as adenoid (adenoid tonsils), are aggregates of lymphoid reticular tissue similar to a lymph node that lies at the superior portion of the nasopharynx. The function of the pharyngeal tonsil is not well understood, but it contains a rich supply of lymphocytes and is covered with ciliated epithelium that traps and destroys invading pathogens that enter during inhalation. The pharyngeal tonsils are large in children, but interestingly, tend to regress with age and may even disappear. The uvula is a small bulbous, teardrop-shaped structure located at the apex of the soft palate. Both the uvula and soft palate move like a pendulum during swallowing, swinging upward to close off the nasopharynx to prevent ingested materials from entering the nasal cavity. In addition, auditory (Eustachian) tubes that connect to each middle ear cavity open into the nasopharynx. This connection is why colds often lead to ear infections.
The Oropharynx
The oropharynx is a passageway for both air and food. The oropharynx is bordered superiorly by the nasopharynx and anteriorly by the oral cavity. Histologically, the wall of the oropharynx is similar to that of the oral cavity. The mucosa includes a stratified squamous epithelium that is endowed with mucus-producing glands. As the nasopharynx becomes the oropharynx, the epithelium changes from pseudostratified ciliated columnar epithelium to stratified squamous epithelium. The oropharynx contains two distinct sets of tonsils, the palatine, and lingual tonsils. The palatine tonsil is one of a pair of structures located posterolaterally in the oropharynx. The lingual tonsil is located at the base of the tongue. Similar to the pharyngeal tonsil, the palatine and lingual tonsils are composed of lymphoid tissue and trap and destroy pathogens entering the body through the oral or nasal cavities.
The Laryngopharynx
The laryngopharynx is inferior to the oropharynx and posterior to the larynx. It continues the route for ingested material and air until its inferior end, where the digestive and respiratory systems diverge. The stratified squamous epithelium of the oropharynx is continuous with the laryngopharynx. Anteriorly, the laryngopharynx opens into the larynx, whereas posteriorly, it enters the esophagus.
Deglutition (Swallowing)
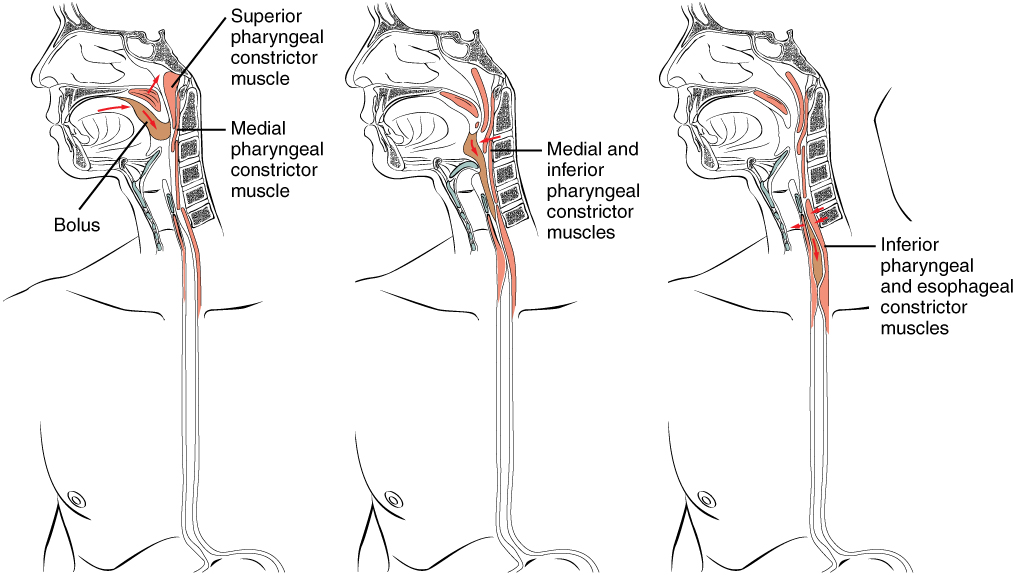
Deglutition is another word for swallowing—the movement of food from the mouth to the stomach. The entire process takes about 4 to 8 seconds for solid or semisolid food, and about 1 second for very soft food and liquids. Although this sounds quick and effortless, deglutition is, in fact, a complex process that involves both the skeletal muscle of the tongue and the muscles of the pharynx and esophagus. It is aided by the presence of mucus and saliva. There are three stages in deglutition: the voluntary phase, the pharyngeal phase, and the esophageal phase. The autonomic nervous system controls the latter two phases.
