Module 6: Articulations
Learning Objectives:
By the end of this module, students will be able to:
- Compare and contrast the axial and the appendicular regions.
- Describe how structure governs function with joints.
- Identify the different types of joints by structural and functional classifications.
- Explain the different components of synovial joints.
- Describe movements around joints with respect to their planes and axes.
- Contrast the various movements that muscles produce around joints.
Terms to Know
|
Bones
**You do not need to identify the italicized terms. You should have a basic understanding of them for this unit.** Articulations
|
Articulations (continued)
|
Introduction – A review of bone growth
This content will not be covered in lecture.
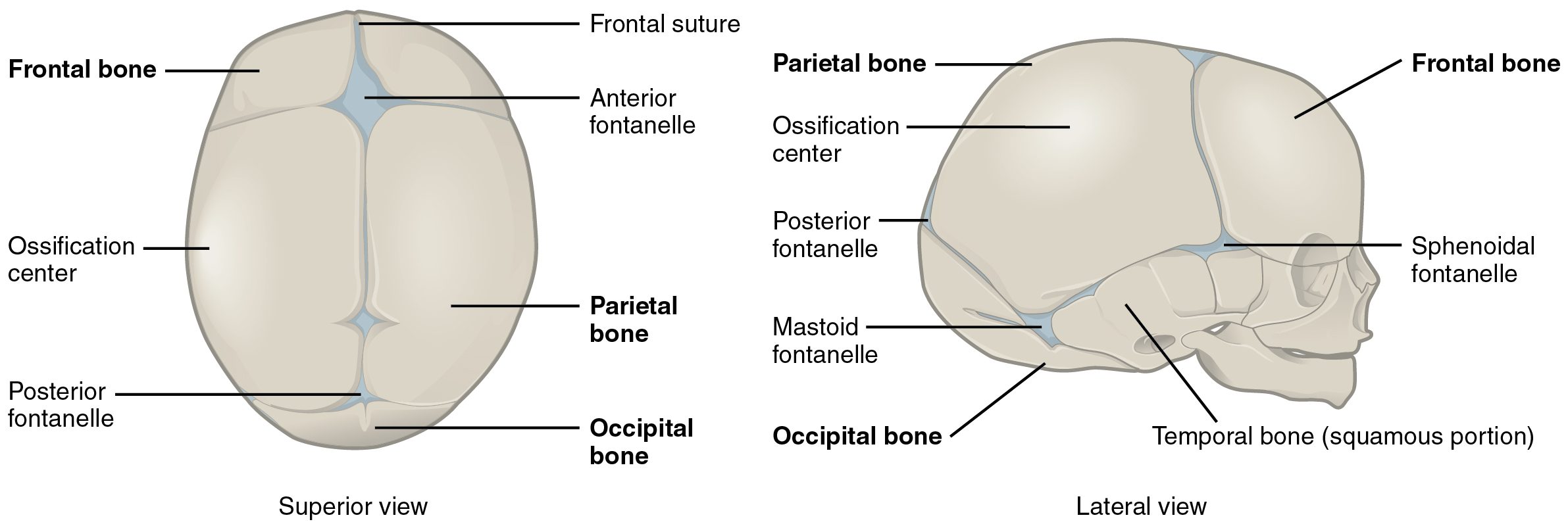
Joints form during embryonic development in conjunction with the formation and growth of the associated bones. The embryonic tissue that gives rise to all bones, cartilages, and connective tissues of the body is called mesenchyme. In the head, mesenchyme will accumulate at those areas that will become the bones that form the top and sides of the skull. The mesenchyme in these areas will develop directly into bone through the process of intramembranous ossification, in which mesenchymal cells differentiate into bone-producing cells that then generate bone tissue. The mesenchyme between the areas of bone production will become the fibrous connective tissue that fills the spaces between the developing bones. Initially, the connective tissue-filled gaps between the bones are wide and are called fontanelles. After birth, as the skull bones grow and enlarge, the gaps between them decrease in width, and the fontanelles are reduced to suture joints in which the bones are united by a narrow layer of fibrous connective tissue.
The bones that form the base and facial regions of the skull develop through endochondral ossification. In this process, mesenchyme accumulates and differentiates into hyaline cartilage, which forms a model of the future bone. The hyaline cartilage model is then gradually, over a period of many years, displaced by bone. The mesenchyme between these developing bones becomes the fibrous connective tissue of the suture joints between the bones in these regions of the skull.
A similar process of endochondral ossification gives rise to the bones and joints of the limbs. The limbs initially develop as small limb buds that appear on the sides of the embryo around the end of the fourth week of development. Starting during the sixth week, as each limb bud continues to grow and elongate, areas of mesenchyme within the bud begin to differentiate into the hyaline cartilage that will form models for each of the future bones. The synovial joints will form between the adjacent cartilage models in an area called the joint interzone. Cells at the center of this interzone region undergo cell death to form the joint cavity, while surrounding mesenchyme cells form the articular capsule and supporting ligaments. Endochondral ossification, which converts the cartilage models into bone, begins by the twelfth week of embryonic development. At birth, ossification of much of the bone has occurred, but the hyaline cartilage of the epiphyseal plate will remain throughout childhood and adolescence to allow for bone lengthening. Hyaline cartilage is also retained as the articular cartilage that covers the surfaces of the bones at synovial joints.
The skeletal system includes all of the bones, cartilages, and ligaments of the body that support and give shape to the body and body structures. The skeleton consists of the bones of the body. For adults, there are 206 bones in the skeleton. Younger individuals have higher numbers of bones because some bones fuse during childhood and adolescence to form an adult bone. The primary functions of the skeleton are to provide a rigid, internal structure that can support the weight of the body against the force of gravity and provide a structure upon which muscles can act to produce movements of the body. The lower portion of the skeleton is specialized for stability during walking or running. In contrast, the upper skeleton has greater mobility and ranges of motion, features that allow you to lift and carry objects or turn your head and trunk.
In addition to providing for support and movements of the body, the skeleton has protective and storage functions. It protects the internal organs, including the brain, spinal cord, heart, lungs, and pelvic organs. The bones of the skeleton serve as the primary storage site for important minerals such as calcium and phosphate. The bone marrow found within bones stores fat and houses the blood-cell producing tissue of the body.
The Axial and Appendicular Skeleton
This content is introduced in the assignment and will be reviewed and built upon in lecture.
The skeleton is subdivided into two major divisions—the axial and appendicular.
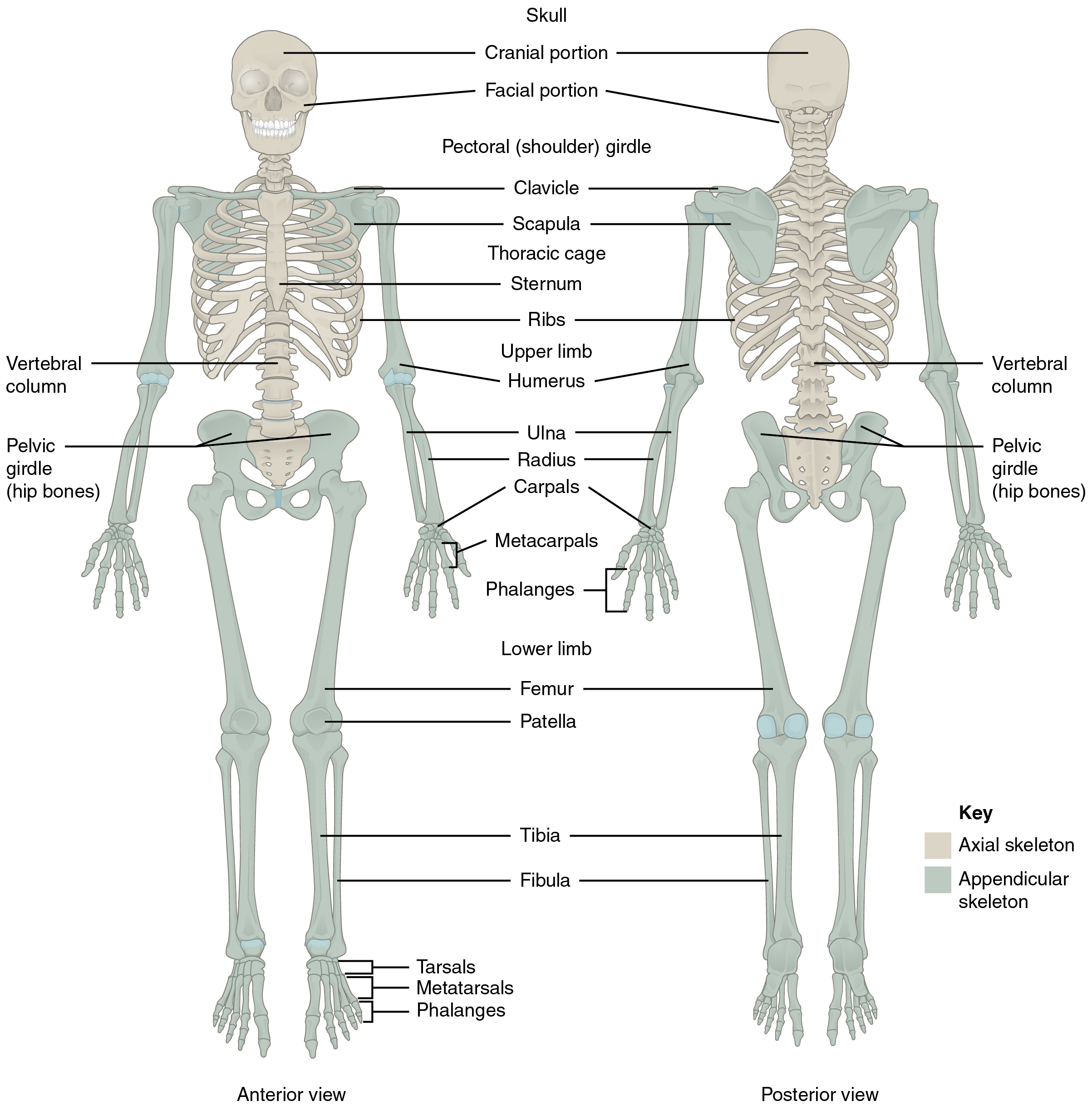
The Axial Skeleton
The axial skeleton forms the vertical, central axis of the body and includes all bones of the head, neck, chest, and back. It serves to protect the brain, spinal cord, heart, and lungs. It also serves as the attachment site for muscles that move the head, neck, and back, and muscles that act across the shoulder and hip joints to move their corresponding limbs.
The axial skeleton of the adult consists of 80 bones, including the skull, the vertebral column, and the thoracic cage. The skull is formed by 22 bones. Also associated with the head are an additional seven bones, including the hyoid bone and the ear ossicles (three small bones found in each middle ear). The vertebral column consists of 24 bones; each called a vertebra, plus the sacrum and coccyx. The thoracic cage includes the 12 pairs of ribs, and the sternum, the flattened bone of the anterior chest.
The Appendicular Skeleton
The appendicular skeleton includes all bones of the upper and lower limbs, plus the bones that attach each limb to the axial skeleton. There are 126 bones in the appendicular skeleton of an adult.
Bony Markings
This content is covered in the pre-lecture assignment and will not be covered during lecture.
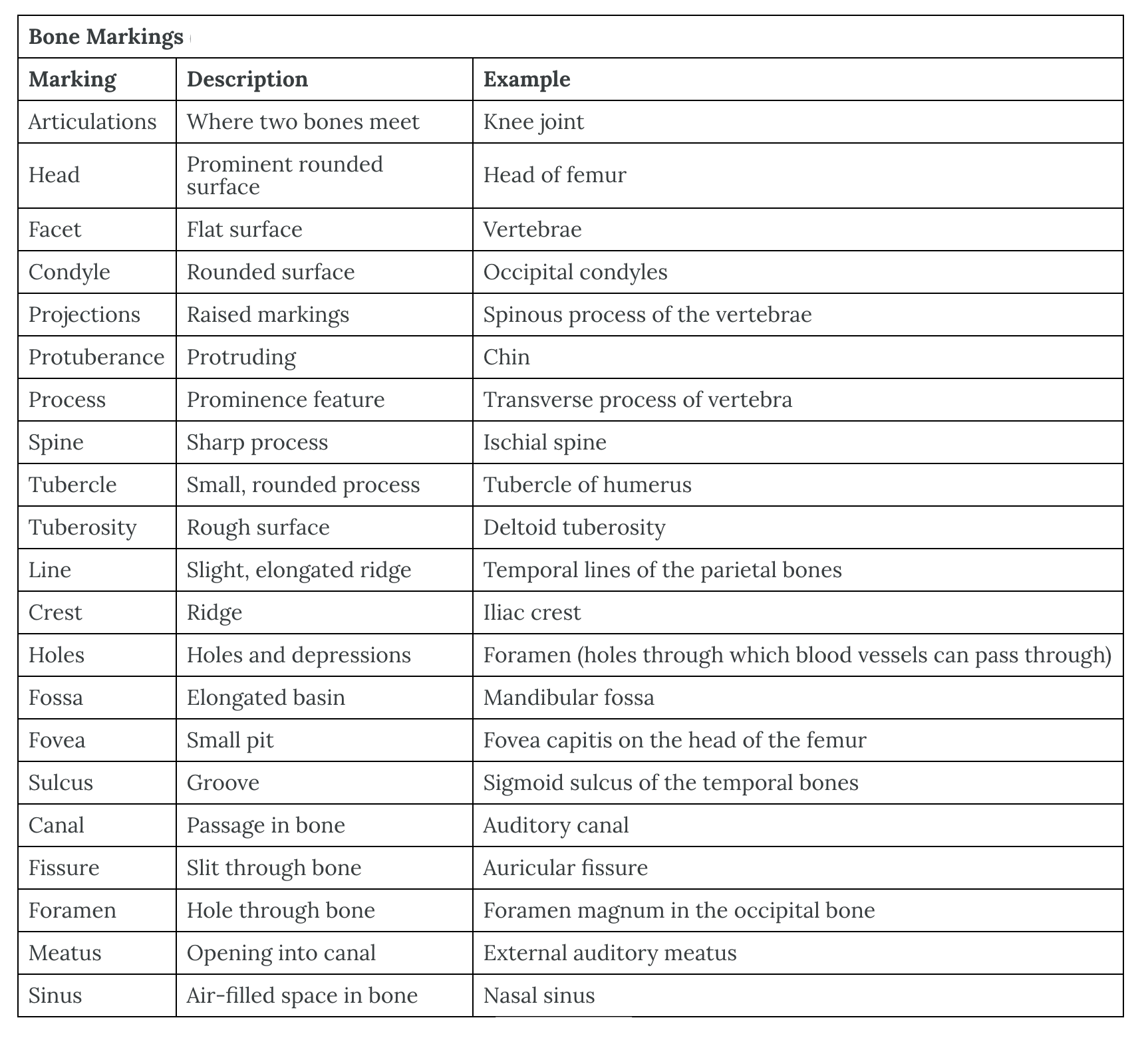
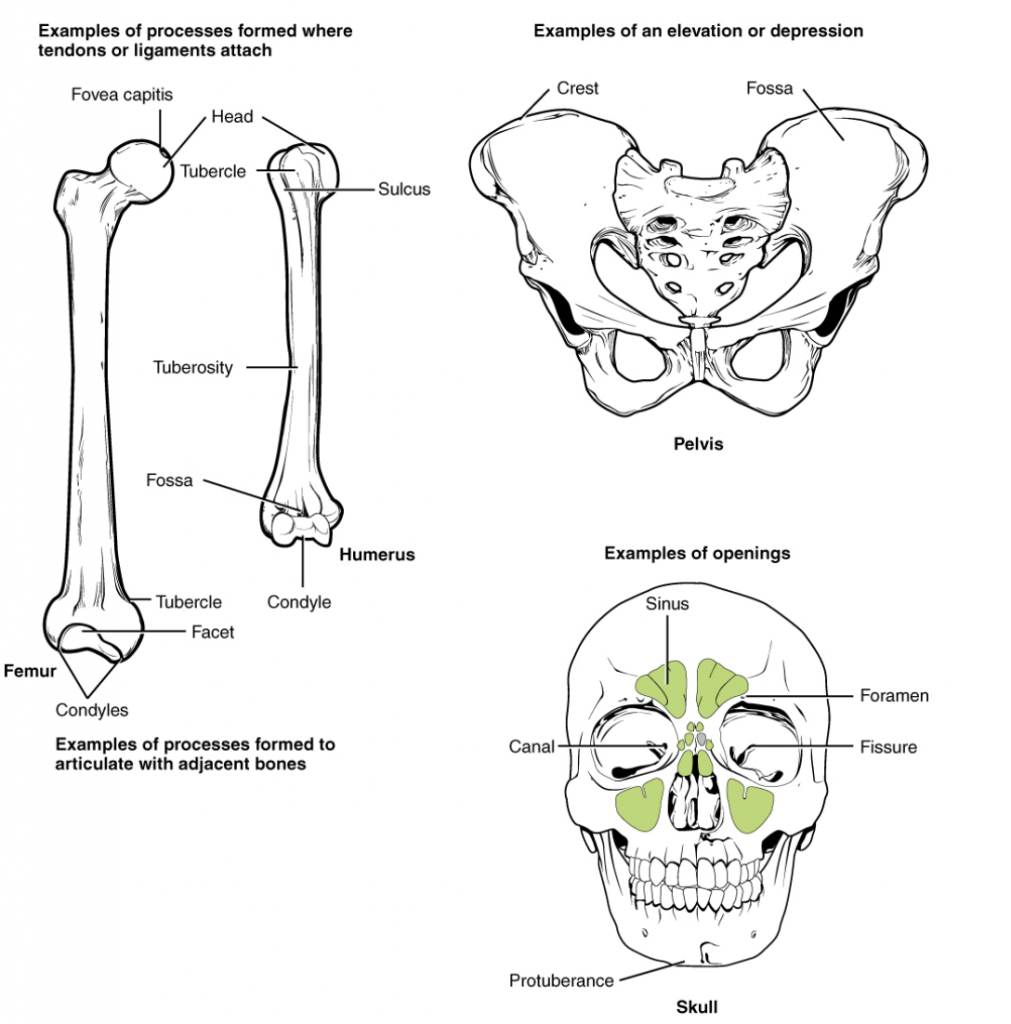
The surface features of bones vary considerably, depending on the function and location in the body. There are general classes of bone markings; articulations, attachments/projections, depressions, and openings. As the name implies, an articulation is where two bone surfaces come together (articulus = “joint”). These surfaces tend to conform to one another, such as one being rounded and the other cupped, to facilitate the function of the articulation. An attachment is an area of a bone that projects above the surface of the bone. These are the attachment points for tendons and ligaments. In general, their size and shape is an indication of the forces exerted through the attachment to the bone. Depressions are grooves where blood vessels and nerves pass on the surface of a bone. Openings allow blood vessels and nerves to enter the bone or pass through the bone. As with the other markings, their size and shape reflect the size of the vessels and nerves that penetrate the bone at these points.
Articulations
This content is introduced in the assignment and will be reviewed and built upon during lecture.
The adult human body has 206 bones, and except for the hyoid bone in the neck, each bone is connected to at least one other bone. Joints are the location where bones come together. Many joints allow for movement between the bones. At these joints, the articulating surfaces of the adjacent bones can move smoothly against each other. However, the bones of other joints may be joined to each other by connective tissue or cartilage. These joints are designed for stability and provide for little or no movement. Importantly, joint stability and movement are related to each other. This means that stable joints allow for little or no mobility between the adjacent bones. Conversely, joints that provide the most movement between bones are the least stable. Understanding the relationship between joint structure and function will explain why particular types of joints are found in certain areas of the body.
The articulating surfaces of bones at stable types of joints, with little or no mobility, are strongly united to each other. For example, most of the joints of the skull are held together by fibrous connective tissue and do not allow for movement between the adjacent bones. This lack of mobility is important because the skull bones serve to protect the brain. Similarly, other joints united by fibrous connective tissue allow for minimal movement, which provides stability and weight-bearing support for the body. For example, the tibia and fibula of the leg are tightly united to give stability to the body when standing. At other joints, the bones are held together by cartilage, which permits limited movements between the bones. Thus, the joints of the vertebral column only allow for small movements between adjacent vertebrae, but when added together, these movements provide the flexibility that allows your body to twist or bend to the front, back, or side. In contrast, at joints that allow for wide ranges of motion, the articulating surfaces of the bones are not directly united to each other. Instead, these surfaces are enclosed within a space filled with lubricating fluid, which allows the bones to move smoothly against each other. These joints provide greater mobility, but since the bones are free to move in relation to each other, the joint is less stable. Most of the joints between the bones of the appendicular skeleton are this freely moveable type of joint. These joints allow the muscles of the body to pull on a bone and thereby produce movement of that body region. Your ability to kick a soccer ball, pick up a fork, and dance the tango depends on mobility at these types of joints.
Functional Classification of Joints
The functional classification of joints is determined by the amount of mobility found between the adjacent bones. Joints are thus functionally classified as a synarthrosis or immobile joint, an amphiarthrosis or slightly moveable joint, or as a diarthrosis, which is a freely moveable joint (arthroun = “to fasten by a joint”). Depending on their location, fibrous and cartilaginous joints may be functionally classified as a synarthrosis (immobile joint) or an amphiarthrosis (slightly mobile joint). All synovial joints are functionally classified as a diarthrosis joint.
Synarthrosis
An immobile or nearly immobile joint is called a synarthrosis. The immobile nature of these joints provides for a strong union between the articulating bones. This is important at locations where the bones provide protection for internal organs. Examples include sutures, the fibrous joints between the bones of the skull that surround and protect the brain, and the manubriosternal joint, the cartilaginous joint that unites the manubrium and body of the sternum for protection of the heart.