During swallowing, the elevator skeletal muscles of the pharynx contract, raising and expanding the pharynx to receive the bolus of food. Once received, these muscles relax, and the constrictor muscles of the pharynx contract, forcing the bolus into the esophagus and initiating peristalsis. Usually, during swallowing, the soft palate and uvula rise reflexively to close off the entrance to the nasopharynx. At the same time, the larynx is pulled superiorly and the cartilaginous epiglottis, its most superior structure, folds inferiorly, covering the glottis (the opening to the larynx); this process effectively blocks access to the trachea and bronchi. When the food “goes down the wrong tube,” it goes into the trachea. When food enters the trachea, the reaction is to cough, which usually forces the food up and out of the trachea, and back into the pharynx.
Deglutition
The Voluntary Phase
The voluntary phase of deglutition (also known as the oral or buccal phase) is so-called because you can control when you swallow food. In this phase, chewing has been completed and swallowing is set in motion. The tongue moves upward and backward against the palate, pushing the bolus to the back of the oral cavity and into the oropharynx. Other muscles keep the mouth closed and prevent food from falling out. At this point, the two involuntary phases of swallowing begin.
The Pharyngeal Phase
In the pharyngeal phase, stimulation of receptors in the oropharynx sends impulses to the deglutition center (a collection of neurons that controls swallowing) in the medulla oblongata. Impulses are then sent back to the uvula and soft palate, causing them to move upward and close off the nasopharynx. The laryngeal muscles also constrict to prevent aspiration of food into the trachea. At this point, deglutition apnea takes place, which means that breathing ceases for a very brief time. Contractions of the pharyngeal constrictor muscles move the bolus through the oropharynx and laryngopharynx. Relaxation of the upper esophageal sphincter then allows food to enter the esophagus.
The Esophageal Phase
The entry of food into the esophagus marks the beginning of the esophageal phase of deglutition and the initiation of peristalsis. As in the previous phase, the complex neuromuscular actions are controlled by the medulla oblongata. Peristalsis propels the bolus through the esophagus and toward the stomach. The circular muscle layer of the muscularis contracts, pinching the esophageal wall and forcing the bolus forward. At the same time, the longitudinal muscle layer of the muscularis also contracts, shortening this area and pushing out its walls to receive the bolus. In this way, a series of contractions keep moving food toward the stomach. When the bolus nears the stomach, distention of the esophagus initiates a short reflex relaxation of the lower esophageal sphincter that allows the bolus to pass into the stomach. During the esophageal phase, esophageal glands secrete mucus that lubricates the bolus and minimizes friction.
The Larynx
The larynx is a cartilaginous structure inferior and anterior to the laryngopharynx that connects the pharynx to the trachea and helps regulate the volume of air that enters and leaves the lungs. The structure of the larynx is formed by several pieces of cartilage. Three large cartilage pieces—the thyroid cartilage (anterior), epiglottis (superior), and cricoid cartilage (inferior)—form the major structure of the larynx. The thyroid cartilage is the largest piece of cartilage that makes up the larynx. The thyroid cartilage consists of the laryngeal prominence (Adam’s apple) which tends to be more prominent in people with high levels of testosterone. The thick cricoid cartilage forms a ring, with a wide posterior region and a thinner anterior region. Three smaller, paired cartilages—the arytenoids, corniculates, and cuneiforms—attach to the epiglottis and the vocal cords and muscles that help move the vocal cords to produce speech.