Key Takeaways
Synarthrosis (functional classification)
- An immobile or nearly immobile joint
- Examples include:
- Some fibrous joints (structural classification)
- Sutures
- Gomphosis
- Some cartilaginous joints (structural classification)
- Synchondrosis
- Some fibrous joints (structural classification)
- Examples include:
Amphiarthrosis
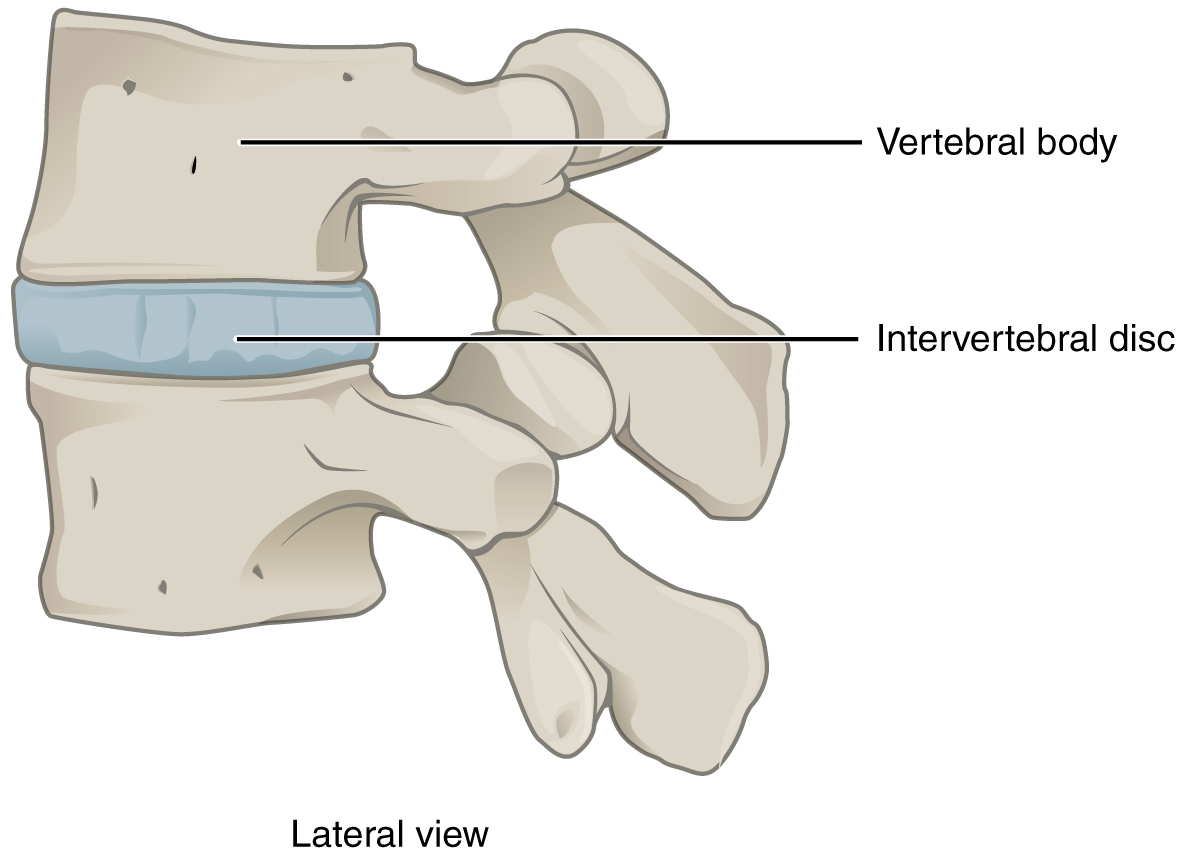
An amphiarthrosis is a joint that has limited mobility. An example of this type of joint is the cartilaginous joint that unites the bodies of adjacent vertebrae. Filling the gap between the vertebrae is a thick pad of fibrocartilage called an intervertebral disc. Each intervertebral disc strongly unites the vertebrae but still allows for a limited amount of movement between them. However, the small movements available between adjacent vertebrae can sum together along the length of the vertebral column to provide for large ranges of body movements.
Another example of an amphiarthrosis is the pubic symphysis of the pelvis. This is a cartilaginous joint in which the pubic regions of the right and left hip bones are strongly anchored by fibrocartilage. This joint normally has very little mobility. The strength of the pubic symphysis is important in conferring weight-bearing stability to the pelvis.
Key Takeaways
Amiphiarthrosis (functional classification)
- A joint with limited mobility
- Examples include:
- Some fibrous joints (structural classification)
- Syndesmosis
- Some cartilaginous joints (structural classification)
- Symphysis
- Some fibrous joints (structural classification)
- Examples include:
Diarthrosis
A freely mobile joint is classified as a diarthrosis. These joints include all synovial joints of the body, which provide the majority of body movements. Most diarthrotic joints are found in the appendicular skeleton, giving the limbs a wide range of motion. These joints are divided into categories, based on the number of axes of motion provided by each. An axis in anatomy is described as the movements about the three anatomical planes: transverse, frontal (coronal), and sagittal. Thus, diarthroses are classified as nonaxial (do not move about a plane), uniaxial (for movement in one plane), biaxial (for movement in two planes), or multiaxial joints (for movement in all three anatomical planes).
A uniaxial joint only allows for a motion in a single plane (around a single axis). The elbow joint, which only allows for bending or straightening, is an example of a uniaxial joint. A biaxial joint allows for motions within two planes. An example of a biaxial joint is a metacarpophalangeal joint (knuckle joint) of the hand. The joint allows for movement along one axis to produce bending or straightening of the finger, and movement along a second axis, which allows for spreading of the fingers away from each other and bringing them together. A joint that allows for several directions of movement is called a multiaxial joint (polyaxial or triaxial joint). This type of diarthrotic joint allows for movement along three axes. The shoulder and hip joints are multiaxial joints. They allow the upper or lower limb to move in an anterior-posterior direction and a medial-lateral direction. In addition, the limb can also be rotated around its long axis. This third movement results in rotation of the limb so that its anterior surface is moved either toward or away from the midline of the body.
Key Takeaways
Diarthrosis (functional classification)
- A freely mobile joint
- Examples include:
- Synovial joints (structural classification)
- Examples include:
Structural Classification of Joints
The structural classification of joints is based on whether the articulating surfaces of the adjacent bones are directly connected by fibrous connective tissue or cartilage or whether the articulating surfaces contact each other within a fluid-filled joint cavity. These differences serve to divide the joints of the body into three structural classifications. A fibrous joint is where the adjacent bones are united by fibrous connective tissue. At a cartilaginous joint, the bones are joined by hyaline cartilage or fibrocartilage. At a synovial joint, the articulating surfaces of the bones are not directly connected but instead come into contact with each other within a joint cavity that is filled with a lubricating fluid. Synovial joints (discussed under diarthrosis joints) allow for free movement between the bones and are the most common joints of the body. We will classify joints functionally and sub-classify the structural features of joints for this course.
Fibrous Joints
At a fibrous joint, the adjacent bones are directly connected by fibrous connective tissue, and thus the bones do not have a joint cavity between them. The gap between the bones may be narrow or wide. There are three types of fibrous joints. A suture is the narrow fibrous joint found between most bones of the skull. At a syndesmosis joint, the bones are more widely separated but are held together by a narrow band of fibrous connective tissue called a ligament, or a wide sheet of connective tissue called an interosseous membrane. This type of fibrous joint is found between the shaft regions of the long bones in the forearm and the leg. Lastly, a gomphosis is the narrow fibrous joint between the roots of a tooth and the bony socket in the jaw into which the tooth fits.
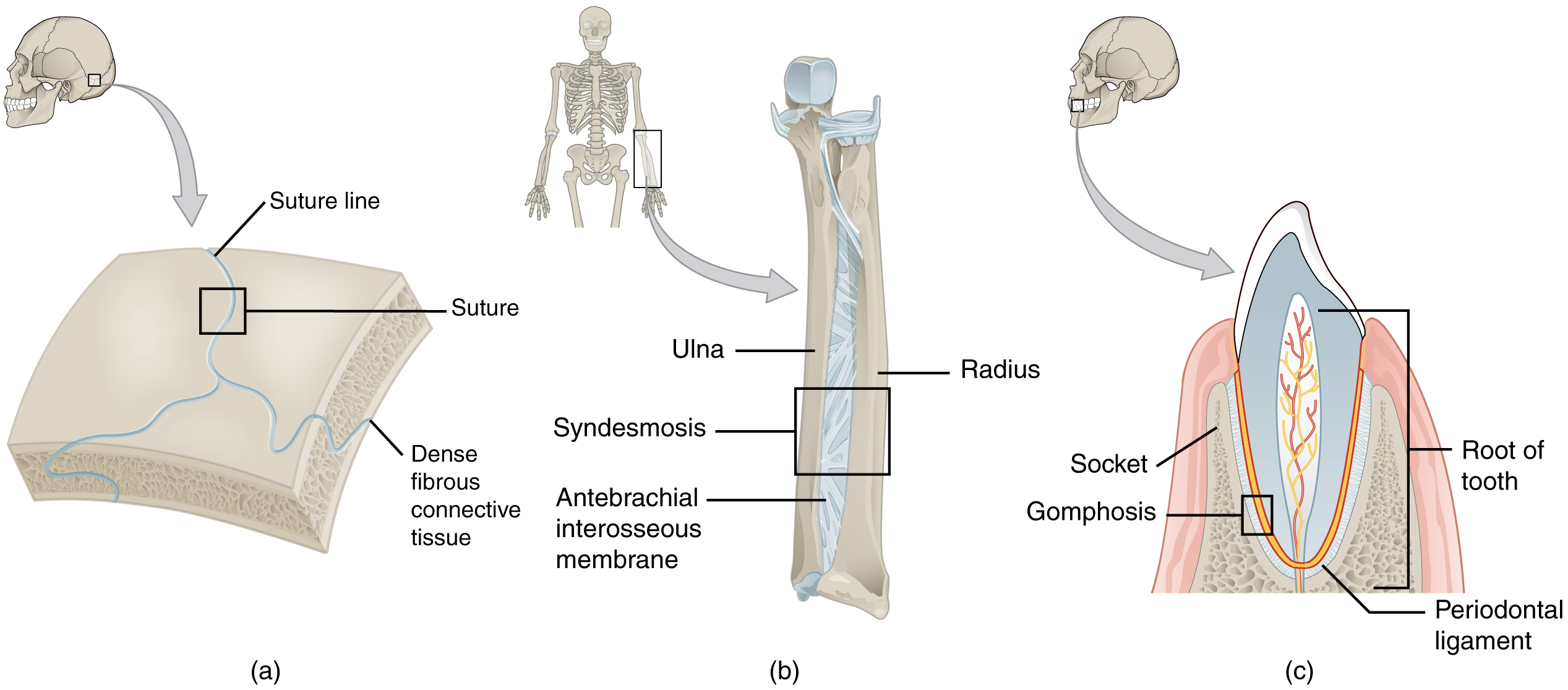
Suture
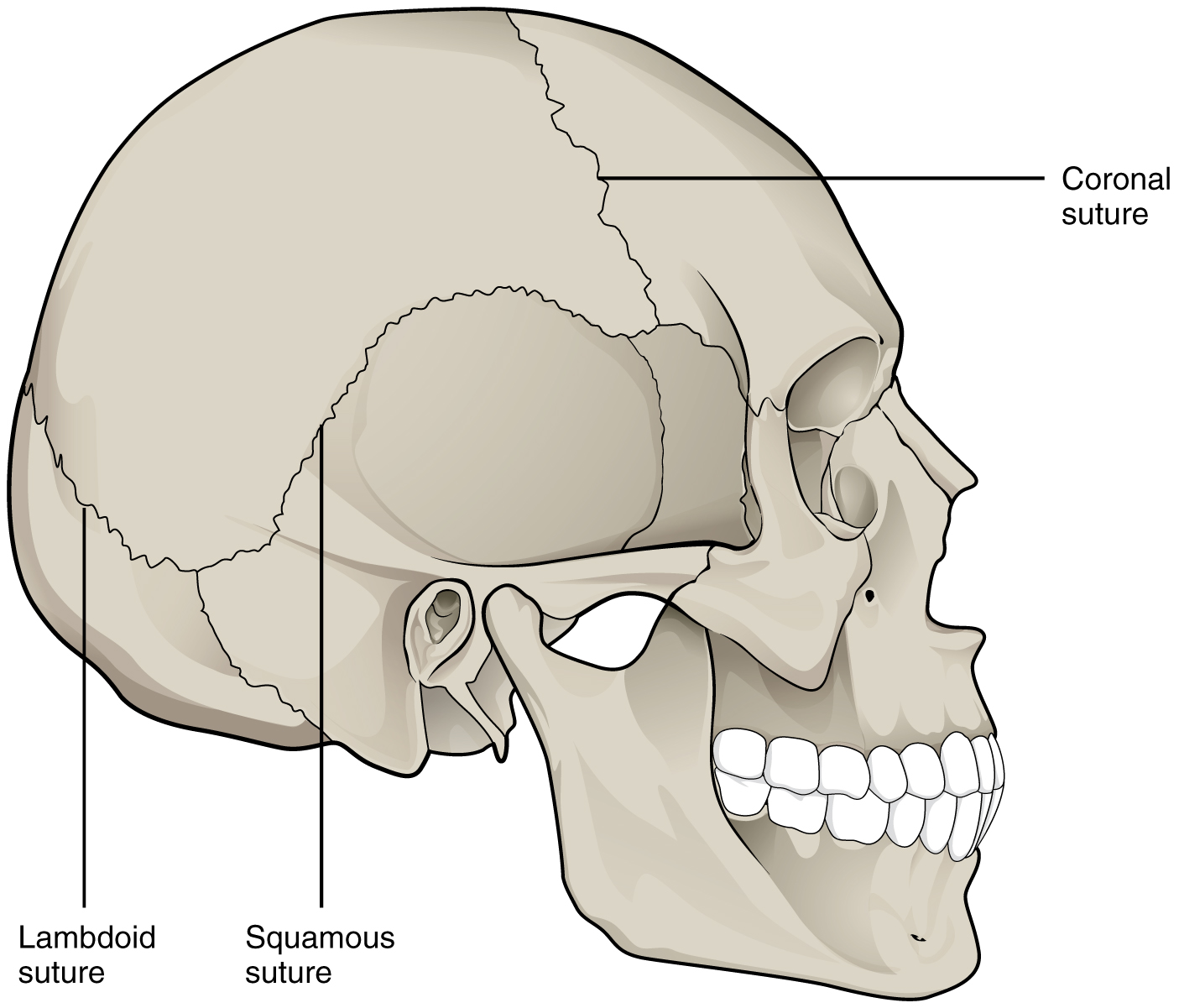
All the bones of the skull, except for the mandible, are joined to each other by a fibrous joint called a suture. The fibrous connective tissue found at a suture (“to bind or sew”) strongly unites the adjacent skull bones and thus helps to protect the brain and form the face. In adults, the skull bones are closely opposed, and fibrous connective tissue fills the narrow gap between the bones. The suture is frequently convoluted, forming a tight union that prevents most movement between the bones. Thus, skull sutures are functionally classified as a synarthrosis, although some sutures may allow slight movements between the cranial bones.
In newborns and infants, the areas of connective tissue between the bones are much wider, especially in those areas on the top and sides of the skull that will become the sagittal, coronal, squamous, and lambdoid sutures. These broad areas of connective tissue are called fontanelles. During birth, the fontanelles provide flexibility to the skull, allowing the bones to push closer together or to overlap slightly, thus aiding the movement of the infant’s head through the birth canal. After birth, these expanded regions of connective tissue allow for the rapid growth of the skull and enlargement of the brain. The fontanelles greatly decrease in width during the first year after birth as the skull bones enlarge. When the connective tissue between the adjacent bones is reduced to a narrow layer, these fibrous joints are now called sutures. At some sutures, the connective tissue will ossify and be converted into bone, causing the adjacent bones to fuse. Late in life, the sagittal, coronal, and lambdoid sutures of the skull will begin to ossify and fuse, causing the suture line to gradually disappear.
Syndesmosis
A syndesmosis (“fastened with a band”) is a type of fibrous joint in which two parallel bones are united to each other by fibrous connective tissue. The gap between the bones may be narrow, with the bones joined by ligaments, or the gap may be wide and filled in by a broad sheet of connective tissue called an interosseous membrane.
In the forearm, the wide gap between the shaft portions of the radius and ulna bones are strongly united by an interosseous membrane. Similarly, in the leg, the shafts of the tibia and fibula are also united by an interosseous membrane. In addition, at the distal tibiofibular joint, the articulating surfaces of the bones lack cartilage, and the narrow gap between the bones is anchored by fibrous connective tissue and ligaments on both the anterior and posterior aspects of the joint. Together, the interosseous membrane and these ligaments form the tibiofibular syndesmosis.
The syndesmoses found in the forearm and leg serve to unite parallel bones and prevent their separation. However, a syndesmosis does not prevent all movement between the bones, and thus this type of fibrous joint is functionally classified as an amphiarthrosis. In the leg, the syndesmosis between the tibia and fibula strongly unites the bones, allows for little movement, and firmly locks the talus bone in place between the tibia and fibula at the ankle joint. This provides strength and stability to the leg and ankle, which are important during weight-bearing. In the forearm, the interosseous membrane is flexible enough to allow for rotation of the radius bone during forearm movements. Thus, in contrast to the stability provided by the tibiofibular syndesmosis, the flexibility of the antebrachial interosseous membrane allows for the much greater mobility of the forearm.
The interosseous membranes of the leg and forearm also provide areas for muscle attachment. Damage to a syndesmotic joint, which usually results from a fracture of the bone with an accompanying tear of the interosseous membrane, will produce pain, loss of stability of the bones, and may damage the muscles attached to the interosseous membrane. If the fracture site is not properly immobilized with a cast or splint, contractile activity by these muscles can cause improper alignment of the broken bones during healing.
Gomphosis
A gomphosis (“fastened with bolts”) is the specialized fibrous joint that anchors the root of a tooth into its bony socket within the maxillary bone (upper jaw) or mandible bone (lower jaw) of the skull. A gomphosis is also known as a peg-and-socket joint. Spanning between the bony walls of the socket and the root of the tooth are numerous short bands of dense connective tissue, each of which is called a periodontal ligament. Due to the immobility of a gomphosis, this type of joint is functionally classified as a synarthrosis.
Cartilaginous Joints
As the name indicates, at a cartilaginous joint, the adjacent bones are united by cartilage, a tough but flexible type of connective tissue. These joints lack a joint cavity and involve bones joined together by either hyaline cartilage or fibrocartilage. There are two types of cartilaginous joints. A synchondrosis is a cartilaginous joint where the bones are joined by hyaline cartilage. Also classified as a synchondrosis are places where bone is united to a cartilage structure, such as between the anterior end of a rib and the costal cartilage of the thoracic cage. The second type of cartilaginous joint is a symphysis, where the bones are joined by fibrocartilage.
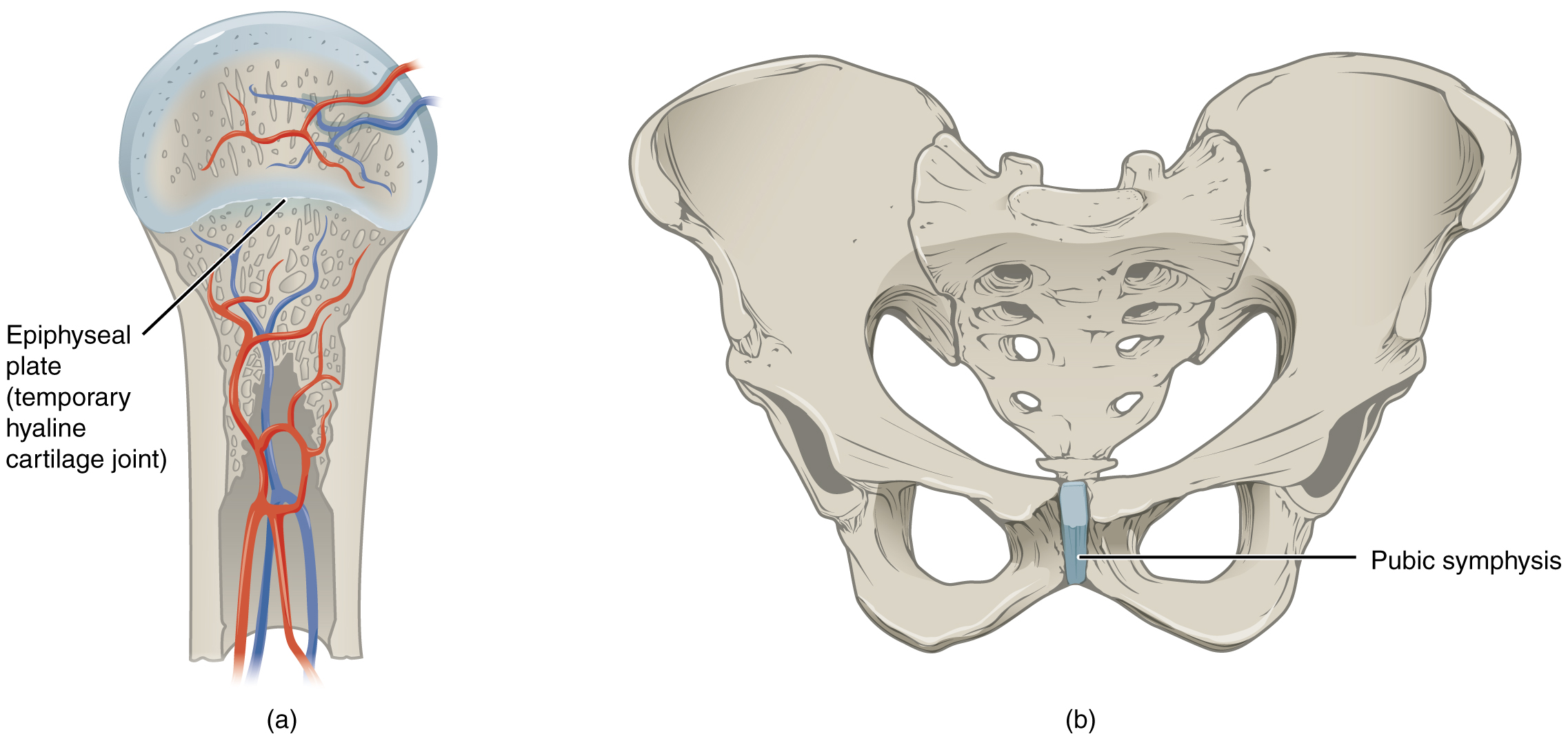
Synchondrosis
A synchondrosis (“joined by cartilage”) is a cartilaginous joint where bones are joined together by hyaline cartilage or where the bone is united to hyaline cartilage. A synchondrosis may be temporary or permanent. A temporary synchondrosis is the epiphyseal plate (growth plate) of a growing long bone. The epiphyseal plate is the region of growing hyaline cartilage that unites the diaphysis (shaft) of the bone to the epiphysis (end of the bone). Bone lengthening involves the growth of the epiphyseal plate cartilage and its replacement by bone, which adds to the diaphysis. For many years during childhood growth, the rates of cartilage growth and bone formation are equal, and thus, the epiphyseal plate does not change in overall thickness as the bone lengthens. During the late teens and early 20s, the growth of the cartilage slows and eventually stops. The epiphyseal plate is then completely replaced by bone, and the diaphysis and epiphysis portions of the bone fuse together to form a single adult bone. This fusion of the diaphysis and epiphysis is a synostosis. Once this occurs, bone lengthening ceases. For this reason, the epiphyseal plate is considered to be a temporary synchondrosis. Because cartilage is softer than bone tissue, injury to a growing long bone can damage the epiphyseal plate cartilage, thus stopping bone growth and preventing additional bone lengthening.
Growing layers of cartilage also form synchondroses that join together the ilium, ischium, and pubic portions of the hip bone during childhood and adolescence. When body growth stops, the cartilage disappears and is replaced by bone, forming synostoses and fusing the bony components into the single hip bone of the adult. Similarly, synostoses unite the sacral vertebrae that fuse to form the adult sacrum.
The growing bones of a child have an epiphyseal plate that forms a synchondrosis between the shaft and end of a long bone. Being less dense than bone, the area of epiphyseal cartilage is seen on this radiograph as the dark epiphyseal gaps located near the ends of the long bones, including the radius, ulna, metacarpal, and phalanx bones.