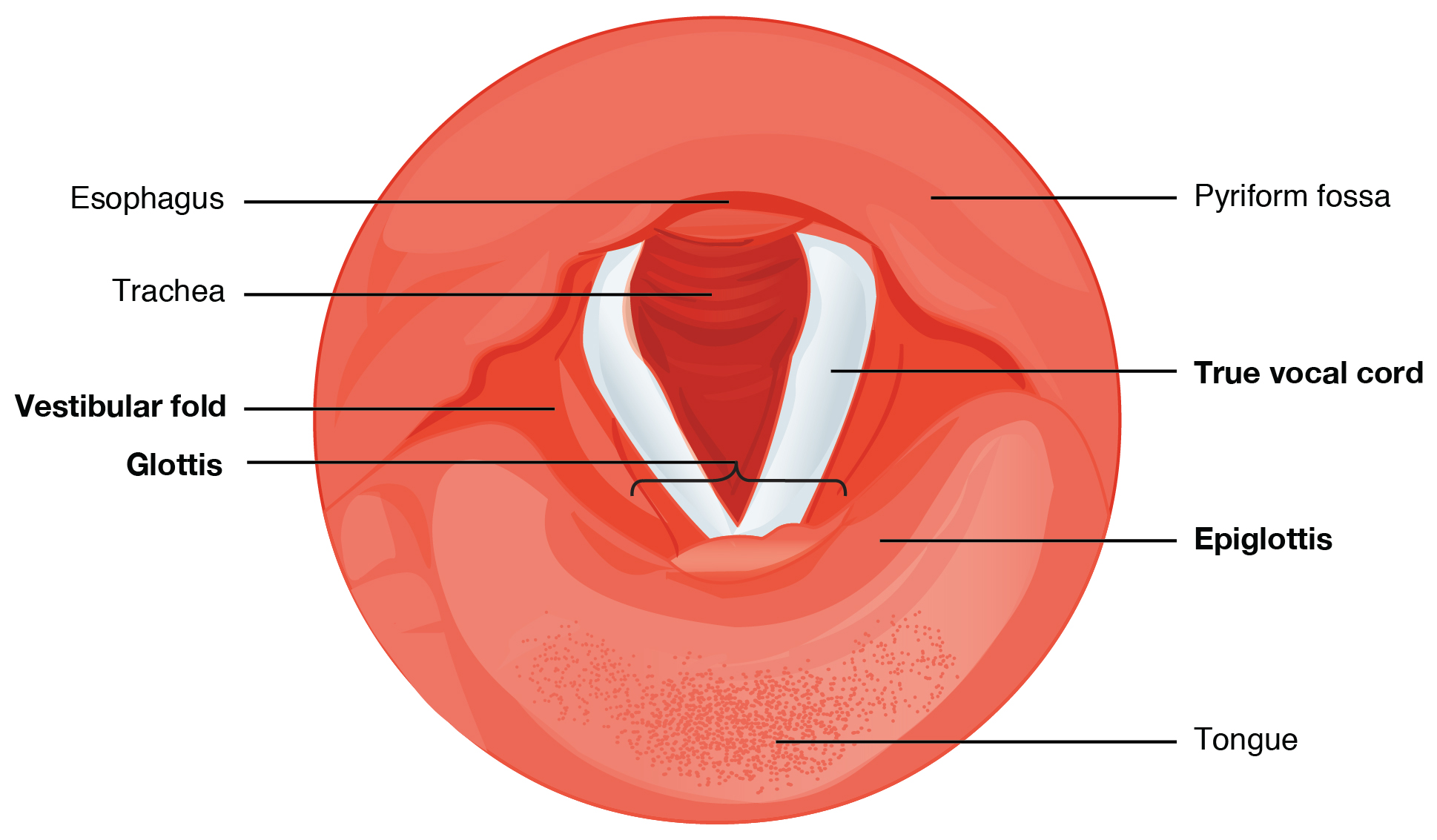
Larynx
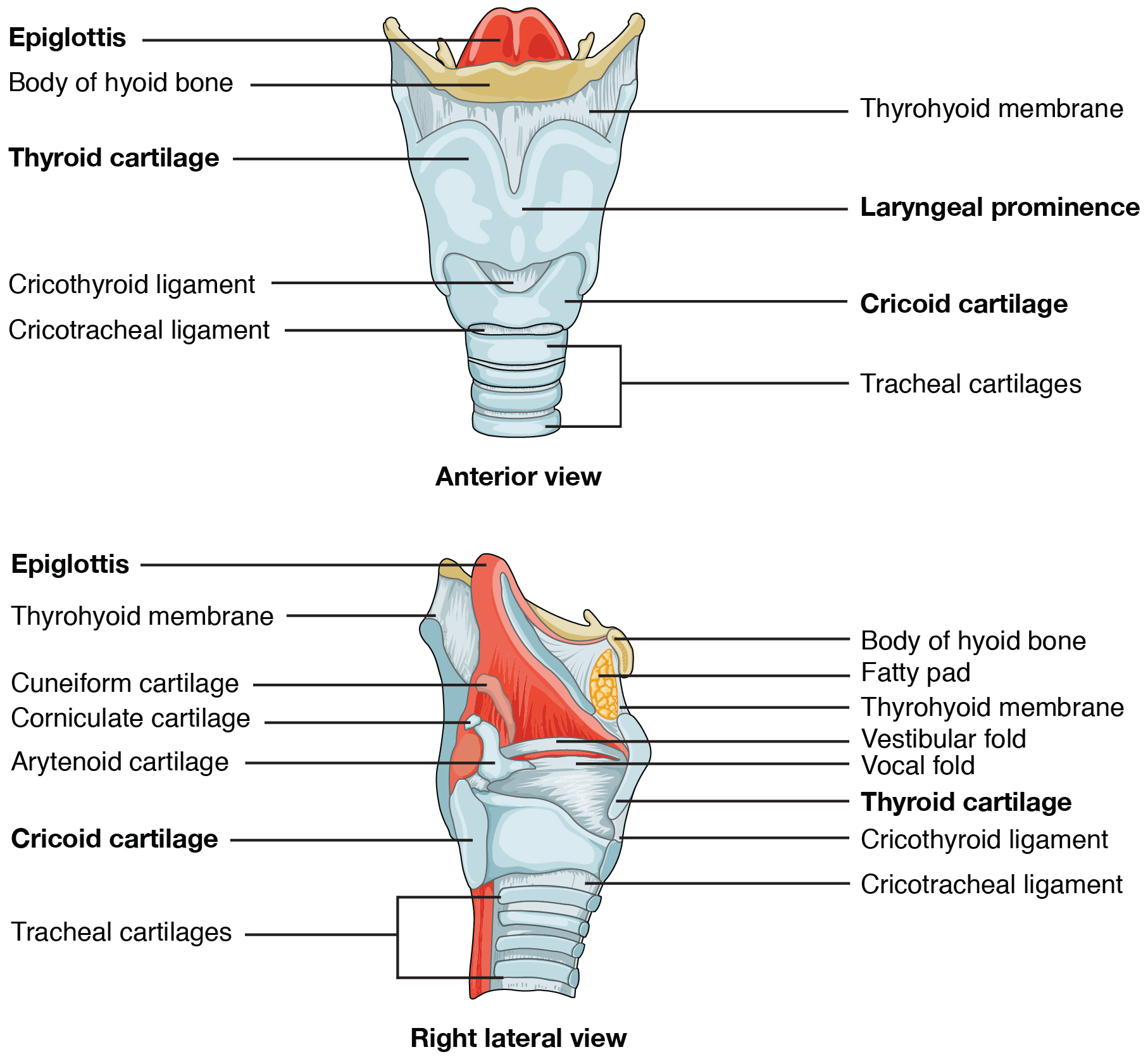
The epiglottis, attached to the thyroid cartilage, is a very flexible piece of elastic cartilage that covers the opening of the trachea. When in the “closed” position, the unattached end of the epiglottis rests on the glottis. The glottis is composed of the vestibular folds, the vocal folds, and the space between these folds. The vestibular folds, or false vocal cords, are a pair of folded sections of mucous membrane. The vocal folds or true vocal cords are the white, membranous folds attached by muscle to the thyroid and arytenoid cartilages of the larynx on their outer edges. The inner edges of the true vocal cords are free, allowing oscillation to produce sound. The size of the membranous folds of the true vocal cords differs between individuals, producing voices with different pitch ranges. Folds in males tend to be larger than those in females, which creates a deeper voice. The act of swallowing causes the pharynx and larynx to lift upward, allowing the pharynx to expand and the epiglottis of the larynx to swing downward, closing the opening to the trachea. These movements produce a larger area for food to pass through while preventing food and beverages from entering the trachea.
Vocal Cords
Continuous with the laryngopharynx, the superior portion of the larynx is lined with stratified squamous epithelium, transitioning into pseudostratified ciliated columnar epithelium that contains goblet cells. Similar to the nasal cavity and nasopharynx, this specialized epithelium produces mucus to trap debris and pathogens as they enter the trachea. The cilia beat the mucus upward towards the laryngopharynx, where it can be swallowed down the esophagus.