Examples of permanent synchondroses are found in the thoracic cage. One example is the first sternocostal joint, where the first rib is anchored to the manubrium by its costal cartilage. (The articulations of the remaining costal cartilages to the sternum are all synovial joints.) Additional synchondroses are formed where the anterior end of the other 11 ribs is joined to its costal cartilage. Unlike the temporary synchondroses of the epiphyseal plate, these permanent synchondroses retain their hyaline cartilage and thus do not ossify with age. Due to the lack of movement between the bone and cartilage, both temporary and permanent synchondroses are functionally classified as a synarthrosis.
Symphysis
A cartilaginous joint where the bones are joined by fibrocartilage is called a symphysis (“growing together”). Fibrocartilage is very strong because it contains numerous bundles of thick collagen fibers, giving it a much greater ability to resist pulling and bending forces than hyaline cartilage. This gives symphyses the ability to strongly unite the adjacent bones but can still allow for limited movement. Thus, a symphysis is functionally classified as an amphiarthrosis.
The gap separating the bones at a symphysis may be narrow or wide. Examples in which the gap between the bones is narrow include the pubic symphysis and the manubriosternal joint. At the pubic symphysis, the pubic portions of the right and left hip bones of the pelvis are joined together by fibrocartilage across a narrow gap. The intervertebral symphysis is a wide symphysis located between the bodies of adjacent vertebrae of the vertebral column. Here a thick pad of fibrocartilage called an intervertebral disc strongly unites the adjacent vertebrae by filling the gap between them. The width of the intervertebral symphysis is important because it allows for small movements between the adjacent vertebrae. In addition, the thick intervertebral disc provides cushioning between the vertebrae, which is important when carrying heavy objects or during high-impact activities such as running or jumping.
Synovial Joints
Synovial joints are the most common type of joint in the body. A key structural characteristic for a synovial joint that is not seen at fibrous or cartilaginous joints is the presence of a joint cavity. This fluid-filled space is the site at which the articulating surfaces of the bones contact each other. Unlike fibrous or cartilaginous joints, the articulating bone surfaces at a synovial joint are not directly connected with fibrous connective tissue or cartilage. This gives the bones of a synovial joint the ability to move smoothly against each other, allowing for increased joint mobility.
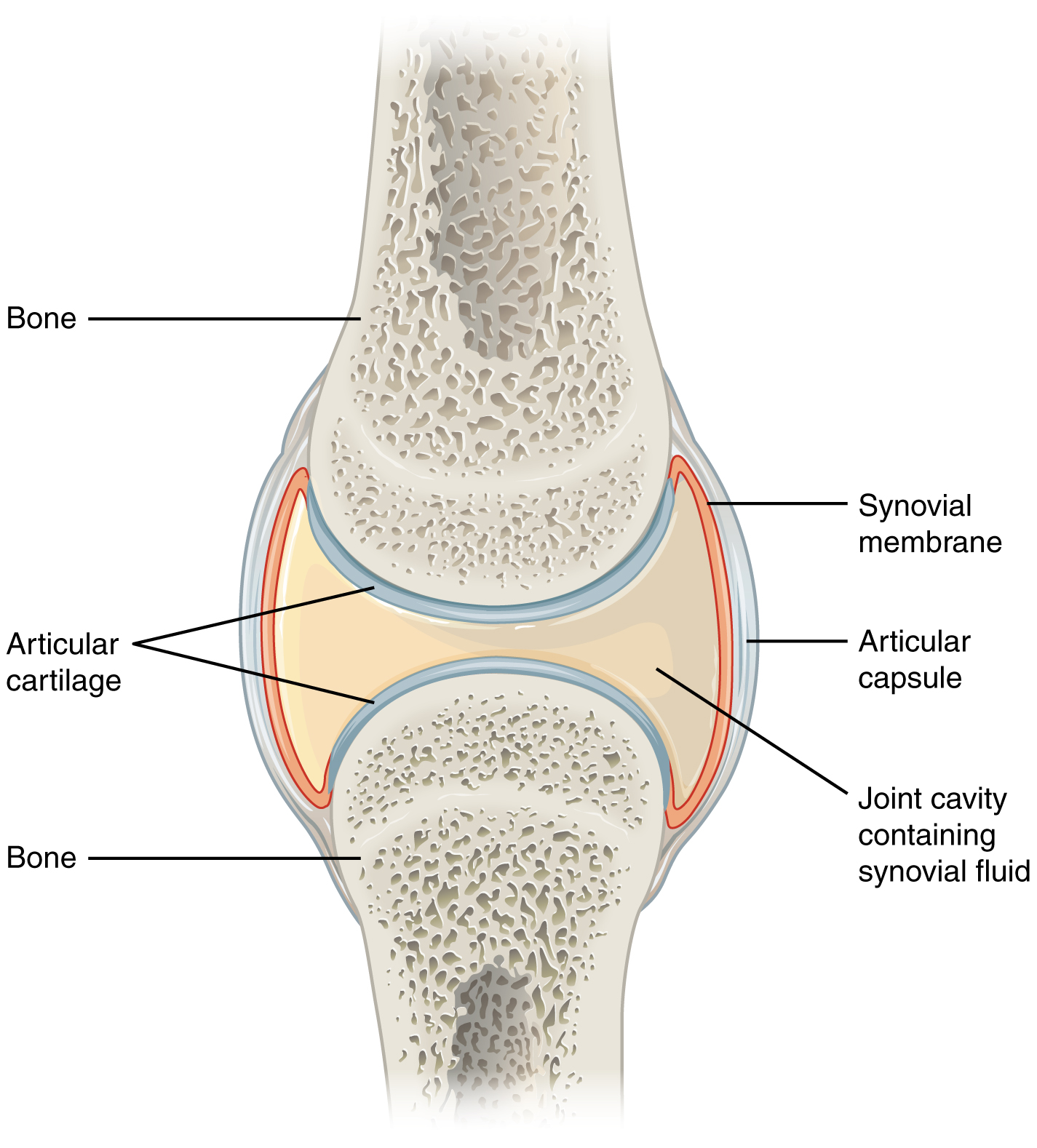
Structural Features of Synovial Joints
Synovial joints are characterized by the presence of a joint cavity. The walls of this space are formed by the articular capsule, a fibrous connective tissue structure attached to each bone just outside the area of the bone’s articulating surface. The bones of the joint articulate with each other within the joint cavity.
Friction between the bones at a synovial joint is prevented by the presence of the articular cartilage, a thin layer of hyaline cartilage that covers the entire articulating surface of each bone. However, unlike at a cartilaginous joint, the articular cartilages of each bone are not continuous with each other. Lining the inner surface of the articular capsule is a thin synovial membrane. The cells of this membrane secrete synovial fluid (synovia = “a thick fluid”), a thick, slimy fluid that provides lubrication to further reduce friction between the bones of the joint. This fluid also provides nourishment to the articular cartilage, which does not contain blood vessels. The ability of the bones to move smoothly against each other within the joint cavity, and the freedom of joint movement this provides, means that each synovial joint is functionally classified as a diarthrosis.
Outside of their articulating surfaces, the bones are connected by ligaments, strong bands of fibrous connective tissue. These strengthen and support the joint by anchoring the bones together and preventing their separation. Ligaments allow for normal movements at a joint but limit the range of these motions, thus preventing excessive or abnormal joint movements. Ligaments are classified based on their relationship to the fibrous articular capsule. An extrinsic ligament is located outside of the articular capsule. An intrinsic ligament is located inside the articular capsule.
Additional support is provided by the muscles and their tendons that act across the joint at many synovial joints. A tendon is the dense connective tissue structure that attaches a muscle to bone. As forces acting on a joint increase, the body will automatically increase the overall strength of contraction of the muscles crossing that joint, allowing the muscle and its tendon to serve as a “dynamic ligament” to resist forces and support the joint. This type of indirect support by muscles is critical at the shoulder joint, for example, where the ligaments are relatively weak.
Additional Structures Associated with Synovial Joints
A few synovial joints of the body have a fibrocartilage structure located between the articulating bones. This is called an articular disc, which is generally small and oval-shaped, or a meniscus, which is larger and C-shaped. These structures can serve several functions, depending on the specific joint. In some places, an articular disc may act to strongly unite the bones of the joint to each other. Examples of this include the articular discs found at the sternoclavicular joint or between the distal ends of the radius and ulna bones. At other synovial joints, the disc can provide shock absorption and cushioning between the bones, which is the function of each meniscus within the knee joint. Finally, an articular disc can smooth the movements between the articulating bones, as seen at the temporomandibular joint. Some synovial joints also have a fat pad, which can serve as a cushion between the bones.
Additional structures located outside of a synovial joint serve to prevent friction between the bones of the joint and the overlying muscle tendons or skin. A bursa (plural = bursae) is a thin connective tissue sac filled with lubricating liquid. They are located in regions where skin, ligaments, muscles, or muscle tendons can rub against each other, usually near a body joint. Bursae reduce friction by separating the adjacent structures, preventing them from rubbing directly against each other. Bursae are classified by their location. A subcutaneous bursa is located between the skin and an underlying bone. It allows the skin to move smoothly over the bone. Examples include the prepatellar bursa located over the kneecap and the olecranon bursa at the tip of the elbow. A submuscular bursa is found between a muscle and an underlying bone or between adjacent muscles. These prevent the rubbing of the muscle during movements. A large submuscular bursa, the trochanteric bursa, is found at the lateral hip, between the greater trochanter of the femur and the overlying gluteus maximus muscle. A subtendinous bursa is found between a tendon and a bone. Examples include the subacromial bursa that protects the tendon of the shoulder muscle as it passes under the acromion of the scapula and the suprapatellar bursa that separates the tendon of the large anterior thigh muscle from the distal femur just above the knee.
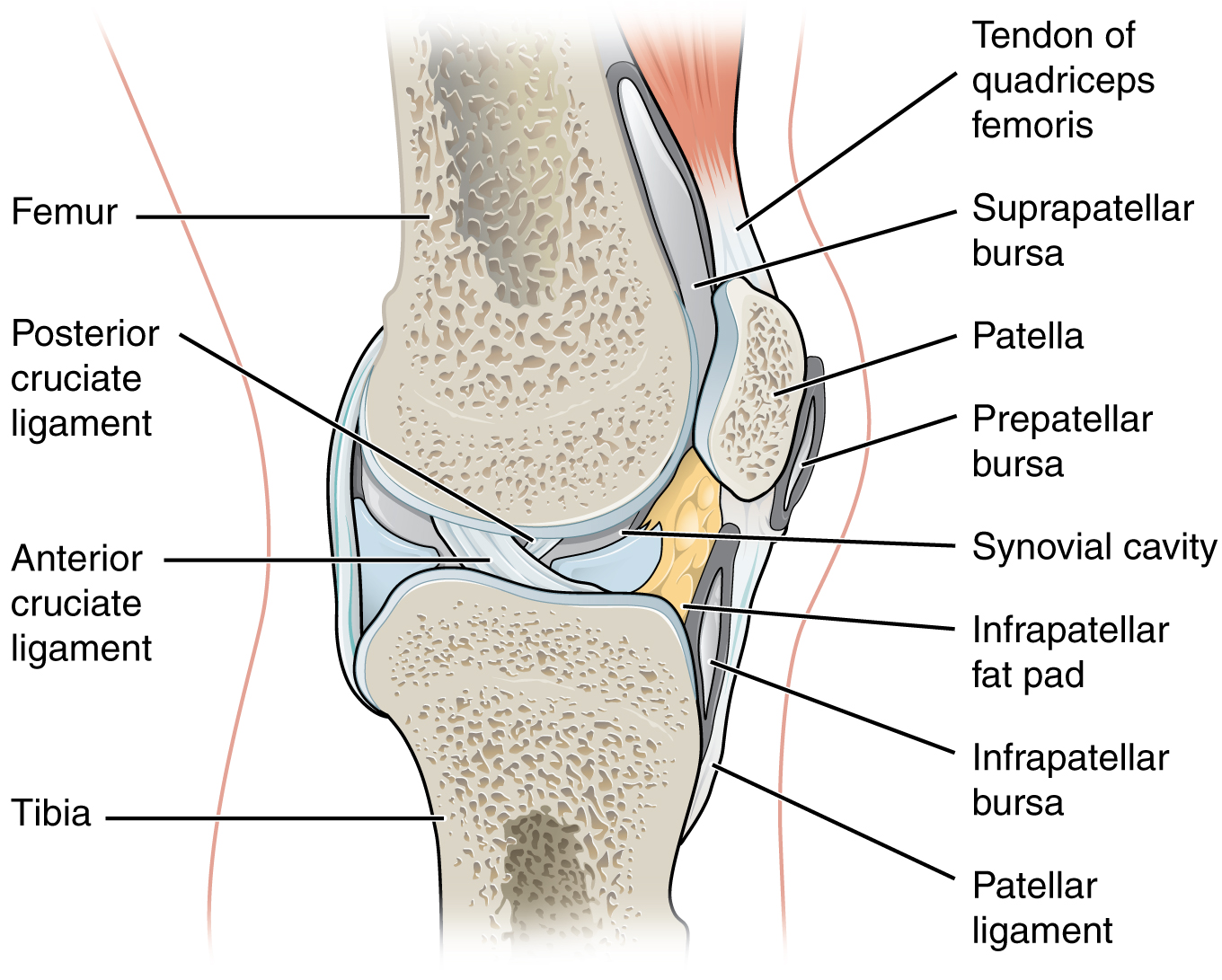
A tendon sheath is similar in structure to a bursa but smaller. It is a connective tissue sac surrounding a muscle tendon at places where the tendon crosses a joint. It contains a lubricating fluid that allows for smooth motions of the tendon during muscle contraction and joint movements. Bursitis is the inflammation of a bursa near a joint. This will cause pain, swelling, or tenderness of the bursa and surrounding area and result in joint stiffness. Bursitis is most commonly associated with the bursae found at or near the shoulder, hip, knee, or elbow joints.
Types of Synovial Joints
Synovial joints are subdivided based on the shapes of the articulating surfaces of the bones that form each joint. The six types of synovial joints are pivot, hinge, condyloid, saddle, plane, and ball-and socket-joints.
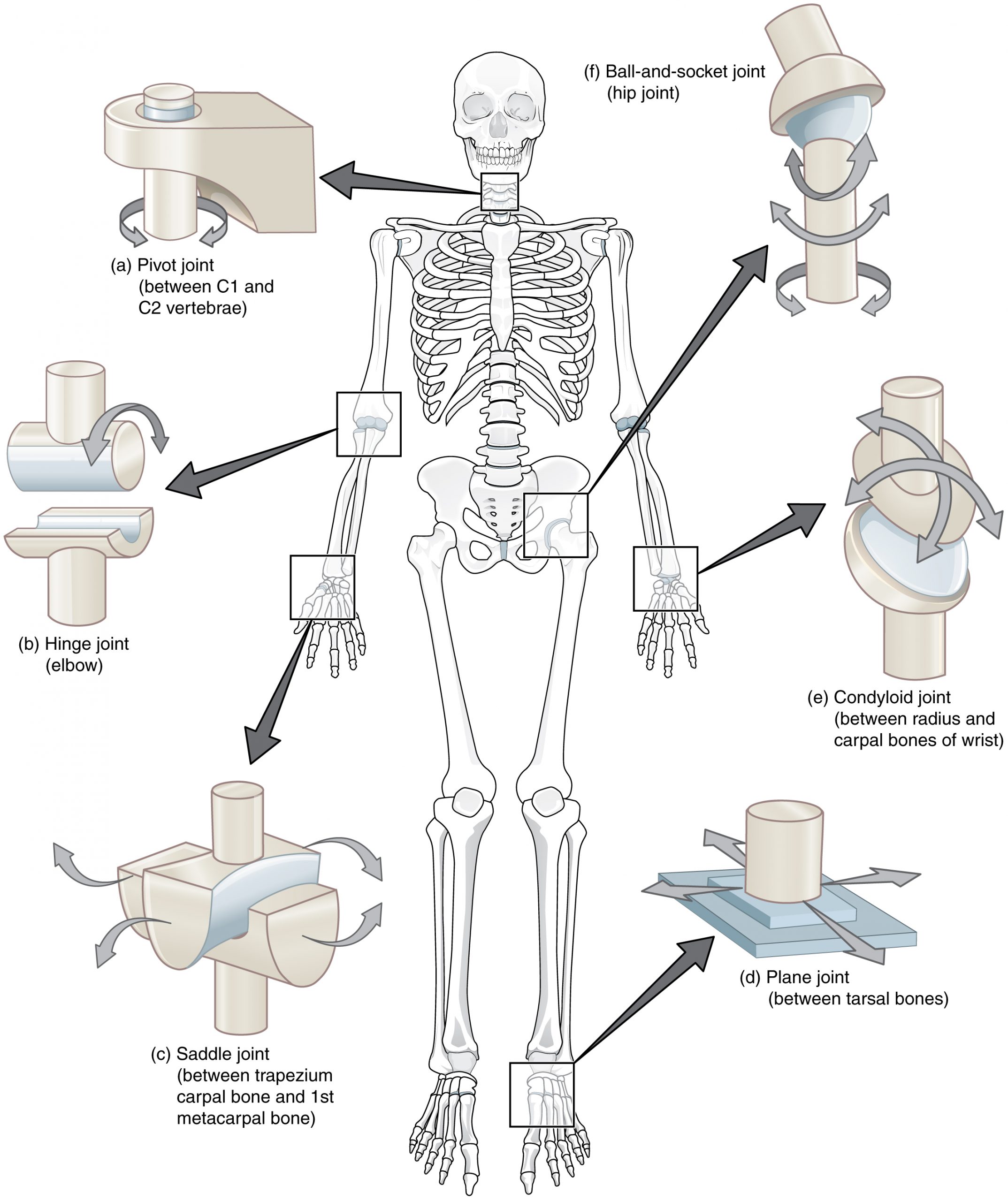
Pivot Joint
At a pivot joint, a rounded portion of a bone is enclosed within a ring formed partially by the articulation with another bone and partially by a ligament. The bone rotates within this ring. Since the rotation is around a single axis, pivot joints are functionally classified as a uniaxial diarthrosis type of joint. An example of a pivot joint is the atlantoaxial joint, found between the C1 (atlas) and C2 (axis) vertebrae. Here, the upward projecting dens of the axis articulates with the inner aspect of the atlas, where it is held in place by a ligament. Rotation at this joint allows you to turn your head from side to side. A second pivot joint is found at the proximal radioulnar joint. Here, the head of the radius is largely encircled by a ligament that holds it in place as it articulates with the radial notch of the ulna. Rotation of the radius allows for forearm movements.
Hinge Joint
In a hinge joint, the convex end of one bone articulates with the adjoining bone’s concave end. This type of joint allows flexion and extension motions along a single axis, and thus hinge joints are functionally classified as uniaxial joints. A good example is the elbow joint, with the articulation between the trochlea of the humerus and the trochlear notch of the ulna. Other hinge joints of the body include the knee, ankle, and interphalangeal joints between the phalanx bones of the fingers and toes.
Condyloid Joint
At a condyloid joint (ellipsoid joint), the shallow depression at the end of one bone articulates with a rounded structure from an adjacent bone or bones. The knuckle (metacarpophalangeal) joints of the hand between the distal end of a metacarpal bone and the proximal phalanx bone are condyloid joints. Another example is the radiocarpal joint of the wrist, between the shallow depression at the distal end of the radius bone and the rounded scaphoid, lunate, and triquetrum carpal bones. In this case, the articulation area has a more oval (elliptical) shape. Functionally, condyloid joints are biaxial joints that allow for two planes of movement. One movement involves the bending and straightening of the fingers or the anterior-posterior movements of the hand. The second movement is a side-to-side movement, which allows you to spread your fingers apart and bring them together or to move your hand in a medial-going or lateral-going direction.
Saddle Joint
At a saddle joint, both of the articulating surfaces for the bones have a saddle shape, which is concave in one direction and convex in the other. This allows the two bones to fit together like a rider sitting on a saddle. Saddle joints are functionally classified as biaxial joints. The primary example is the first carpometacarpal joint, between the trapezium (a carpal bone) and the first metacarpal bone at the base of the thumb. This joint provides the thumb the ability to move away from the palm of the hand along two planes. Thus, the thumb can move within the same plane as the palm of the hand or jut out anteriorly, perpendicular to the palm. This movement of the first carpometacarpal joint is what gives humans their distinctive “opposable” thumbs. The sternoclavicular joint is also classified as a saddle joint.
Plane Joint
At a plane joint (gliding joint), the articulating surfaces of the bones are flat or slightly curved and of approximately the same size, which allows the bones to slide against each other. Plane joints are non-axial. The motion at this type of joint is usually small and tightly constrained by surrounding ligaments. Based only on their shape, plane joints can allow gliding. Plane joints are found between the carpal bones (intercarpal joints) of the wrist or tarsal bones (intertarsal joints) of the foot, between the clavicle and acromion of the scapula (acromioclavicular joint), and between the superior and inferior articular processes of adjacent vertebrae (zygapophysial joints).
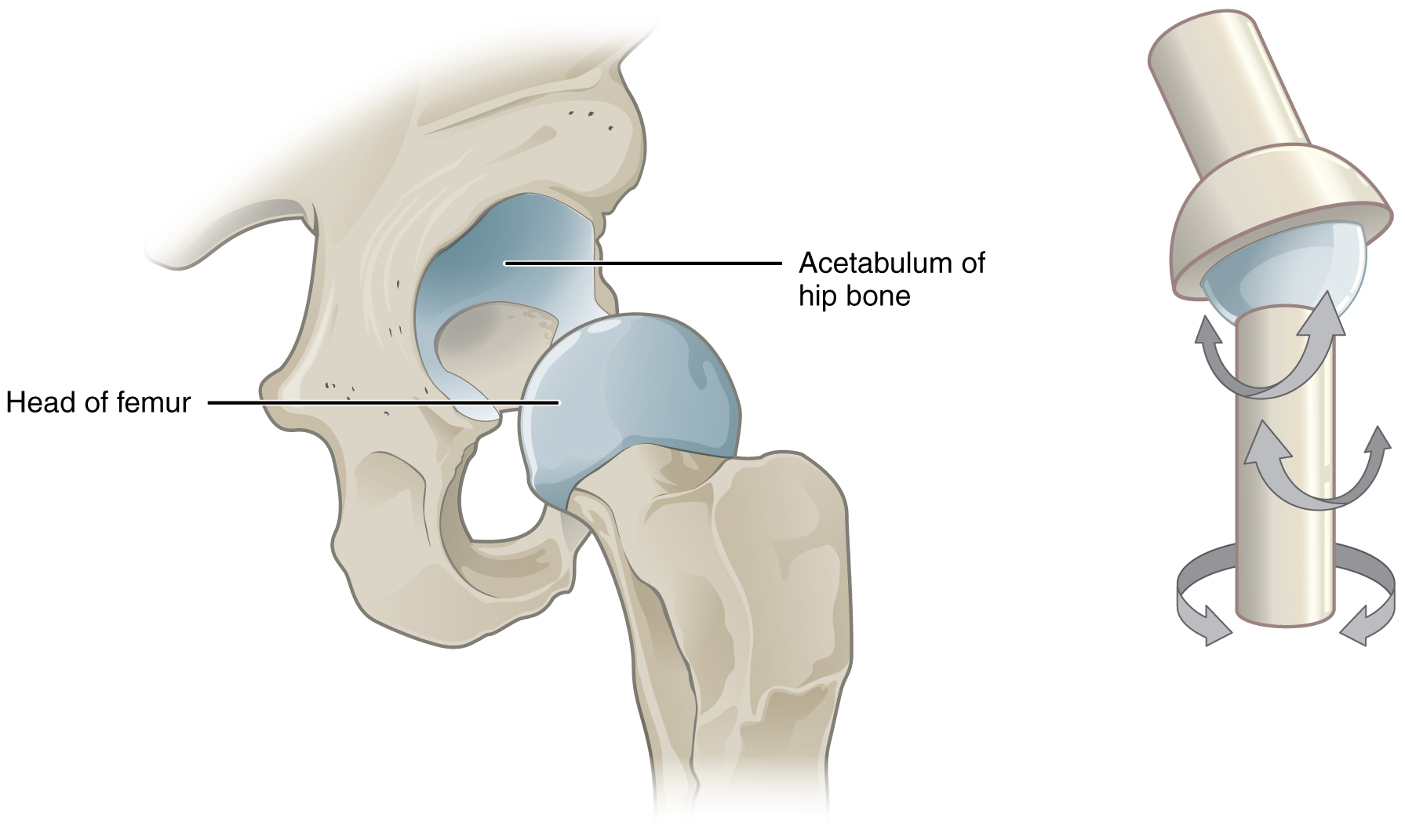
Ball-and-Socket Joint
The joint with the greatest range of motion is the ball-and-socket joint. At these joints, the rounded head of one bone (the ball) fits into the concave articulation (the socket) of the adjacent bone. The hip joint and the glenohumeral (shoulder) joint are the only ball-and-socket joints of the body. At the hip joint, the head of the femur articulates with the acetabulum of the hip bone, and at the shoulder joint, the head of the humerus articulates with the glenoid cavity of the scapula.