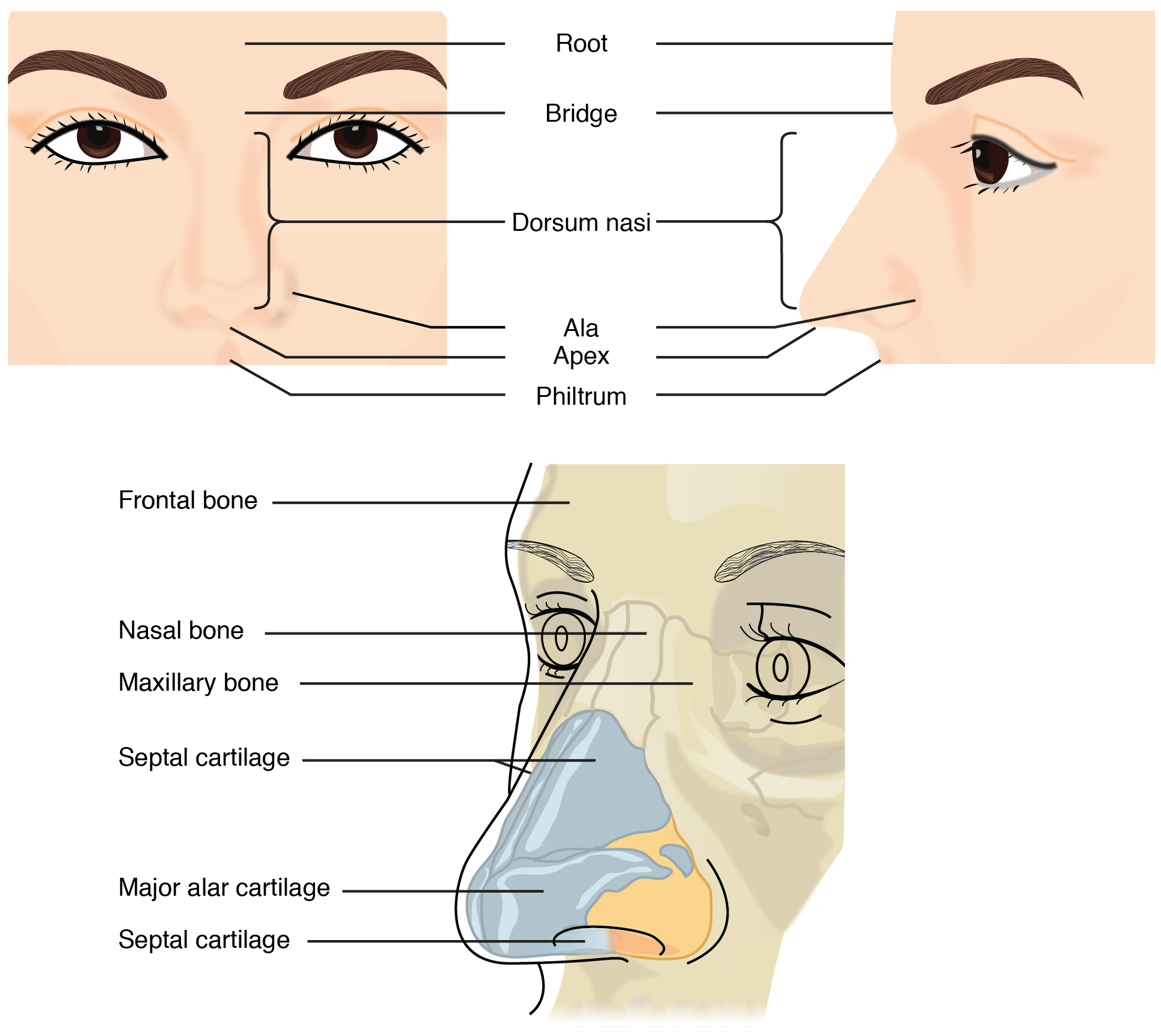
The Nasal Cavity
The nose and nasal cavity function as part of the respiratory system. While the root and bridge of the nose consist of bone, the protruding portion of the nose is composed of cartilage. As a result, when looking at a skull, the nose is missing. The nasal bones lie under the root and bridge of the nose. The nasal bone articulates superiorly with the frontal bone and laterally with the maxillary bones. The alar cartilage forms the apex, or anterior portion, of the nose surrounding the nares, or nostrils. The nasal septum separates the right and left sides of the nasal cavity. The nasal septum is formed anteriorly by a portion of the septal cartilage (the flexible portion you can touch with your fingers) and posteriorly by the perpendicular plate of the ethmoid bone and the thin vomer bone. The floor of the nasal cavity is formed by the maxillary and palatine bones, while the posterior wall is formed by the sphenoid bone.