Ball-and-socket joints are classified functionally as multiaxial joints. The femur and the humerus can move in both anterior-posterior and medial-lateral directions, and they can also rotate around their long axis. The shallow socket formed by the glenoid cavity allows the shoulder joint an extensive range of motion. In contrast, the deep socket of the acetabulum and the strong supporting ligaments of the hip joint serve to constrain movements of the femur, reflecting the need for stability and weight-bearing ability at the hip.
Movements of the Body
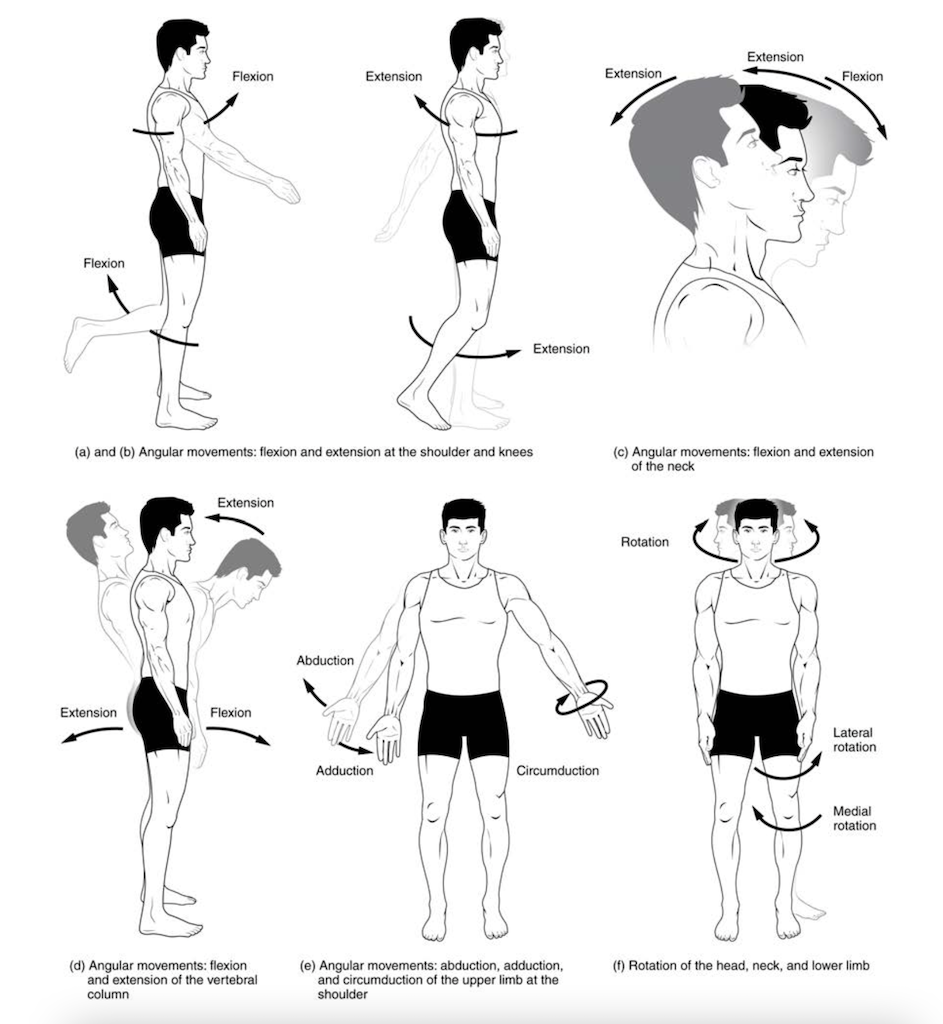
Flexion and Extension
Flexion and extension are movements within the sagittal plane and involve anterior or posterior movements of the body or limbs. For the vertebral column, flexion (anterior flexion) is an anterior (forward) bending of the neck or body, while extension involves a posterior-directed motion, such as straightening from a flexed position or bending backward. Lateral flexion is the bending of the neck or body toward the right or left side. These movements of the vertebral column involve both the symphysis joint formed by each intervertebral disc, as well as the plane type of synovial joint formed between the inferior articular processes of one vertebra and the superior articular processes of the next lower vertebra.
In the limbs, flexion decreases the angle between the bones (bending of the joint), while extension increases the angle and straightens the joint. For the upper limb, all anterior-going motions are flexion, and all posterior-going motions are extension. These include anterior-posterior movements of the arm at the shoulder, the forearm at the elbow, the hand at the wrist, and the fingers at the metacarpophalangeal and interphalangeal joints. For the thumb, extension moves the thumb away from the palm of the hand, within the same plane as the palm, while flexion brings the thumb back against the index finger or into the palm. These motions take place at the first carpometacarpal joint. In the lower limb, bringing the thigh forward and upward is flexion at the hip joint, while any posterior-going motion of the thigh is extension. Note that extension of the thigh beyond the anatomical (standing) position is greatly limited by the ligaments that support the hip joint. Knee flexion is the bending of the knee to bring the foot toward the posterior thigh, and extension is the straightening of the knee. Flexion and extension movements are seen at the hinge, condyloid, saddle, and ball-and-socket joints of the limbs.
Hyperextension is the abnormal or excessive extension of a joint beyond its normal range of motion, thus resulting in injury. Similarly, hyperflexion is excessive flexion at a joint. Hyperextension injuries are common at hinge joints such as the knee or elbow. In cases of “whiplash,” in which the head is suddenly moved backward and then forward, a patient may experience both hyperextension and hyperflexion of the cervical region.
Abduction and Adduction
Abduction and adduction motions occur within the coronal plane and involve medial-lateral motions of the limbs, fingers, toes, or thumb. Abduction moves the limb laterally away from the midline of the body, while adduction is the opposing movement that brings the limb toward the body or across the midline. For example, abduction is raising the arm at the shoulder joint, moving it laterally away from the body, while adduction brings the arm down to the side of the body. Similarly, abduction and adduction at the wrist moves the hand away from or toward the midline of the body. Spreading the fingers or toes apart is also abduction while bringing the fingers or toes together is adduction. For the thumb, abduction is the anterior movement that brings the thumb to a 90° perpendicular position, pointing straight out from the palm. Adduction moves the thumb back to the anatomical position, next to the index finger. Abduction and adduction movements are seen at condyloid, saddle, and ball-and-socket joints.
Circumduction
Circumduction is the movement of a body region in a circular manner, in which one end of the body region being moved stays relatively stationary while the other end describes a circle. It involves the sequential combination of flexion, adduction, extension, and abduction at a joint. This type of motion is found at biaxial condyloid and saddle joints and multiaxial ball-and-socket joints.
Rotation
Rotation can occur within the vertebral column, at a pivot joint, or a ball-and-socket joint. Rotation of the neck or body is the twisting movement produced by the summation of the small rotational movements available between adjacent vertebrae. At a pivot joint, one bone rotates about another bone. This is a uniaxial joint, and thus rotation is the only motion allowed at a pivot joint. For example, at the atlantoaxial joint, the first cervical (C1) vertebra (atlas) rotates around the dens, the upward projection from the second cervical (C2) vertebra (axis). This allows the head to rotate from side to side as when shaking the head “no.” The proximal radioulnar joint is a pivot joint formed by the head of the radius and its articulation with the ulna. This joint allows for the radius to rotate along its length during pronation and supination movements of the forearm.
Rotation can also occur at the ball-and-socket joints of the shoulder and hip. Here, the humerus and femur rotate around their long axis, which moves the anterior surface of the arm or thigh either toward or away from the midline of the body. The movement that brings the anterior surface of the limb toward the midline of the body is called medial (internal) rotation. Conversely, rotation of the limb so that the anterior surface moves away from the midline is lateral (external) rotation. Be sure to distinguish medial and lateral rotation, which can only occur at the multiaxial shoulder and hip joints, from circumduction, which can occur at either biaxial or multiaxial joints.
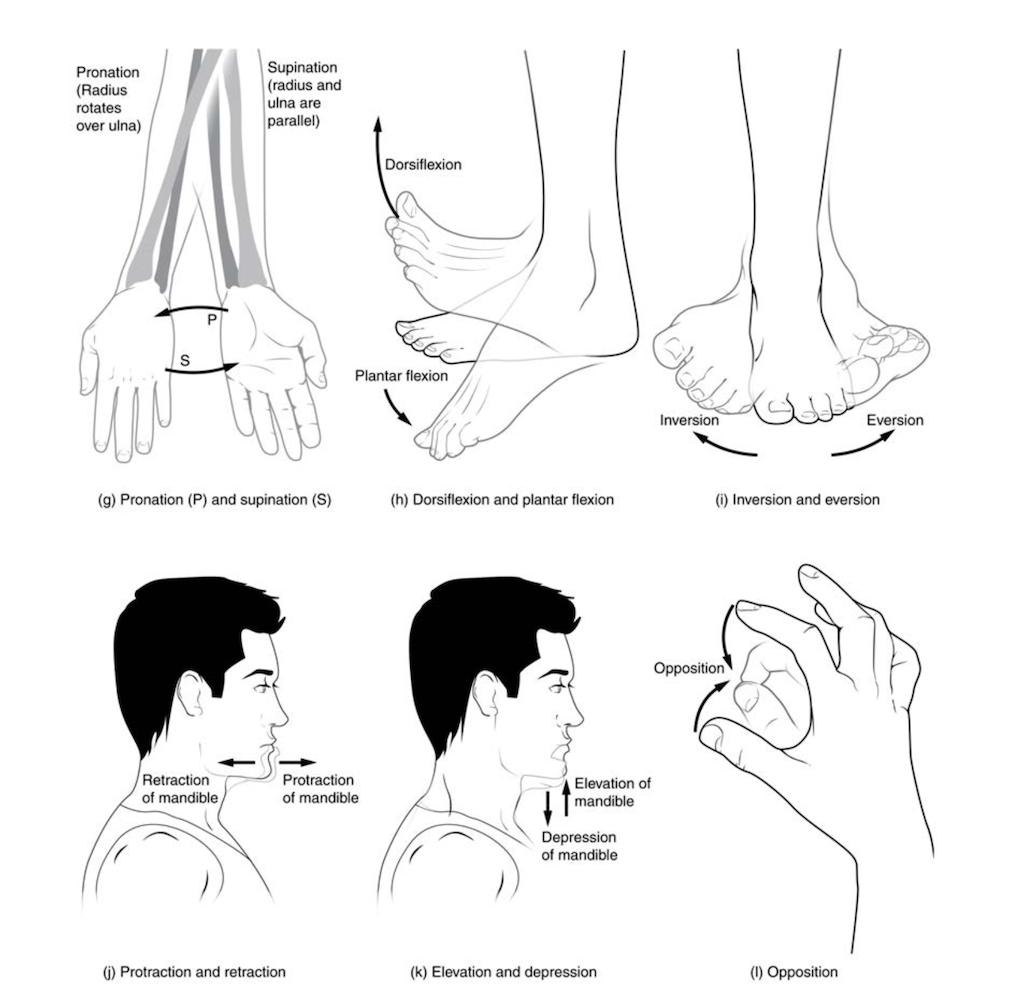
Supination and Pronation
Supination and pronation are movements of the forearm. In the anatomical position, the upper limb is held next to the body, with the palm facing forward. This is the supinated position of the forearm. In this position, the radius and ulna are parallel to each other. When the palm of the hand faces backward, the forearm is in the pronated position, and the radius and ulna form an X-shape.