Each lateral wall of the nasal cavity has three bony projections, called the superior, middle, and inferior nasal conchae. The inferior nasal conchae are separate bones, whereas the superior and middle conchae are portions of the ethmoid bone. The superior, middle, and inferior nasal meatuses are the spaces located inferior to the concha of the same name. The conchae serve to increase the surface area of the nasal cavity and to disrupt the flow of air as it enters the nose, causing air to bounce along the epithelium, where it is cleaned and warmed.
Paranasal Sinuses
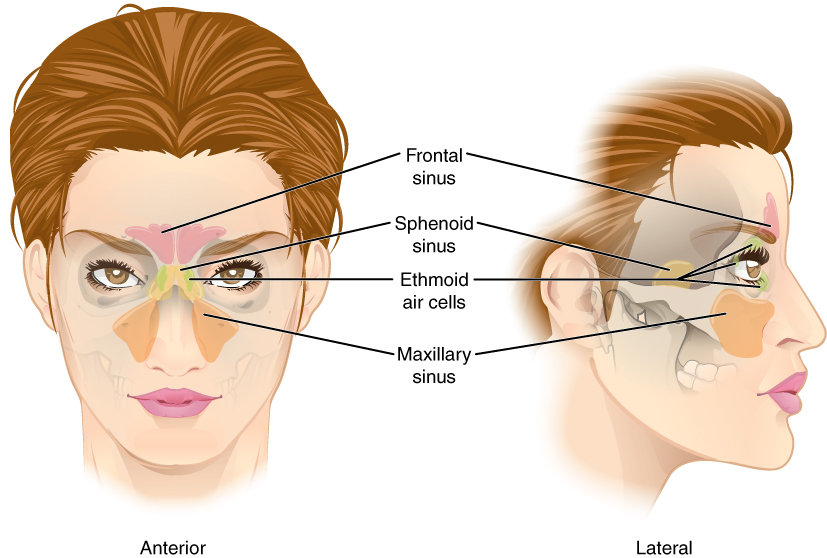
The paranasal sinuses are hollow, air-filled spaces located within certain bones of the skull. All of the sinuses communicate with the nasal cavity (paranasal = “next to nasal cavity”) and are lined with nasal mucosa. They serve to reduce bone mass and thus lighten the skull, condition and warm the air that swirls through them, and add resonance to the voice.
The paranasal sinuses are named for the skull bone that each occupies. The frontal sinus is located just above the eyebrows, within the frontal bone. The frontal sinus is the most anterior of the paranasal sinuses. The largest sinus is the maxillary sinus. These are paired and located within the right and left maxillary bones, where they occupy the area just below the orbits. The sphenoid sinus is a single, midline sinus. It is located within the body of the sphenoid bone, making it the most posterior of the paranasal sinuses. The lateral aspects of the ethmoid bone contain multiple small spaces separated by very thin bony walls. The ethmoid air cells are multiple small spaces located in the right and left sides of the ethmoid bone, between the medial wall of the orbit and lateral wall of the upper nasal cavity.
Sinuses – Fun Fact (->you will not be assessed on this content)
The maxillary sinuses are most commonly involved during sinus infections. Because their connection to the nasal cavity is located high on their medial wall, they are difficult to drain.
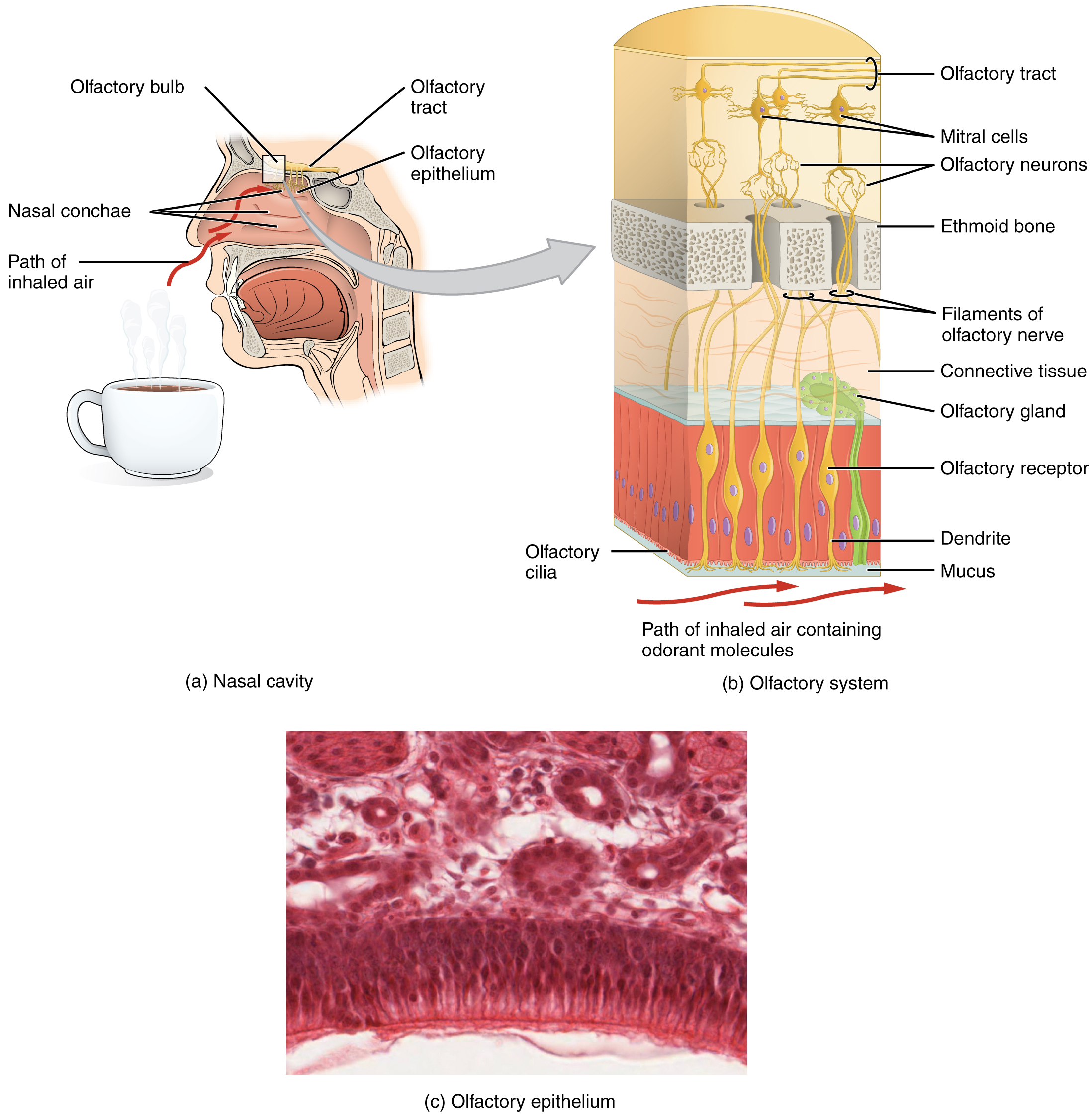
Olfaction (Smell)
Olfaction, or the sense of smell, is responsive to chemical stimuli. The olfactory receptor neurons are located in a small region within the superior nasal cavity. This region is referred to as the olfactory epithelium and contains bipolar sensory neurons. Each olfactory sensory neuron has dendrites, called olfactory hairs or olfactory cilia, that extend from the apical surface of the epithelium into the mucus layer lining the cavity. As airborne molecules are inhaled through the nose, they pass over the olfactory epithelial region and dissolve into the mucus and are sensed by the olfactory receptor cells.
The axon of an olfactory receptor neuron extends from the basal surface of the epithelium, through the cribriform plate foramina of the ethmoid bone, and into the brain. They synapse in the olfactory bulb, which sits just superior to the cribriform plate foramina. From the olfactory bulb, axons of the second neuron in the pathway form the olfactory tract and travel posteriorly on the inferior aspect of the frontal lobe. Most of these axons travel to the primary olfactory cortex, which processes the olfactory information to give us the conscious experience of smell. The primary olfactory cortex is located in the superomedial areas of the temporal lobe.