Supination and pronation are the movements of the forearm that go between these two positions. Pronation is the motion that moves the forearm from the supinated (anatomical) position to the pronated (palm backward) position. This motion is produced by rotation of the radius at the proximal radioulnar joint, accompanied by movement of the radius at the distal radioulnar joint. The proximal radioulnar joint is a pivot joint that allows for the rotation of the head of the radius. Because of the slight curvature of the shaft of the radius, this rotation causes the distal end of the radius to cross over the distal ulna at the distal radioulnar joint. This crossing over brings the radius and ulna into an X-shape position. Supination is the opposite motion, in which rotation of the radius returns the bones to their parallel positions and moves the palm to the anterior facing (supinated) position. It helps to remember that supination is the motion you use when scooping up soup with a spoon.
Dorsiflexion and Plantar Flexion
Dorsiflexion and plantar flexion are movements at the ankle joint, which is a hinge joint. Lifting the front of the foot so that the top of the foot moves toward the anterior leg is dorsiflexion while lifting the heel of the foot from the ground or pointing the toes downward is plantar flexion. These are the only movements available at the ankle joint.
Inversion and Eversion
Inversion and eversion are complex movements involving the multiple plane joints among the tarsal bones of the posterior foot (intertarsal joints) and are thus not motions at the ankle joint. Inversion is the turning of the foot to angle the bottom of the foot toward the midline, while eversion turns the bottom of the foot away from the midline. The foot has a greater range of inversion than eversion motion. These are important motions that help stabilize the foot when walking or running on an uneven surface and aid in the quick side-to-side changes in direction used during active sports such as basketball, racquetball, or soccer.
Protraction and Retraction
Protraction and retraction are anterior-posterior movements of the scapula or mandible. Protraction of the scapula occurs when the shoulder is moved forward, as when pushing against something or throwing a ball. Retraction is the opposite motion, with the scapula being pulled posteriorly and medially toward the vertebral column. For the mandible, protraction occurs when the lower jaw is pushed forward to stick out the chin, while retraction pulls the lower jaw backward.
Depression and Elevation
Depression and elevation are downward and upward movements of the scapula or mandible. The upward movement of the scapula and shoulder is elevation, while a downward movement is depression. These movements are used to shrug your shoulders. Similarly, elevation of the mandible is the upward movement of the lower jaw used to close the mouth or bite on something, and depression is the downward movement that produces the opening of the mouth.
Excursion
Excursion is the side to side movement of the mandible. Lateral excursion moves the mandible away from the midline, toward either the right or left side. Medial excursion returns the mandible to its resting position at the midline.
Superior Rotation and Inferior Rotation
Superior and inferior rotation are movements of the scapula and are defined by the direction of movement of the glenoid cavity. These motions involve rotation of the scapula around a point inferior to the scapular spine and are produced by combinations of muscles acting on the scapula. During superior rotation, the glenoid cavity moves upward as the medial end of the scapular spine moves downward. This is a very important motion that contributes to upper limb abduction. Without superior rotation of the scapula, the greater tubercle of the humerus would hit the acromion of the scapula, thus preventing any abduction of the arm above shoulder height. Superior rotation of the scapula is thus required for full abduction of the upper limb. Superior rotation is also used without arm abduction when carrying a heavy load with your hand or on your shoulder. You can feel this rotation when you pick up a load, such as a heavy book bag, and carry it on only one shoulder. To increase its weight-bearing support for the bag, the shoulder lifts as the scapula superiorly rotates. Inferior rotation occurs during limb adduction and involves the downward motion of the glenoid cavity with upward movement of the medial end of the scapular spine.
Opposition and Reposition
Opposition is the thumb movement that brings the tip of the thumb in contact with the tip of a finger. This movement is produced at the first carpometacarpal joint, a saddle joint formed between the trapezium carpal bone and the first metacarpal bone. Thumb opposition is produced by a combination of flexion and abduction of the thumb at this joint. Returning the thumb to its anatomical position next to the index finger is called reposition.
| Movements of the Joints | ||
|---|---|---|
| Type of Joint | Movement | Example |
| Pivot | Uniaxial joint; allows rotational movement | Atlantoaxial joint (C1–C2 vertebrae articulation); proximal radioulnar joint |
| Hinge | Uniaxial joint; allows flexion/extension movements | Knee; elbow; ankle; interphalangeal joints of fingers and toes |
| Condyloid | Biaxial joint; allows flexion/extension, abduction/adduction, and circumduction movements | Metacarpophalangeal (knuckle) joints of fingers; radiocarpal joint of wrist; metatarsophalangeal joints for toes |
| Saddle | Biaxial joint; allows flexion/extension, abduction/adduction, and circumduction movements | First carpometacarpal joint of the thumb; sternoclavicular joint |
| Plane | Nonaxial joint; allows inversion and eversion of foot, or flexion, extension, and lateral flexion of the vertebral column | Intertarsal joints of foot; superior-inferior articular process articulations between vertebrae |
| Ball-and-socket | Multiaxial joint; allows flexion/extension, abduction/adduction, circumduction, and medial/lateral rotation movements | Shoulder and hip joints |
Aging and Joints
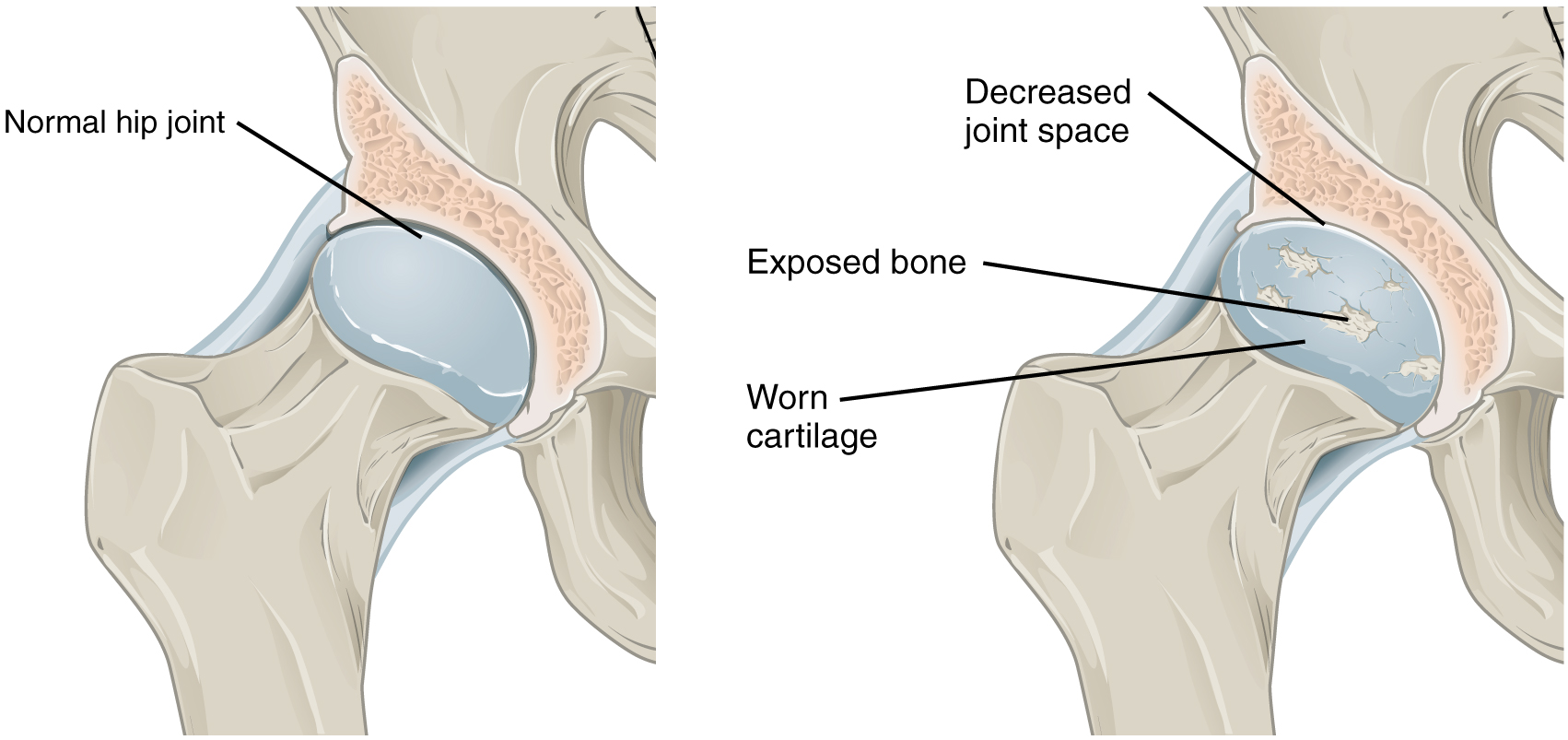
Arthritis is a common disorder of synovial joints that involves inflammation of the joint. This often results in significant joint pain, along with swelling, stiffness, and reduced joint mobility. There are more than 100 different forms of arthritis. Arthritis may arise from aging, damage to the articular cartilage, autoimmune diseases, bacterial or viral infections, or unknown (probably genetic) causes.
The most common type of arthritis is osteoarthritis, which is associated with aging and “wear and tear” of the articular cartilage. Risk factors that may lead to osteoarthritis later in life include injury to a joint; jobs that involve physical labor; sports with running, twisting, or throwing actions; and being overweight. These factors put stress on the articular cartilage that covers the surfaces of bones at synovial joints, causing the cartilage to gradually become thinner. As the articular cartilage layer wears down, more pressure is placed on the bones. The joint responds by increasing production of the lubricating synovial fluid, but this can lead to swelling of the joint cavity, causing pain and joint stiffness as the articular capsule is stretched. The bone tissue underlying the damaged articular cartilage also responds by thickening, producing irregularities and causing the articulating surface of the bone to become rough or bumpy. Joint movement then results in pain and inflammation. In its early stages, symptoms of osteoarthritis may be reduced by mild activity that “warms up” the joint, but the symptoms may worsen following exercise. In individuals with more advanced osteoarthritis, the affected joints can become more painful and therefore are difficult to use effectively, resulting in increased immobility. There is no cure for osteoarthritis, but several treatments can help alleviate the pain. Treatments may include lifestyle changes, such as weight loss and low-impact exercise, and over-the-counter or prescription medications that help alleviate pain and inflammation. For severe cases, joint replacement surgery (arthroplasty) may be required.